Michael J. Yaremchuk, MD, FACS
4.1 Background
The need to immobilize fractured facial bones in anatomic apposition to effect healing has long been known. Hippocrates described1 the closed reduction and external stabilization of mandibular fractures with the use of “bridal wire — a wire wrapped around two teeth on either side of the fracture.” Open techniques of fracture reduction and immobilization were introduced in the 19th century. Gurdon Buck, in 1847, used interfragmentary wires to treat a fractured mandible.2 Max Schede, in 1888, first described the use of steel plates and screws to treat mandible fractures.3 It was not until corrosion-resistant materials were developed, such as stainless steel and the alloy Vitallium, that internal fixation for the facial skeleton became more common.4
Wire osteosynthesis has largely been replaced by more rigid fixation constructs that use miniaturized plates and screws. Plate-and-screw fixation allows skeletal positioning in three dimensions, often with sufficient stability to eliminate or reduce the need for jaw immobilization when occlusal bearing-bone segments are involved. This “rigid internal fixation” has become the gold standard for stabilization of the facial skeleton.5
4.2 Bone Healing
Healing of bone fractured by trauma or osteotomy requires stable apposition of the fracture surfaces. Gross movement or significant gaps between fractured bone segments lead to nonunion and fibrocartilaginous tissue formation. Bone heals by the following two mechanisms, which depend on the degree of bone-end apposition and movement.
4.2.1 Primary bone healing
When fracture segments are closely apposed (usually compressed) and sufficiently immobilized to eliminate any motion, the bone healing process is termed primary. Primary bone healing is characterized by the direct formation of bone. Under these conditions, the union of bone segments occurs without a preceding intermediary tissue type (i.e., a callus).
4.2.2 Secondary bone healing
A hematoma develops between the two bone segments after a fracture. The hematoma is then sequentially replaced by fibrous tissue, cartilage (in endochondral but not membranous bone), woven bone, and lamellar bone. As the tissues in the callus mature, stiffness is increased and strain is reduced across the bone segments. This process decreases motion at the fracture site. The result allows for bone formation and subsequent bone healing. This process is called secondary bone healing. It is the usual process occurring after facial skeletal rearrangement or repair, either because it is necessary to maintain small gaps between bone segments to create or maintain certain 3-dimensional relationships or because the scale of the fixation device required to eliminate any micromotion would be prohibitive.
4.3 Skeletal Reduction and Immobilization
Similar to long-bone fractures, facial bone fractures are treated by one of the two basic methods: closed reduction and external stabilization (or splinting), or open reduction and internal fixation.
4.3.1 Closed reduction and external stabilization
The three surgical procedures commonly used by craniofacial surgeons for closed reduction and external stabilization are maxillomandibular fixation (MMF), suspension wires plus MMF, and external fixators. Section 4.3.1.1 will discuss those procedures in detail.
4.3.1.1 Maxillomandibular fixation
MMF can be an effective way to reduce and immobilize certain simple fractures of the mandible. MMF requires an external device (Erich arch bars) to be applied to the upper and lower dental arches by wiring them to the teeth. Application of the arch bar to the lower teeth helps reduce tooth-bearing fracture segments. Occluding the fractured lower dental arch to the intact upper dental arch refines fracture reduction. Wiring the upper arch bar to the lower arch bar helps immobilize the fracture. Hence, MMF can be both a closed means of fracture reduction and a means of immobilization. By restoring occlusion, MMF is also used in more complex mandible fractures, or mid-face fractures, as a guide to accurate reduction (Figure 4.1).
MMF screws may be a time-saving alternative to Erich arch bars. MMF screws are self-drilling titanium screws designed to hold wires. They are inserted into the upper and lower dental arches. They may be used to maintain dental occlusion as a guide to mid-face fracture alignment when the upper and lower dental arches are intact (Figure 4.2).

Figure 4.1. MMF with Erich arch bars.

Figure 4.2. Maxillomandibular screws used for MMF.
4.3.1.2 Suspension wires and MMF
MMF can restore proper occlusal relationships between the upper and lower tooth-bearing segments, but it does not ensure the proper positioning of the teeth in relation to the rest of the facial skeleton.
Until the 1980s, midface fractures were reduced by restoring the occlusion with MMF and immobilizing the fracture using suspension wires. Wires were dropped down from the orbit, zygoma, or stable bone structures adjacent to or associated with the cranial base to suspend the occluded tooth-bearing segment. In certain cases, head frames were used to create a stable base for the suspension wires. Unfortunately, suspensory wires create only a vertical vector, which precludes control of sagittal positioning of the occluded segment — a major limitation. Suspension-wire tightening forces the midface toward the base of the cranium, resulting in a vertical foreshortening and retrusion of the midface (Figure 4.3).6
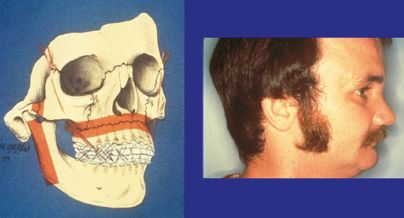
Figure 4.3. An example of subcondylar and Le Fort fractures treated with suspensory wires (left) and MMF causing vertical foreshortening and retrusion of the face (right). Reprinted with permission from Lippincott Williams & Wilkins (Manson PN, et al. Midface fractures: advantages of immediate extended open reduction and bone grafting. Plast Reconstr Surg 1985;76:1–10).
4.3.1.3 External fixators
External fixation is a method by which the bone segments are held in place by percutaneous wires attached to an external frame (Figure 4.4). In the past, it was frequently used to treat complex Le Fort fractures in an attempt to obtain 3-dimensional fracture positioning. Today, it is most often used in patients who have severe soft tissue injury, contamination, severe infection, or comminuted fractures of the mandible, often with bone loss. In addition, external fixators are practical for treating fractures in patients who are medically too unstable for major surgical procedures. They are usually used to provide temporary fixation and are replaced with internal fixation when the soft tissue envelope is repaired, infection is controlled, or the patient is medically stable. In some situations, external fixators are left in place until the fracture heals.
4.3.2 Open reduction and internal fixation
Open reduction and internal fixation techniques involve direct exposure of bone segments, their realignment, and immobilization. Surgical approaches have been borrowed from aesthetic and craniofacial surgery. They include the use of bicoronal, intraoral, and periorbital incisions. All fractures are exposed by surgical dissection in a subperiosteal plane.

Figure 4.4. Clinical example of external fixator used to treat a severely comminuted mandibular fracture.
4.3.2.1 Interfragmentary wiring
After fracture exposure and reduction, bone immobilization can be obtained by passing wire (usually 28 or 30 gauge) through drill holes placed on either side of the fracture. The ends of the wire are twisted to one another until a stable construct is obtained. Interfragmentary wiring can provide effective immobilization for simple fractures. However, the uniplanar nature of interfragmentary wiring limits its efficacy when immobilization needs become more complex. Interfragmentary wiring becomes less effective in restoring anatomy as the number of fracture segments or the 3-dimensionality of the construct to be restored increases, or both. The limitation of interfragmentary wiring is demonstrated in Figure 4.5.
With the advent of plate-and-screw fixation techniques that allow stable 3-dimensional reconstruction, interfragmentary wiring is most often used now for simple fractures or to help in temporary alignment of fractured segments before rigid fixation.
4.3.2.2 Plate-and-screw fixation
The use of miniaturized plates and screws, commonly referred to as rigid fixation, has revolutionized surgery of the craniofacial skeleton. The rigidity provided by these devices limits or eliminates motion between fracture segments, hence optimizing conditions for bone healing. The ability to bend plates in desired shapes allows precise, 3-dimensional bone positioning and therefore reconstruction (Figure 4.5).
For bones to heal in the desired position, the fixation devices must be strong enough to neutralize the force exerted by gravity, soft tissue deforming forces, or the muscles of mastication occurring at the fracture site. Since these distracting forces vary in different areas of the craniofacial skeleton, the design and scale of plates and screws vary accordingly. In general, larger, more rigid systems are used to counteract the muscles of mastication, and systems of lesser scale are used to counteract soft tissue deforming forces.
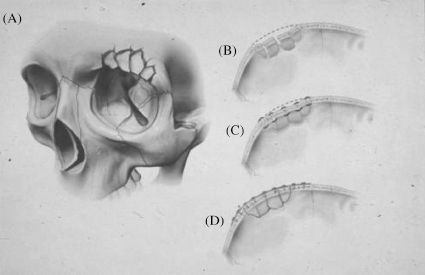
Figure 4.5. The difference in 3-dimensional result between wire and plate-and-screw fixation. (A) Comminuted supraorbital rim fracture. (B) Axial view shows loss of curvature. (C) Interfragmentary wiring collapses arch. The collapse is exaggerated by the inevitable bone loss occurring at the fracture sites. With increasing comminution, interfragmentary stabilization results in a uniplanar construct. (D) Plate-and-screw fixation allows restoration of preinjury curvature. The plate is bent to the desired shape, and the fracture segments are attached to it with screws.
Plate-and-screw fixation techniques can provide desired skeletal configurations only if these devices are adapted to properly positioned bone segments. It is crucial to contour plates properly to the underlying bone since bone fragments adapt to the shape of the plate. Improper plate bending will result in bone malalignment (Figure 4.6). A malleable template will help to guide plate bending.
In the treatment of maxillary and mandibular fractures, it is essential to restore pretraumatic dental occlusion with MMF before reduction and fixation of the fractures.
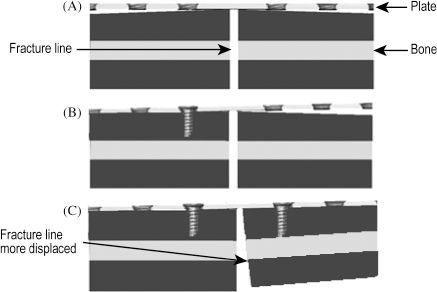
Figure 4.6. (A) The plate is not perfectly contoured to the bone. (B and C) As the screws are tightened, the bone adapts to the shape of the plate and the fracture becomes displaced.
In the treatment of facial fractures, plates should be placed in areas of adequately robust bone (i.e., buttresses).7 In the face, there are four paired vertical buttresses; from anteromedial to posterolateral, they are the nasomaxillary, zygomaticomaxillary, pterygomaxillary, and mandibular ramus buttresses.6
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


