The aim of this article was to relate the clinical case of an HIV-positive orthodontic patient who reported that her cheeks had been hurting since treatment began. We started with the data collected in anamnesis and by contact with the patient’s physician, and a diagnosis of facial lipodystrophy as a result of the use of retroviral drugs was reached. The patient was referred to a dermatologist for treatment of the facial lipodystrophy.
Human immunodeficiency virus (HIV), or acquired immunodeficiency syndrome (AIDS), was described in 1981 in the United States. Since the appearance of the first cases, important alterations in the demographic and epidemiologic characteristics of the disease have been observed. Initially, it seemed to be restricted to specific populations or geographic areas, but it soon spread to other regions in the world and became pandemic.
When the epidemic began, the main paths of transmission of the disease were homosexual relationships and the use of endovenous drugs. People with these behaviors were called “risk groups.” At present, increased transmission through heterosexual relationships has been observed and today, there are no longer any “risk groups.”
Highly active antiretroviral therapies containing the protease inhibitor class of drugs promoted important and sustained suppression of viral replication, raising the survival rate and quality of life of seropositive patients. Nevertheless, antiretroviral therapy is accompanied by metabolic alterations, such as dyslipidemia, insulin resistance, hyperglycemia, and redistribution of body fat, risk factors for cardiovascular disease. This set of alterations is known as the lipodystrophic syndrome of HIV.
Estimates of the prevalence of the lipodystrophic syndrome of HIV are not precise. Mauss et al found a prevalence of 34% in 221 German HIV-positive patients having antiretroviral therapy for more than 3 years.
The aim of this study was to relate a clinical case of an HIV-positive orthodontic patient who was being treated with retroviral medication and developed facial lipodystrophy.
Case report
A 34-year-old woman came to the orthodontic consulting room with a complaint that, after 11 months of orthodontic treatment with another clinician, her cheeks had become became flaccid. The patient was seeking a professional opinion to determine whether the treatment she was undergoing, including fixed appliance therapy to correct a Class I malocclusion, had any influence on the reduction of fat in her cheeks. She had been diagnosed 1 year earlier as having AIDS and began drug therapy with retroviral medication at that time.
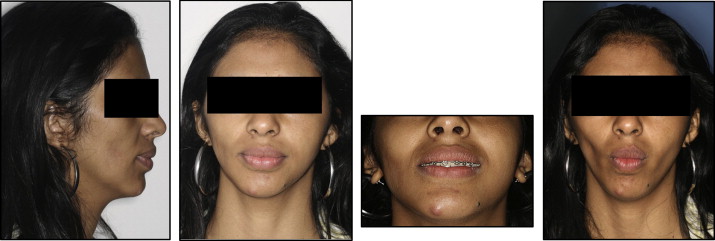
The extraoral clinical examination showed a reduction of fat in the region of the cheeks, particularly on the right side ( Fig ). Palpation of the cheeks confirmed that the adipose tissue of the cheek was diminished, particularly on the right. For better visualization, we asked the patient to perform the function of suction.
Starting with the data collected in anamnesis and the clinical examination, we contacted the dermatologist and the infectologist to evaluate the possible interactions of AIDS and the medications on the reduction of fat in the cheeks. The diagnosis reached was facial lipodystrophy as a result of the retroviral medications.
Discussion
The purpose of this article was to relate a clinical case of an orthodontic patient who, 1 year after the start of treatment, noted that a process of reduction of her cheeks had occurred. Although lipodystrophy is not known to result from orthodontic movements, if it occurs during orthodontic treatment, a patient might assume that they are related.
Lipodystrophic syndrome in patients treated for AIDS is a progressive condition; the severity appears to be directly proportional to the time of treatment with antiretroviral medications. The progression of lipodystrophy in this patient is strictly related to the time of retroviral medication use.
Lipodystrophy can be clinically classified into 3 categories: (1) lipoatrophy, characterized by the reduction of fat in the peripheral regions, such as the arms, legs, face, and buttocks, with relative muscular and venous prominence; (2) lipohypertrophy, characterized by the accumulation of fat in the abdominal region, presence of dorsal gibbsite, gynecomasty, and increased size of the breasts in women; and (3) mixed form, characterized by the association of components of both forms. Our patient was in classification type 1, with only reduction of facial fat.
Because the causes of lipodystrophy are not sufficiently known, it has been difficult to delineate the attempts to treat it. Although diet and regular physical exercise are not definitive solutions for the effects of lipodystrophy, studies have pointed out that changes in dietary habits and the practice of physical activity are important to obtain some positive results. Such changes in lifestyle appear to help in maintaining weight and contribute to less accelerated progression of the metabolic alterations.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


