Introduction
An accurate assessment of face symmetry is necessary for the development of a dentofacial diagnosis in orthodontics, and an understanding of individual differences in perception of face symmetry between patients and providers is needed to facilitate successful treatment.
Methods
Orthodontists, general dentists, and control participants completed a series of tasks to assess symmetry. Judgments were made on pairs of upright faces (similar to the longitudinal assessment of photographic patient records), inverted faces, and dot patterns. Participants completed questionnaires regarding clinical practice, education level, and self-confidence ratings for symmetry assessment abilities.
Results
Orthodontists showed expertise compared with controls ( P <0.001), whereas dentists showed no advantage over controls. Orthodontists performed better than dentists, however, in only the most difficult face symmetry judgments ( P = 0.006). For both orthodontists and dentists, accuracy increased significantly when assessing symmetry in upright vs inverted faces ( t = 3.7, P = 0.001; t = 2.7, P = 0.02, respectively).
Conclusions
Orthodontists showed expertise in assessing face symmetry compared with both laypersons and general dentists, and they were more accurate when judging upright than inverted faces. When using accurate longitudinal photographic records to assess changing face symmetry, orthodontists are likely to be incorrect in less than 15% of cases, suggesting that assistance from some additional technology is infrequently needed for diagnosis.
Symmetry is an important biologically based determinant of facial attractiveness, and assessment of symmetry in a patient’s face is paramount to the development of a complete dentofacial diagnosis. In an era of modern orthodontics when the soft-tissue paradigm and patient perception often dictate the success of treatment outcomes, it is not acceptable for the orthodontist to simply identify problems and proceed with treatment. An understanding of individual differences in the perception of face symmetry across orthodontists, their patients, and other providers of dental care is needed to facilitate communication among these groups and to ensure optimal treatment results. To these ends, recent research has attempted to establish thresholds for the perception of a problem in face symmetry in various professional and nonprofessional groups.
Huisinga-Fischer et al asked participants to objectively compare asymmetry between subjects’ faces. Their results suggest that orthodontists and surgeons might judge face symmetry more accurately than other groups but leave room for alternative explanations because of the nature of the stimuli and the tasks. Specifically, the face stimuli they used had pathologic deviations from normal symmetry and normal proportions, and the participants were asked to rate how the faces differed in terms of deformity from normal rather than in symmetry explicitly. Accordingly, the role of symmetry in the participants’ judgments was unclear. Another study related to the perception of face symmetry suggested dental expertise, but the participants were asked to rate attractiveness rather than symmetry. Finally, a study using virtual 3-dimensional face stimuli suggested that whereas there are thresholds for the perception of an asymmetric nose or chin, orthodontists and oral surgeons showed no meaningful advantage in judging face symmetry compared with laypersons. None of these studies was designed to investigate expertise explicitly.
Of equal importance to the threshold for detection of a problem is an understanding of the orthodontist’s perceptual ability in general and in relation to the patient. Are orthodontists experts at assessing face symmetry? To date, the data are equivocal at best because studies have not been adequately designed to answer that question. If an orthodontist is better at judging face symmetry than the patient, then he or she can confidently help the patient to decide whether treatment is warranted. If the orthodontist is not better at assessing face symmetry, then treatment outcomes as viewed by the patient might not meet the patient’s goals. With the availability of 3-dimensional imaging of facial surfaces, which allows for the exact quantification of face symmetry, understanding perceptual differences might become increasingly relevant. If an orthodontist understands his or her abilities in relation to the patient, he or she might better be able to determine when such technology is needed to assist in diagnosis.
The aims of this study were to determine whether orthodontists possess expertise in assessing face symmetry and to explore the nature of this ability with the hope of informing clinical practice and patient communication. To accomplish these goals, we compared performance on symmetry judgment tasks across orthodontists, general dentists, and control participants with no training in face symmetry assessment.
Material and methods
This study was considered exempt from institutional board review by the Office of Human Research Ethics at the University of North Carolina at Chapel Hill and approved as an addition to a separate ongoing study by the institutional review board of Duke University, Durham, NC. Orthodontists (n = 31; 8 women; mean age, 43.5 years; SD, 15.8 years) were recruited from the University of North Carolina’s School of Dentistry, including residents in various stages of the 3-year program as well as full-time and part-time faculty members. The faculty participants reported an average of 27.4 years of clinical practice (SD, 12.5 years). General dentists were also recruited from the University of North Carolina’s School of Dentistry and included residents and faculty members (n = 12; 3 women; mean age, 53.1 years; SD, 13.2 years). Orthodontic residents, orthodontic faculty, and general dentists were all compensated $10 per hour for their time.
Control participants with no symmetry training were recruited from 2 sources: nonprofessional laypersons from Duke University (nonprofessionals) and Transportation Security Administration (TSA) officers employed at Raleigh-Durham International Airport in North Carolina. The nonprofessionals represented a diverse cross-section of the Duke University community and included undergraduate, graduate, and postdoctoral students as well as employees and general affiliates of the university. This group of laypersons, with exclusion based only on vision screening or failure to give consent, had no known special visual skills. The nonprofessionals (n = 23; 13 women; mean age, 20.9 years; SD, 4.5 years) were compensated with course credits or paid $10 per hour for their participation. The TSA officers represented a population known to have enhanced visual cognition abilities unrelated to face symmetry assessment. The TSA officers (n = 10; 2 women; mean age, 42.3 years; SD, 10.2 years) were not directly compensated because their data were collected during normal working hours as part of their employment. Participation in this study by the TSA officers was entirely confidential and voluntary. Two additional participants in the TSA group and 1 in the nonprofessional group had overall face accuracy scores that were 2 SD below the mean overall face accuracy score for all participants, and their data were excluded from all analyses. Exclusion of these data was carried out according to criteria established a priori to account for participants who might not make earnest judgments and instead just complete the tasks for the compensation provided. All participants had 20/20 vision or used corrective lenses at the time of data collection.
Data were acquired in 3 locations with identical protocols and environments: orthodontic resident, orthodontic faculty, and general dentist data were collected at the University of North Carolina’s School of Dentistry; nonprofessional data were collected at Duke University in the Visual Cognition Laboratory; and TSA officer data were collected at Raleigh-Durham International Airport in a private testing room. The experiment was run in a dimly lit room; participants at the universities viewed the experiments on an Inspiron computer (Dell, Round Rock, Tex) with a 20-in cathode ray tube monitor, and participants at Raleigh-Durham airport viewed the experiments on Vostro 260 computers (Dell) and 23.6-in computer displays that were adjusted so that all participants were presented with stimuli of the same physical size. The participants were seated at a viewing distance of approximately 57 cm with no head restraint. Stimuli were presented and responses were recorded with MATLAB (MathWorks, Natick, Mass) using the Psychophysics Toolbox (version 3.0.8; http://psychtoolbox.org ). Questionnaire data were collected using the Qualtrics Research Suite (Qualtrics Labs, 2012; http://www.qualtrics.com/ ).
All participants completed 3 visual cognition tasks related to symmetry and presented in a blocked design; order was counterbalanced across all participants and tasks. Each task began with a series of practice trials, which were immediately followed by the experimental segment during which trial-by-trial accuracy and response time were recorded. At the start of each trial, a fixation cross was presented for 500 ms, followed by the stimulus. Participants responded to each trial with 1 of 2 possible keys, and no feedback was provided.
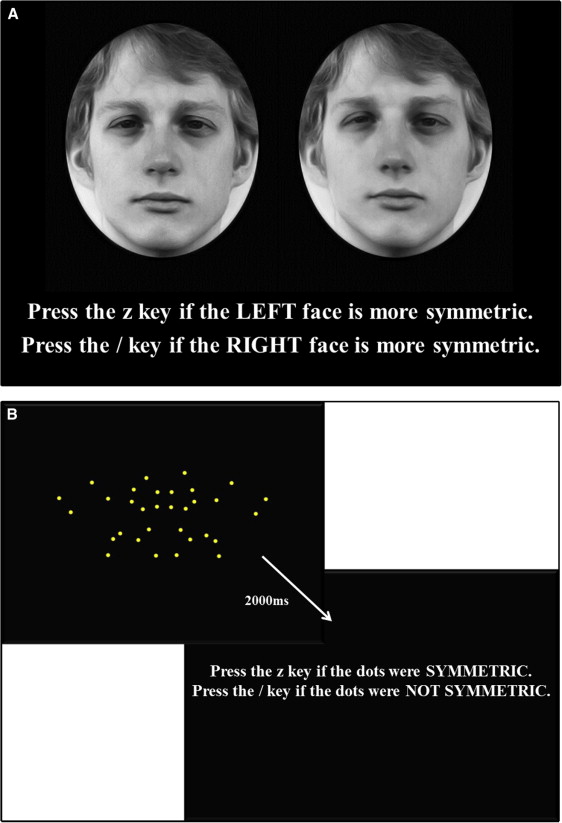
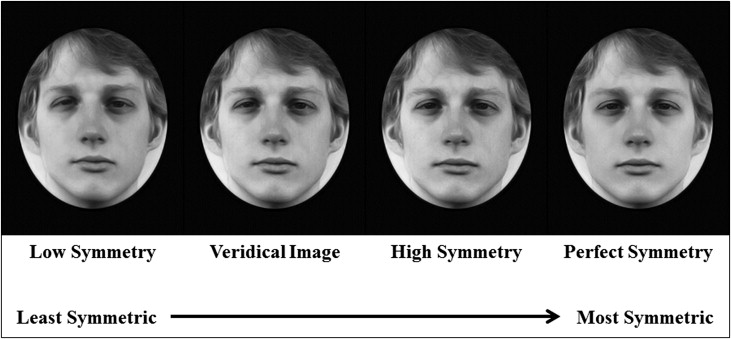
Task 1 was symmetry assessment of upright faces. After 6 practice trials, the participants assessed symmetry in 96 trials of upright faces by making a 2-alternative forced-choice judgment between 2 versions of the same face presented side by side ( Fig 1 , A ). Stimuli were presented on a black background, and the participant was instructed to press the “z” key if the face on the left appeared more symmetric or the “/” key if the face on the right appeared more symmetric. Stimuli were presented until the participant responded. Trials were counterbalanced using a random number sequence assignment for each participant as to whether the right or left face was more symmetric in each trial. Stimuli consisted of black-and-white photographs of faces of 16 (8 female) white people captured using symmetric lighting and morphed to varying levels of overall face asymmetry while preserving averaged proportions. All points in each photograph were morphed simultaneously to change overall face symmetry, not individual features such as the nose or chin (see the study of Rhodes et al for details on stimuli generation). Veridical hairstyles (ie, the unaltered hairstyles) were maintained for all versions of each face by editing the original stimuli set from Rhodes et al with Photoshop Elements10 (Adobe, San Jose, Calif) so that the hair could not be used as a cue to symmetry. Four versions of each face, varying in symmetry, were used: veridical (original) face, face with perfect symmetry, face with symmetry increased 50% from veridical, and face with symmetry decreased 50% from veridical ( Fig 2 ). By pairing each face version with all iterations of that face, 6 possible pairings were created (veridical with perfect symmetry, veridical with high symmetry, veridical with low symmetry, high symmetry with perfect symmetry, high symmetry with low symmetry, and low symmetry with perfect symmetry). These stimuli were presented at random in terms of both the levels of symmetry being compared and the face that was used. Participants viewed all possible pairings (96 pairings in total) of each face during task 1.
Task 2 was symmetry assessment of inverted faces. It was identical to task 1, but all stimuli were presented upside down. The sequence of presentation was randomized separately from task 1.
Task 3 was symmetry detection in dot patterns. Participants judged whether a dot pattern presented as a centered image on a black background was perfectly symmetric about its vertical axis ( Fig 1 , B ). Each dot image was displayed for 2000 ms, after which the participants were asked to make a response using the “z” key to indicate that the dot pattern was symmetric or the “/” key to indicate that the dot pattern was not symmetric. The 2000-ms display time was used to maintain consistency with a previously used experimental protocol. Stimuli were 18-dot patterns based on the body patterns of animals with bilaterally symmetric bodies (see the study of Evans et al for details). After 4 practice trials, each dot pattern was presented in random order in both upright and inverted conditions, for a total of 36 trials.
Immediately after all the visual tasks, each participant completed a Web-based questionnaire that asked for demographic information, strategies used during the symmetry assessment, and subjective self-confidence ratings for the tasks completed with the Royal College of Physicians confidence rating scale (4, fully confident in most cases; 3, confident in some cases; 2, satisfactory but lacking confidence; 1, not confident). The orthodontists and general dentists were asked whether the patient is most often upright or inverted when they assess face symmetry clinically and about their duration of training or clinical practice. The nonprofessionals and TSA officers were asked whether they had any training or experience in symmetry assessment.
Results
Descriptive statistics for accuracy, response time, and confidence ratings for each task are given in the Table . Normality of the data was confirmed using quantile-quantile plots, and homogeneity of variance between groups was confirmed using the Levene test. Accuracy and response times were compared among the groups using 1-way analysis of variance and the Tukey HSD test. Within-subject comparisons were made using paired t tests or Wilcoxon signed rank tests (for confidence ratings); statistical significance was set at P = 0.05. Reliability measures for the face symmetry tasks have been reported previously, with Cronbach alpha coefficients greater than 0.92 in all cases.
| Orthodontists (n = 31) | General dentists (n = 12) | Nonprofessionals (n = 23) | TSA officers (n = 10) | |
|---|---|---|---|---|
| Accuracy, mean (SD) | ||||
| All faces | 85.5 (3.8) | 82.4 (5.0) | 79.7 (6.7) | 79.1 (6.0) |
| Upright faces | 87.0 (4.1) | 84.8 (6.8) | 80.8 (7.9) | 79.8 (6.7) |
| Inverted faces | 84.0 (4.7) | 80.0 (4.8) | 78.6 (7.1) | 78.4 (6.2) |
| Dots | 63.8 (10.3) | 61.6 (6.1) | 65.8 (10.8) | 63.9 (9.1) |
| Response time, mean (SD) | ||||
| All faces | 7.5 (3.0) | 8.5 (7.7) | 3.3 (1.5) | 7.7 (3.9) |
| Upright faces | 7.6 (3.3) | 8.3 (6.6) | 3.2 (1.6) | 7.7 (4.4) |
| Inverted faces | 7.4 (4.2) | 8.8 (9.3) | 3.3 (1.5) | 7.6 (4.0) |
| Dots | 0.9 (0.4) | 0.8 (0.2) | 0.6 (0.3) | 0.9 (0.5) |
| Confidence, percent of responses indicating confidence ∗ | ||||
| Upright faces | 100 | 91.7 | 91.3 | 70 |
| Inverted faces | 61.3 | 75.0 | 52.1 | 50 |
| Dots | 41.9 | 66.7 | 52.1 | 70 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


