Introduction
The purposes of this in-vivo study were to compare the modes of failure of uncoated and adhesive precoated metal brackets by using the adhesive remnant index, and to assess the quality of the enamel surface after cleanup by using the enamel damage index.
Methods
Twelve Victory brackets (group A) and 12 Victory adhesive precoated brackets (group B) (both, 3M Unitek, Monrovia, Calif) were bonded onto the maxillary second premolars of 12 volunteers. The uncoated brackets were bonded with Transbond XT adhesive resin (3M Unitek). Replicas of the teeth were made before bonding (T0), after bracket removal (T1), and after cleanup (T2). Scanning electron microscope images of all labial enamel surfaces were taken at T0, T1, and T2, and these were evaluated according to the adhesive remnant index and the enamel damage index.
Results
Evaluation of the adhesive remnant index scores with the chi-square test showed no statistically significant difference between the groups. Evaluation of the enamel damage index grades with the sign test for paired samples showed a statistically significant difference ( P <0.01) between T0 and T2.
Conclusions
Uncoated and precoated brackets exhibited similar debonding patterns. Additionally, the debonding method tested in this study did not restore the original enamel surface, although there was no clinically relevant enamel damage.
After orthodontic treatment with fixed appliances, bonded brackets and any residual adhesive must be removed. Ideally, the debonding procedure should lead to restitutio ad integrum of the enamel or, at least, restore the enamel surface as closely as possible to its pretreatment condition.
During bracket removal, bond failure can occur at the adhesive-enamel interface or at the adhesive-bracket interface (adhesive failure), or within the adhesive (cohesive failure). Generally, bracket failure is a combination of adhesive and cohesive failures, the latter resulting in retention of material on the enamel and bracket surfaces (mixed failure). When adhesive failure between the adhesive resin and the enamel surface occurs, a certain amount of enamel loss is almost inevitable because of the micromechanical bond between the composite resin bonding agent and the acid-etched enamel.
At present, no universally approved protocol has been established for the removal of adhesive resin after debracketing, and no instrument can achieve complete composite removal without affecting the enamel surface. Even though tooth dehydration and absence of ion exchange between saliva and tooth can affect debonding, most studies evaluating the removal of adhesive resins have been conducted in vitro. The purposes of this in-vivo study were to (1) evaluate whether there are any differences in the mode of failure of uncoated metal brackets vs adhesive precoated metal brackets, and (2) assess the quality of the enamel surfaces after cleanup.
Material and methods
Twelve dental students (3 women, 9 men; mean age, 23.5 ± 1.34 years) were enrolled in the study. Each participant was informed of its objectives and provided informed consent.
The teeth used for evaluation were selected based on visual observation of the soundness of the coronal portion, the absence of cavities and cracks on the labial surface, and the lack of exposure to chemical agents.
As has been reported in previous in-vitro studies and for esthetic reasons, the volunteers received brackets on their maxillary second premolars. A total of 24 premolars were examined and categorized as follows: group A, 12 premolars (8 on the right side, 4 on the left side of the mouth) were bonded with uncoated metal brackets (Victory Series; 3M Unitek, Monrovia, Calif); and group B: 12 premolars (4 on the right side, 8 on the left side of the mouth) were bonded with adhesive precoated metal brackets (APC II Victory Series; 3M Unitek).
The teeth were randomly divided into 2 groups by flipping an unbiased coin for the right side of each volunteer’s mouth; on the basis of this result, the left side was assigned to the remaining group.
The labial enamel surfaces of the teeth were cleaned and polished with slurry made of nonfluoride pumice and water by using a slow-speed hand piece for 20 seconds; they were then rinsed for 20 seconds and dried for 10 seconds with a moisture-free air spray.
Impressions of the teeth were taken by using polyvinyl siloxane (President Plus Light-Body, Coltène, Altstätten, Switzerland) and cast in epoxy resin (Epofix; Struers, Ballerup, Denmark) to obtain replicas of the labial surfaces before bracket bonding (T0). Subsequently, the enamel was etched with 35% orthophosphoric acid gel (Scotchbond, 3M Unitek) for 30 seconds, rinsed with water, sprayed with air for 30 seconds, and dried for 20 seconds until the etched enamel surfaces had a white frosty appearance, as reported by Al Shamsi et al and Kitahara-Céia et al.
A thin uniform coat of adhesive agent (Transbond XT Light Cure adhesive primer; 3M Unitek) was applied to the teeth with a microbrush. A small amount of adhesive resin (Transbond XT; 3M Unitek) was placed on the base of the uncoated brackets in strict accordance with the manufacturer’s instructions.
The brackets were then placed on the tooth surfaces, adjusted to their final positions, and pressed firmly in place. After removing excess resin from the periphery of the bracket base with a dental probe, light curing for 20 seconds (10 seconds from the mesial side and 10 seconds from the distal side) by using a halogen unit (Demetron A2, Demetron-SDS© 2007; KerrHawe SA, Bioggio, Switzerland) was performed according to the manufacturer’s instructions.
As reported by Eliades et al, and to ensure maximum bond strength, 7 days (T1) after bonding, the brackets were removed by gently squeezing the mesial and distal wings with bracket removal pliers (Ormco, Glendora, Calif). After bracket removal, second impressions of the labial surfaces of the teeth were taken and replicated in epoxy resin.
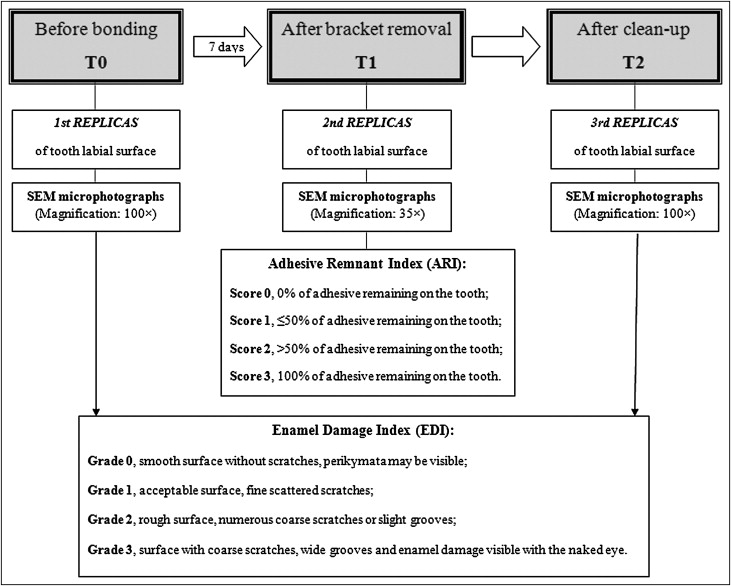
The adhesive remnants were carefully removed from the teeth by using a 12-blade tungsten carbide bur (H247; Komet, Lemgo, Germany) driven on a low-speed hand piece at 20,000 rpm without water cooling. This procedure was followed by sequentially finishing the residual resin and underlying enamel with medium, fine, and ultrafine aluminum oxide-impregnated discs (Sof-Lex; 3M Dental, St Paul, Minn) driven on a low-speed hand piece at 10,000 rpm. Complete removal of the composite resin was verified by visual inspection of the teeth under a dental operating light, after which the teeth were cleaned with water spray. The same operator (M.Z.) performed all clinical procedures. After cleanup again (T2), the third impressions of the labial surfaces were taken, and epoxy resin replicas were produced. The study protocol is summarized in Figure 1 .
The dental replicas were mounted on aluminum stubs, sputter-coated with a 300-Å layer of gold and palladium (Sputter Coater SC7620; Polaron, East Grinstead, United Kingdom) and analyzed with a high vacuum scanning electron microscope (JSM-5200; JEOL, Tokyo, Japan) capturing secondary electron images at 15 kV, at a working distance of 20 mm.
To determine the amount of resin remaining on the surface of the teeth at T1, microphotographs of the epoxy resin replicas taken at a magnification of 35 times were assessed with the adhesive remnant index described by Årtun and Bergland. Adhesive remnant index scores range from 0 to 3, with 0 indicating that no adhesive remained on the tooth, 1 indicating that ≤50% of the adhesive remained on the tooth, 2 indicating that >50% of the adhesive remained on the tooth, and 3 indicating that 100% of the adhesive remained on the tooth.
Because we found no differences in the amounts of adhesive left on the enamel surfaces between the 2 adhesive systems, groups A and B were combined to assess the quality of the enamel surface.
The status of the enamel surface at T0 and T2 was evaluated according to the enamel damage index, a measure adapted from the surface roughness index described by Howell and Weekes, which includes the following categories: grade 0, smooth surface without scratches, and perikymata might be visible; grade 1, acceptable surface, with fine scattered scratches; grade 2, rough surface, with numerous coarse scratches or slight grooves visible; and grade 3, surface with coarse scratches, wide grooves, and enamel damage visible to the naked eye.
To determine the enamel damage index grade, microphotographs of the epoxy resin replicas were taken at a magnification of 100 times.
Adhesive remnant index and enamel damage index evaluations were performed by an examiner (S.M.), who did not know to which group (A or B) or phase (T0 or T2) the specimens belonged. The evaluations were repeated by the same examiner 1 week later. If any discrepancies arose, a third assessment was performed to determine the final score.
Statistical analysis
By hypothesizing an expected difference between the 2 groups in the adhesive remnant index score of 1 point, at an α level of 0.05 and with a power of 80%, a minimum of 12 premolars was required for each group. A nonparametric chi-square test was used to evaluate any differences in the adhesive remnant index scores between the groups. In addition, we performed a sign test for paired samples using a binomial distribution to evaluate the enamel damage index scores of the surfaces at T0 and T2. P values of <0.01 were considered statistically significant.
Results
No discrepancies arose in the determination of the adhesive remnant index scores or the enamel damage index grades between the first and second assessments by the examiner (S.M.), so a third assessment was not required. The distribution of the adhesive remnant index scores for the groups is shown in Table I . The chi-square analysis did not show a statistically significant difference in the sites of bond failure between the uncoated (group A) vs the precoated (group B) brackets ( P = 0.8897).
| Group | ARI score | Chi-square | P | |||
|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | |||
| A | 0 | 3 | 3 | 6 | 0.2338 | 0.8897 |
| B | 0 | 3 | 4 | 5 | ||
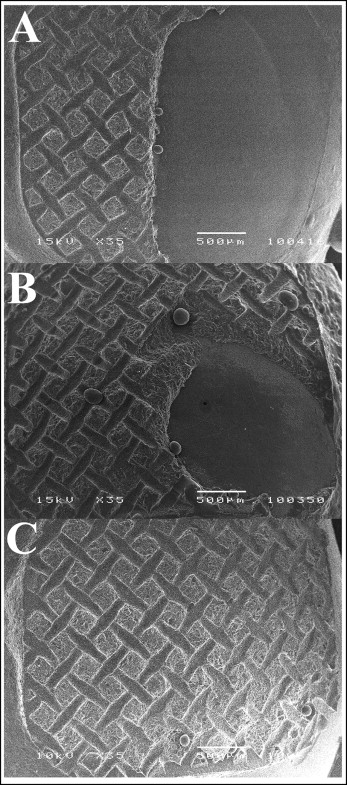
Figure 2 shows representative examples of teeth with the different residual adhesive patterns observed. The distributions of the modes of failure of uncoated vs precoated metal brackets for the groups of teeth are shown in Table II . For the uncoated brackets, bond failures occurred at the bracket-adhesive interface in 50% of the cases, resulting in an adhesive remnant index score of 3. The remaining 50% exhibited a combination of adhesive and cohesive failure, corresponding to adhesive remnant index scores of 1 or 2. For the precoated brackets, the predominant mode of failure was mixed (58.3%).

Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


