Introduction
The aim of this study was to compare the esthetic judgments of orthodontists and laypeople regarding the appearance of palatally displaced canines 3 months after treatment with either a closed or an open surgical exposure and orthodontic alignment.
Methods
A multicenter randomized controlled trial was undertaken in 3 hospitals in the United Kingdom. Patients with unilateral palatally displaced canines were randomly allocated to receive either a closed or an open surgical exposure. The teeth were aligned with fixed appliances, and 3 months after debond, intraoral photographs were taken. The photographs were projected in random order to 2 panels of judges (orthodontists and laypeople), who completed a questionnaire.
Results
The images of 67 participants (closed, 33; open, 34) were included. The laypeople were able to identify the operated tooth only 49.7% of the time (95% CI, 45.3%-54.0%); this was no better than chance ( P = 0.880). The orthodontists were more successful but still identified the treated canine with certainty only 60.7% of the time (95% CI, 53.7%-67.8%; P = 0.003). Both panels more frequently assessed the unoperated canine to have a better appearance than the contralateral operated canine; however, there were no differences between the closed and open groups (proportion preferring unoperated canine—laypeople: closed, 58.7%; open, 57.0%; P = 0.43; and orthodontists: closed, 60.9%; open, 60.6%; P = 0.27).
Conclusions
There is an esthetic impact to aligning a palatally displaced canine, but it is mostly minor and unlikely to be detectable by laypeople. The esthetic impact was the same, whether the canine was exposed with a closed or an open surgical technique.
Highlights
- •
Two panels rated palatally displaced canines treated with closed or open technique and aligned.
- •
Both panels assessed the unoperated canine to have a better appearance than the operated canine.
- •
Laypeople identified the operated tooth correctly 49.7% of the time and orthodontists 60.7% of the time.
- •
There was no difference between canines surgically exposed with the closed or the open technique.
- •
The esthetic impact of aligning a palatally displaced canine is undetectable by most laypeople.
Wisth et al suggested that a closed surgical exposure of a palatally displaced canine (PDC) leads to better periodontal outcomes than an open surgical exposure; however, this was an inherently weak retrospective study. A systematic review found no evidence of the superiority in terms of clinical attachment levels after treatment with one technique over the other. A recent randomized controlled trial has confirmed this.
One outcome that has received limited investigation is the esthetic appearance of the PDC after surgical exposure and alignment. D’Amico et al obtained the esthetic judgments of orthodontists and patients concerning displaced canines that had been exposed with a closed surgical technique and orthodontically aligned. Their sample included the clinical photographs of 61 patients with either unilateral or bilateral, buccally or palatally displaced canines, at a mean of 3.5 years after debond. They found that orthodontists rated the esthetic results as “good” in 57% of the patients, “acceptable” in 26%, and “not good” in 17%. Interestingly, the orthodontists were able to correctly identify only 48% of the canines that had a unilateral buccal displacement compared with the normal contralateral tooth and 61% of those that had a unilateral palatal displacement.
Ling et al investigated the posttreatment appearance of unilateral displaced palatal canines in 28 patients; half of them had surgical exposure and assisted eruption, and half had unassisted eruption. The canines that had surgical exposure were identified by 2 orthodontists in 12 of 14 cases, and both assessors used differences in inclination and the appearance of the labial and gingival contours. All 14 subjects in the surgical exposure group were either “satisfied” or “very satisfied” with their overall final appearance.
No studies in the literature have investigated the judgments of laypeople concerning the appearance of treated PDCs. It has been shown that dentists and orthodontists differ compared with laypeople in their judgments about the appearance and gingival health of the canine crown. The aim of this study was therefore to explore any differences in the esthetic outcomes of canines exposed using a closed vs an open surgical technique in the views of 2 groups of judges: orthodontists and laypeople.
The following research questions were investigated.
- 1.
Can the operated canine be identified by the orthodontists or the laypeople?
- 2.
Were the judges able to identify the operated canine more frequently when it was treated with a closed or an open surgical procedure?
- 3.
Is there a difference in the appearance of the teeth and gingivae between the 2 surgical procedures? This was judged in terms of the following.
- a.
Which canine looks better? Is the gum health better if it is exposed with a closed or an open procedure?
- b.
Does the length of the canine have a tendency to be too long in the closed group and too short in the open group?
- a.
- 4.
Are orthodontists better than laypeople at identifying the operated canine?
The study was undertaken to test the equivalence between the 2 techniques. Traditional comparative studies test the hypothesis that there is a difference between the 2 techniques and whether there is insufficient evidence that a difference exists (nonsignificant P value), and then the researchers conclude that equality cannot be ruled out. Equivalence studies aim to test the opposite: ie, the evidence supporting equivalence. If there is not strong evidence supporting equivalence, then researchers conclude that nonequivalence cannot be ruled out.
An assumption was made that equivalence would be established if the proportions of assessors correctly identifying the operated and unoperated teeth surgically exposed with a closed or an open procedure were 50% and within an equivalence margin of 10%.
Three research hypotheses were tested: (1) there is no difference in the assessors’ judgments of the appearance of operated and unoperated canines; (2) there is no difference in the assessors’ judgments of the appearance of PDCs treated with either a closed or an open surgical exposure; and (3) there is a difference in the esthetic judgments of laypeople and orthodontists.
The first 2 hypotheses were examined by looking at the confidence intervals of the differences to see whether there was equivalence or clinically meaningful differences. The third research hypothesis was tested by the more traditional method of examining the probability that there was no difference, because it was assumed that orthodontists would be more expert than laypeople.
The null hypotheses tested were (1) the assessors’ judgments of the appearance of operated and unoperated canines are not equivalent; (2) the assessors’ judgments of the PDC treated with either a closed or an open surgical exposure are not equivalent; and (3) the esthetic judgments of laypeople and orthodontists are equivalent.
Material and methods
The clinical material used in this study was collected as part of a multicenter randomized controlled clinical trial involving 2 parallel groups of patients with unilateral PDC. Details of the study methodology, including the inclusion and exclusion criteria, have been described elsewhere. Briefly, the participants who agreed to take part and provided informed consent were randomized to receive either a closed or an open surgical procedure for their unilateral PDC. After surgery, orthodontic treatment was undertaken by a specialist orthodontic practitioner to align the PDC. On completion of treatment, the appliances were removed and the patient was supplied with a removable retainer to wear at night. Three months after debond, records were obtained, including clinical photographs, which were used in the assessment process.
Two groups of judges were convened: a dental panel comprising 11 specialist orthodontists (6 men, 5 women) and a lay panel comprising 11 professional people (5 men, 6 women) in nondental occupations. The orthodontists were mainly senior specialists (National Health Service consultants) and participated in the assessment process during a regional audit meeting. The lay panel was a convenience sample of nondentists. No incentive or reward was given to participants for taking part, except that refreshments were provided.
The panels were shown a PowerPoint (Microsoft, Redmond, Wash) presentation of the 3-month debond photographs. Before each presentation, a brief overview of the study was given to both groups, with images to explain the salient points. The participants were told that there were no right or wrong answers and were asked to give their own assessments, without conferring.
Each slide consisted of the buccal intraoral images of both the operated and unoperated sides of 1 subject ( Fig 1 ). Each member of the 2 panels was asked to rate the appearance of the 2 canines using a standard assessment sheet that was developed and piloted among the research team before use ( Supplementary Appendix 1 ). After the initial piloting and modification, the assessment sheet was piloted and modified again among 3 orthodontists and 3 laypeople who were not involved in the final process.
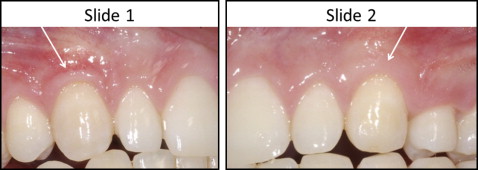
For the final assessment process, the principles of scoring were explained thoroughly, especially among the laypeople. The judgments requested included ratings of gingival health and appearance of each operated and unoperated maxillary canine. Assessment of appearance included a rating of crown length using a visual analog scale (VAS) consisting of a 100-mm line labeled “very poor” on the left and “very good” on the right. The respondents were also asked for their subjective judgments about whether they considered the tooth crown to be too long or too short, which tooth looked better, and which tooth they thought had been operated on. After the first slide, only 1 minute was allowed for the assessment.
Statistical analysis
For the assessment of whether the operated canine could be identified, the outcome was a binary yes or no response. Although there was a category for those who could not guess, this was interpreted as “no” because the question asked was whether the operated canine could be identified. If any observers were unable to decide, then this was interpreted as meaning that they could not identify it correctly.
For each set of patient images, the percentage of times that the operated tooth was correctly identified was calculated. To examine whether the correct tooth could be identified, a 1-sample t test was conducted to determine whether the proportion of correctly identified treated teeth was significantly different from chance: ie, greater than 50%. The confidence intervals were examined for clinically significant differences. Responses from lay judges and orthodontists were analyzed separately, and any potential differences between the panels were examined in the same manner.
To determine whether a closed or an open surgical exposure resulted in a better appearance, several outcome variables were used. The observers were asked to rate whether they thought that one canine looked better than the other, or whether both were the same. In addition, gum health was measured directly on a continuous 0 to 100 point VAS. It was expected that in most cases the untreated canine would be rated as looking better than the operated canine; therefore, the percentage of times that the untreated canine was thought to look better was initially compared between the closed and open groups using a 2-sample t test. For these analyses, interest was focused on the differences between the 2 procedures, and so no comparisons were made between orthodontists and laypeople. When analyzing the continuous measure of gum health, analysis of variance (ANOVA) using a random-effects model was carried out, with the assessors as a random effect. Differences between the assessors were not inherently of interest, but by fitting them as a random effect it allowed us to account for the between-assessor variations in the analysis and report the differences between the 2 operations, after adjustment for assessor. In addition, the health of the untreated canine was fitted as a covariate to control for what the tooth should look like. The data were analyzed with SPSS software (version 20; IBM, Armonk, NY).
The final analysis was concerned with crown length. Was there a difference between the 2 procedures in terms of the length of the operated canine when compared with the unoperated canine? ANOVA with a random-effects model was fitted with the length of the treated tooth as the outcome variable, and assessor was fitted as a random effect. In addition, the length of the untreated canine was fitted as a covariate to control for what the tooth should look like. As with the analysis of gum health, interest was focused on the difference between the 2 procedures, and so no comparisons were made between orthodontists and laypeople.
No repeatability study was performed because we were interested in what the judges first thought about the appearance of the canines. On examining the data, we saw that there were discrepancies in the recording of the judgments by 1 orthodontist, and those data were subsequently excluded from the analysis.
Results
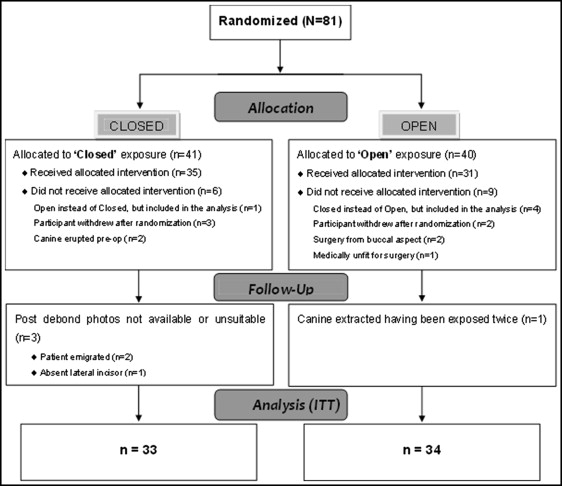
Recruitment of participants to the clinical trial commenced at the beginning of August 2002 and finished at the end of January 2007. Figure 2 shows the flow of patients through the trial, and the numbers included and excluded from the esthetic analysis. Eighty-one participants were recruited, but 10 were excluded from all analyses, as outlined in a previous report. Four participants were excluded from the esthetic analysis: 1 patient was missing a lateral incisor (closed); 1 patient had the canine extracted after 2 attempts at surgical exposure (open); and in 2 participants, no postdebond photographs were available (closed). Five participants received the incorrect procedure (closed, 1; open, 4); however, the intention-to-treat principle was adhered to, and they were all analyzed in their original allocated groups.
Question 1: Can the operated canine be identified by the orthodontists and laypeople?
On average, 60.7% (95% CI, 53.7%-67.8%) of the time the orthodontists correctly identified the tooth that was operated on, and this percentage was significantly different from the null percentage of 50% ( P = 0.003) ( Table I ). The results for the laypeople indicated that they could not tell the operated canine from the unoperated canine; on average, they identified the operated canine correctly 49.7% of the time (95% CI, 45.3%-54.0%), and this did not differ significantly from the null value ( P = 0.880). Interestingly, 1 lay judge was particularly good at identifying the treated canine, with 71.6% of the responses correct. This was the second highest success rate of all the judges; an orthodontist had the highest score of 73.1% for correct identifications.
| Correctly identified, %, mean (95% CI) | Difference (%) (95% CI) | P value | |
|---|---|---|---|
| Operated vs unoperated | |||
| Orthodontists | 60.7 (53.7-67.8) | 0.003 | |
| Laypeople | 49.7 (45.3-54.0) | 0.880 | |
| 11.1 (4.3-17.9) | 0.002 | ||
| Orthodontists | |||
| Closed | 59.4 (48.5-70.3) | ||
| Open | 62.1 (52.6-71.5) | ||
| 2.7 (−11.4-16.8) | 0.470 | ||
| Laypeople | |||
| Closed | 49.6 (43.0-56.2) | ||
| Open | 49.7 (43.8-55.7) | ||
| 0.2 (−8.6-8.9) | 0.620 | ||
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


