Endoscopy has proven to be a valuable tool in almost every surgical specialty. Patients have benefited from smaller incisions, less morbidity, and rapid convalescence. It is not surprising that in the world of cosmetic surgery, where patients are becoming ever more knowledgeable and demanding, endoscopic procedures are increasingly popular. Of all endoscopic procedures performed, the endoscopic forehead and brow lift has proved to be the most common and predictable of the facial cosmetic techniques.
Facial cosmetic surgery has had an unprecedented steady increase in popularity over the past 20 years. The desire of the aging population to feel and look rejuvenated has led to new techniques that provide a more youthful and natural appearance and offer faster recovery. Rejuvenation of the upper third of the face is a vital component for proper treatment of the aging face.
Esthetic concerns of the forehead and brow regions affect a wide range of age groups. In contrast to standard lower face and neck rhytidectomies that are more commonly performed on patients older than age 45, cosmetic concerns in the upper third of the face may be evident for patients in their 20s and 30s because of genetic predisposition. The forehead and the brow must be fully evaluated for a wide range of interlacing problems. Matching the diagnosis to the ideal rejuvenation technique(s) is essential for maximum esthetic benefit. Thinning skin and laxity due to age and gravity represent only a portion of the forehead and brow region dynamics. One must address all problems to achieve optimal results and patient satisfaction.
The endoscopic forehead and brow lift is a comprehensive operation and is not just a method used for raising the brows. When used properly, it can address not only brow ptosis but also dynamic muscular problems ( Figure 26-1 ). This procedure yields more dramatic facial improvement when properly and selectively combined with other rejuvenation procedures such as fat grafting, skin resurfacing, Botox, and bone remodeling. Correct diagnosis of age-related changes is critical.
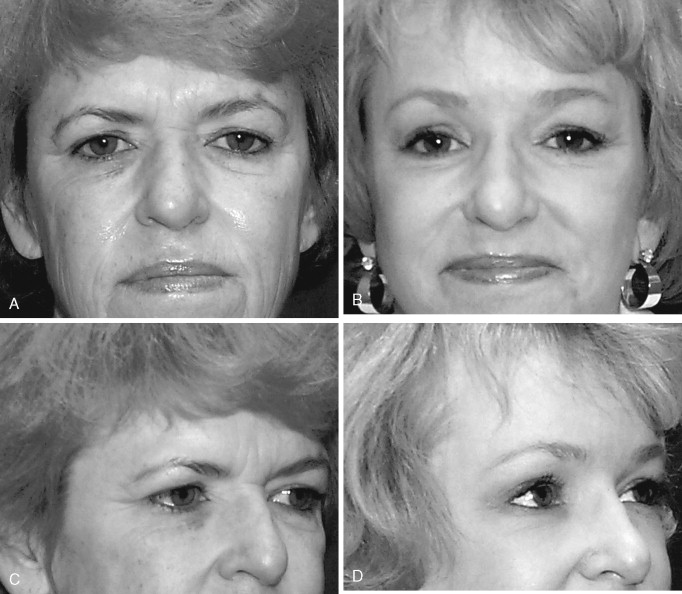
The aging process typically leads to forehead and brow ptosis for almost every patient. However, it is necessary to determine whether the ptosis seen around the forehead and brow region is due to a problem with brow position or with upper eyelid laxity, or whether it is caused by the combination of the two. Sometimes, what others may see as ptosis in the lateral brow may actually be fat atrophy that can be better rejuvenated with fat grafting than with lifting of the brow. Still other problems such as dynamic lines produced by muscle activity in the glabellar region and in the forehead itself also must be addressed. Skin texture, variable hairline patterns, bony abnormalities, and asymmetries should be evaluated.
Rejuvenation of the upper third of the face can be one of the most rewarding and fulfilling procedures one can offer to select patients. Specific elevation and correction of lateral hooding, along with a reduction in wrinkles, can result in a natural appearance yet still can impart a tremendous improvement in the patient’s overall beauty and youthful appearance. The goal of this chapter is to review upper facial third anatomy specific to the endoscopic forehead brow lift procedure.
ANATOMIC AND ESTHETIC CONSIDERATIONS
It is commonly accepted that a youthful forehead represents roughly one third of the overall facial height. In essence, the distance from hairline to glabella is equal to the distance from the glabella to the point at the base of the columella (subnasale). A youthful appearing eyebrow is different for men than for women. The female eyebrow should be arched with the peak point of the brow on a sagittal line of the lateral limbus of the eye. The brow itself should be positioned just above the orbital rim, in contrast to a typical male eyebrow, which should lie along the orbital rim in a more horizontal fashion.
The comprehensive anatomy of individual areas has been well described in the literature, often in relation to the specific procedure that is being performed. Therefore, the anatomic discussion can be simplified by separating the specific regions into bone anatomy, muscle and fascial anatomy, vessel and nerve anatomy, and endoscopic anatomy. Each anatomic region will be addressed specifically here so the reader will gain an understanding of surgical anatomy as it relates specifically to the endoscopic forehead and brow lift.
BONE ANATOMY
The highest percentage of bony landmarks for the forehead and brow lift involve the frontal bone, and adjacent parietal bone, zygoma, maxilla, and nasal bones will be at least partially exposed when the procedure is performed. The connections (suture lines such as nasofrontal, zygomatico-frontal, and coronal) are important landmarks because they can be clinically pertinent for limits of dissection and can help the surgeon to know these locations during dissection. Case in point, the fronto-zygomatic suture line is the location at which some surgeons may elect to halt dissection for a basic brow lift. Just posterior and slightly inferior to this suture line is the sentinel vein. This vein is avoided to prevent undesirable bleeding that may complicate the procedure. Some surgeons elect to ligate and transect this vein for further tissue release. Knowledge of its location in relation to the adjacent bone landmark is critical. Additional dissection can be performed if mid-face lifting is also considered, or if the patient desires more elevation at the lateral canthal region. Elevation in the subperiosteal plane below the fronto-zygomatic suture into the cheek can be performed for increased lift in the mid-face. Overaggressive dissection into the cheek and around the orbit can create an unnatural “cat eye” appearance if too much tissue is elevated, particularly medially along the fronto-zygomatic suture line and the deep lateral canthus.
The nasofrontal suture line is an excellent landmark to note during dissection. First, dissection needs to proceed only a few millimeters below this suture level onto the nasal bones for adequate release. Second, the paired procerus muscles can be identified here and transection performed if indicated. Third, depending on the point of horizontal transection in this area, the nasofrontal angle location can be altered slightly if desired. Lastly, nasal tip rotation can be achieved if desired, particularly with considerable dissection below the nasofrontal suture line.
Another critical bony landmark is the orbital rim and associated arcus marginalis (orbital rim margin), which limits inferior dissection but must be well visualized and freed of periosteal attachments if the brow and brow fat pads are to be lifted for lasting results. Significant muscle and fascial attachments are also located at the level of the orbital rim medially and laterally. The tenacious temporal fusion line that exists along the temporal ridge is important to identify during dissection; it is equally important for the clinician to know its location preoperatively, so that correct incision placement can be made to facilitate clean dissection under this area. Clean dissection, free of hanging or torn tissues, is critical for adequate endoscopic visualization.
Bony thickness varies in different areas of the skull, and this must be recognized when fixation methods that drill into the skull are used. In addition, venous lakes along the diploe surface of the skull tend to be more centralized around the sagittal suture line, and drilling here should be avoided. Thickness increases posteriorly near the occiput, but screw or bone tunnel fixation here is not required. Caution must be taken to avoid bone penetration near the temporalis muscle in the lateral skull region, where the middle meningeal arteries could be injured. Awareness of average thickness for a given location and of internal anatomy is necessary before drilling into the skull is performed for any reason. The safest site used for bone tunnels or screws for brow lifting is located along a parasagittal line, approximately at the mid-pupil or lateral limbus line and just anterior to the coronal suture.
MUSCLE AND FASCIAL ANATOMY
Paired muscles of the forehead and brow region are commonly thought of as elevators and depressors. Although the depressors can actually move in an oblique or circular fashion, the only true elevator of the forehead, the frontalis, moves upward to raise the brow. This movement, along with some static tone, maintains brow position and can produce horizontal creases over time. The frontalis muscle originates from the deep galeal plane (galea aponeurotica that connects to the occipital muscle posteriorly). It inserts into the orbital portion of the orbicularis oculi muscle inferiorly, and this inserts into the dermis immediately below the eyebrow. Its lateral extension fuses into the dense collection of fascia approximately 1 cm wide, called the zone of adherence ; this zone runs the length of the superior temporal line and ends inferiorly just above the zygomatico-frontal suture at an attachment of fascia known as the orbital ligament. These areas are important clinical anatomic regions because freeing the zone of adherence is necessary to achieve good long-term results with lift procedures. Care is required in this region to avoid overzealous stretching and injury to the facial nerve.
The acronym SCALP applies in the forehead for the standard layers: s kin, sub c utaneous tissue, a poneurosis (the thick galeal fascia), l oose areolar (subgaleal) plane, and p eriosteum. The galeal fascia has simply blended into the frontalis muscle and its midline fascial attachments at the forehead level. This allows sliding movement over the scalp with contraction of the muscle. The frontalis and the galea may be thought of as an extension of the temporoparietal fascia in the temporal region and in the SMAS (superficial musculoaponeurotic system) below the level of the zygomatic arch. The temporoparietal fascia appears somewhat spongy and houses the frontal branch of the facial nerve on its undersurface in the temporal region.
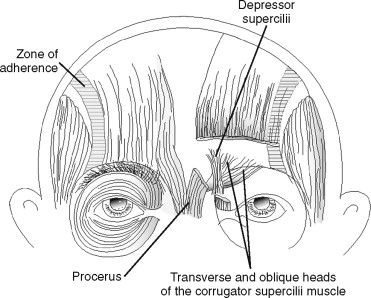
Several other paired forehead and brow muscles thought of as “depressors” are present along the brow and facilitate facial expression. The two most well recognized of these are the procerus and the corrugator supercilii muscles, which are present in the glabella. The procerus muscles are paired superiorly but fuse inferiorly into a single muscle belly that originates on the nasal bones and cartilages. It inserts into the midline intervening medial frontalis muscle fibers and the overlying dermis. The procerus is responsible for depression and frowning between the eyes that often creates a horizontal crease (bunny line) across the upper portion of the nose. The corrugator supercilii muscles are depressors that act obliquely across the glabella and form the classic vertical lines seen during squinting or frowning. These muscles create an “angry” appearance. The corrugator supercilii originates from the frontal bone just above the nasal bones and inserts into the dermis of the medial brow. The corrugator has two heads, the oblique and the transverse, which act in unison to pull the medial brow down and together. Collectively, the paired procerus and corrugator muscles are the main depressors of the medial brow and are the muscles most commonly treated with Botox to help alleviate frown lines in the glabella. These same two muscles are most often transected during an endoscopic brow or forehead lift to achieve a smooth and long-lasting result.
Another depressor muscle of importance is the depressor supercilii muscle, which originates on the frontal process of the maxilla just inferior and superficial to the origin of the corrugator supercilii. It inserts into the medial frontalis fibers and dermis just above the medial brow. The depressor supercilii is important because it is superficial to the corrugator and is easily treated inadvertently with Botox. It is also important because it lies behind the corrugator during a brow lift and can be transected via aggressive dissection through the corrugator muscle. Although a few patients with very low medial brow position may occasionally benefit from this maneuver, it more often causes over-elevation of the medial brow and creates the “surprised” look. Superficial to the depressor supercilii is the orbital portion of the orbicularis oculi, which inserts into portions of the adjacent depressors, the surface of the inferior frontalis, and the dermis below the brow. The orbital portion of the orbicularis muscle originates, to some extent, from the medial canthal tendon and from adjacent bone ( Figure 26-2 ). Deep to all the depressors is the galeal fat pad, which lies directly below the transverse head of the corrugator and helps to reveal the locations of muscular landmarks when it is exposed clinically after transection through the periosteum along the orbital rim.
Lastly, paired temporalis muscles are located in each temporal fossa, where they originate and then insert onto the coronoid process of the mandible. The importance of these muscles during upper facial rejuvenation is most often related to its overlying temporalis fascia, which can be used to delineate surgical planes and aid in fixation. The temporalis fascia is adherent to the temporalis below and splits into superficial and deep layers in the lower half of the fossa. For consistency, the superficial layer of the deep temporalis fascia describes only that portion of the deep temporalis fascia that is present at the level of the split; the area below is referred to simply as the temporalis fascia, that is, the deep, thick fascial layer seen clinically from the temporal crest down to the zygomatic arch. The spongy temporoparietal fascia, which is superficial to the dense and glossy white–appearing temporalis fascia, houses the frontal branch of the facial nerve within its deep surface.
One method of fixation that may be performed during brow lifting involves using suture to fixate the temporoparietal fascia from below a skin incision to the adherent temporalis fascia in a more superior position, to elevate the lateral brow and upper cheek. Some surgeons advocate removing a window of temporalis fascia during this suture fixation procedure and exposing the underlying temporalis muscle in the hope of gaining additional fibrosis and improving fixation longevity.
VESSEL AND NERVE ANATOMY
Perfusion to the upper face and scalp is excellent and comes from multiple sources. Several major blood vessels of the upper face and scalp, including the superficial temporal artery and the facial artery, originate from the external carotid. These give rise to the blood supply in the medial canthal region via the angular artery and in the lateral canthal region via the frontal or anterior branch of the superficial temporal artery. The internal carotid artery branches to the middle meningeal artery and to the ophthalmic artery, which gives rise to the supraorbital and supratrochlear arteries that exit their respective foramina and supply most of the forehead and mid-scalp region. The terminal arterial branches of the upper face have multiple significant anastomoses with adjacent vessels.
Venous drainage of the upper face follows the respective arterial supply, although this pattern can vary. Still, one particular vein that is relatively consistent is known as the sentinel vein (medial zygomatico-temporal vein); this vein runs perpendicular through the temporalis fascia at a location approximately 2 cm lateral or posterior to the lateral canthus. It is clinically significant during endoscopic procedures because of the problems that are created by injury to it, such as bruising and impaired visualization. As one elevates the tissues inferior to the zygomatico-frontal suture in the subperiosteal plane, care must be taken to avoid careless dissection laterally, where the sentinel vein can be accidentally torn.
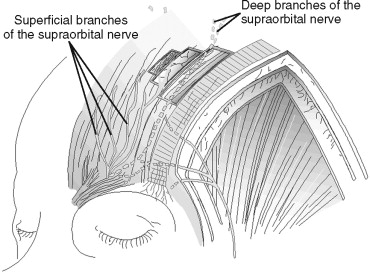
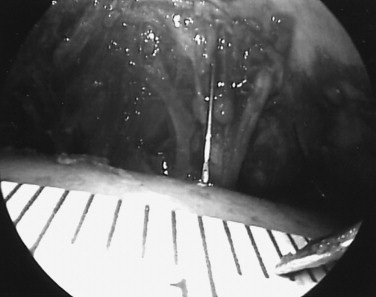
Nerve supply parallels arterial supply to some extent. The supratrochlear and supraorbital nerves, which account for most sensation to the forehead, exit the same foramina or notch as the same named blood vessels. These sensory nerves originate from the first division of the trigeminal nerve. The supraorbital nerve has two divisions after it emerges from the frontal bone: (1) the deep (or lateral) division that supplies the more lateral and posterior portion of the forehead and scalp ( Figure 26-3 ), and (2) the superficial (or medial) division that pierces the frontalis early in its course and runs superficial to the muscle, supplying sensation to the lower forehead and the mid-forehead along the mid-pupil line. The bony exit point of the supraorbital nerve is relatively consistent. The supraorbital foramen or notch typically is found within 1 mm of a line drawn in a sagittal plane tangential to the medial limbus ( Figure 26-4 ). This point can be marked on the skin of the brow to give the surgeon a reference point that reveals the exit point of this important structure ( Figure 26-5 ). The deep division has been known to exit as often as 10% of the time from another foramen that may be as high as 1.5 cm above the orbital rim. Therefore, some surgeons advocate that blind (non-endoscopic) inferior dissection from the scalp above should be performed only to within 2 cm of the orbital rims, and that should be followed by endoscopic guidance below this point to decrease the chances of nerve injury.

Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


