(1)
Canberra, ACT, Australia
Summary
Accurate diagnostic information leads to better clinical outcomes. Radiographic examinations will always form the backbone of a diagnostic workup confirming clinical signs and symptoms. Conventional plain film radiography and digital radiography have been proved to be invaluable tools in the modern endodontic practice. The technology of cone-beam computed tomography has evolved in recent times with previous astronomical costs no longer prohibiting the purchase of machines for the modern endodontic practice. The technology has been embraced by endodontists to aid in the diagnosis of endodontic pathosis and canal morphology, assessment of root and alveolar fracture, resorptive defect analysis, identification of non-endodontic pathology and pre-surgical assessment. The question still remains regarding possible medicolegal issues pertaining to the acquisition and interpretation of CBCT data. An alternative arrangement is to refer the patient to an imaging centre where the CBCT scan can be reported by a radiologist preventing the possibility of missing any additional pathology or life-threatening lesions.
Clinical Relevance
Endodontic diagnosis, treatment planning and outcome assessment are dependent on radiographic examinations. Peri-apical radiographs captured on conventional plain films or digital sensors provide limited information due to their two-dimensional nature and distortion from surrounding anatomical noise. Recently cone-beam computed tomography has been proposed as a viable alternative to overcome the disadvantages of conventional peri-apical radiography in the dental surgery. The clinician should be aware of not only the advantages and disadvantages of all techniques but also the radiological principle of doses as low as reasonably achievable (ALARA), thereby minimising any risk of ionising radiation to the patient.
12.1 Overview of Radiology and Endodontics
Professor Wilhelm Conrad Röntgen was a German physicist, who, on 8 November 1895, produced and detected electromagnetic radiation in a wavelength range [1]. This discovery has led to the use of x-rays that is an integral and essential tool used in modern endodontics. In 1899 Dr. Charles Edmund Kells was one of the first dentists to use x-rays and a lead wire placed in a fractured upper central incisor to determine the working length [2]. Radiography has provided useful information about the presence, location and extent of the peri-radicular lesion, anatomy of root canals, proximity of adjacent anatomical structures and determination of working length that enable cleaning, shaping and filling procedures to be carried out with a degree of certainty, simplicity and accuracy. Conventional intra-oral radiography, captured on x-ray films or digital sensors, has provided clinicians with a high-resolution imaging modality that has been used for many years [3]. Recently there has been considerable debate as to whether newer imaging techniques such as cone-beam computed tomography (CBCT) should be the new standard of care [4, 5]. The major concern regarding standard preoperative CBCT relates to the additional ionising radiation. The effective radiation dose to patients when using CBCT compared to conventional radiography is much higher, and the benefit to the patient must be outweighed by any potential risks in order to be justified. Radiation dose should be kept as low as reasonably achievable (ALARA) [6].
Conventional two-dimensional (2D) radiographs provide a cost-effective, high-resolution image, which continues to be the most popular method of imaging today [6]. According to the consensus report of the European Society of Endodontology, appropriate root canal treatment includes a radiographical control showing a prepared root canal tapered from crown to apex and filled completely without space between canal filling and canal walls [7]. However, the diagnostic potential of peri-apical radiographs is limited. Information may be difficult to interpret, especially when the anatomy and background pattern are complex [8]. Radiographic interpretation is limited since three-dimensional (3D) anatomy is interpreted on a two-dimensional view. The sagittal plane (bucco-lingual) is not observed [3]. Furthermore, when considering surgery, 2D radiographs do not give an accurate spatial relationship of the intended roots to treated and adjacent structures such as the inferior alveolar nerve, mental foramen or maxillary sinus [9].
Lesions of endodontic origin associated with peri-apices of teeth may not be demonstrated on conventional 2D films unless the cortical plate has been breached. If the lesion is confined to the cancellous bone, then it may not even be detected [10–12].
The long-cone paralleling technique is the technique of choice during endodontics minimising any distortions and enabling much greater reproducibility. A further x-ray taken at a different angle (mesial or distal parallax tube shift) may provide additional anatomical information limited by the conventional zero-degree projection of the 2D image [11, 13, 14].
The fastest available films consistent with satisfactory diagnostic results should be used when using plain film radiography. Intra-oral films of ISO speed group E, or faster, are preferred. The use of ‘instant process films’ should be limited to specific essential situations (e.g. during surgery or endodontics). In situations where ‘rapid images’ are routinely required, conventional film with rapid-processing chemistry will generally give better results than instant process films. Strict attention should be paid to correct and consistent film processing so as to produce good quality radiographs and avoid the necessity for examinations to be repeated. Where automatic processing is used, the processor should be properly cleaned and maintained. In the case of manual processing, the temperature of the developer should be checked prior to film processing and the development time adjusted in accordance with the film manufacturer’s instructions. The developer should be changed at regular intervals in accordance with the manufacturer’s instructions [15, 16].
In order to extract full diagnostic information from the films, it is essential to have dedicated viewing facilities. A specially designed light box should be installed in an area where the ambient lighting can be adjusted to appropriate levels. Suitable film masking should be used to optimise the viewing conditions by cutting out stray light. For viewing dense areas of a radiograph, the incorporation of a high intensity light source in the light box is recommended. The provision of magnification by a factor of two would be beneficial [15, 16].
Whenever practicable, techniques using film holders incorporating beam-aiming devices should be adopted for bitewing and peri-apical radiography. If rectangular collimation is being used, a beam-aiming device is essential for accurate alignment with the intra-oral film. Attention is drawn to the probable need for additional operator training in the use of film holders when moving from circular to rectangular collimation [15, 16].
Digital radiography has been available in dentistry for more than 25 years but has not completely replaced conventional film-based radiography. The main reasons cited for this appear to be due to the financial investment required [17]. The advantages of using a digital system include the ability to manipulate images allowing for better interpretation and correction of under- or overexposures optimising the image for the diagnostic purpose. Manufacturers often cite that the radiation dose the patient receives is reduced. However, the dose reduction is not as large as often quoted due to an increase in the number of radiographs taken due to the ease of remakes akin to digital systems [18].
In selecting digital equipment, it is necessary to ensure that the chosen system offers the sensor sizes that are clinically required. Sensor sizes should be available in a range that is comparable with dental film [15].
The sensitivity of the detector system has to be compatible with the x-ray set(s) for which it is to be used. Ideally the x-ray set should have an effectively constant operating potential with the ability to select sufficiently low exposure settings to enable the full extent of available dose savings to be realised [15].
Cone-beam computed tomography (CBCT) has been introduced to dental offices recently due to reduced costs and the size of the machines to produce undistorted 3D information of the maxillofacial skeleton with a substantially lower radiation dose compared to conventional CT [3]. 3D imaging software enables the CBCT scans to be viewed by the clinician in axial, coronal and sagittal 2D sections not seen with conventional peri-apical radiography. The software also allows 3D reconstruction of areas of interest further optimising the true clinical picture. A limited CBCT is often utilised for endodontic purposes with a limited field of view ranging from 40 to 100 mm [19].
The applications of CBCT and its obvious advantages over conventional plain film radiography in endodontics include the diagnosis of peri-apical disease [4, 20–23], assessment of internal and external resorption lesions [24–28], identification of perforations, root fractures and injuries sustained from dental trauma [29–32] and pre-surgical treatment planning [9, 33–37].
CBCT holds great promise for both patients and dentists, but it comes with potential pitfalls. Medicolegal issues pertaining to the acquisition and interpretation of CBCT data have been highlighted with questions being raised as to the necessity of a qualified radiologist being responsible for this. With careful planning and the use of appropriately qualified individuals to aid in interpretation, dentists can enhance their practice and best serve the interests of their patients [19, 38, 39]. However, its routine use is not recommended due to the higher radiation dose required equivalent to 4–15 panoramic radiographs in some cases [40].
Observation of healing after completion of endodontic therapy is by interpretation of periodic recall radiographs. The time frame of this healing process is poorly understood, but observational follow-up studies and clinical experience have shown that the majority of treated cases with chronic apical periodontitis show signs of healing within 1 year. Standard follow-up of 4 years has been recommended, and in some clinical cases, healing has been demonstrated several years beyond this [7, 41–43]. Success and failure of endodontic treatment are based on strict criteria.
Interpretation of radiographic findings related to the stage and extent of chronic apical periodontitis, both preoperatively and postoperatively, during the course of follow-up has been shown to have great variability amongst observers. This observer variability exists within and amongst different observers when trying to radiographically diagnose the presence of lesions in bone [44–49]. Several factors have been proposed for this variation including individual attitudes to treatment and the hypothesis that dentists’ behaviour is assumed to operate along a health continuum. Furthermore, general dentists and endodontists differ greatly in their treatment decisions and also the assessment of the probabilities of disease and future complications [50, 51].
Although radiographs are an indispensable diagnostic tool, the increased effective doses of common intra-oral and extra-oral imaging techniques are high enough to warrant reconsideration of means to reduce patients’ exposure [52]. Alternative imaging techniques have been investigated for their potential in detecting and diagnosing peri-apical lesions, including ultrasound real-time imaging [53] and magnetic resonance imaging [54], where the side effects of radiation are irrelevant. Nevertheless, conventional radiographic imaging techniques remain the gold standard at this time, and close adherence to recommended guidelines ensures that patients are protected, limiting adverse health outcomes. Every radiation dose of any magnitude can produce some level of detrimental effect that may include an increased risk to genetic mutations and cancers. With this in mind, ALARA (As Low As Reasonably Achievable) is a safety principle designed to minimize radiation doses, thereby protecting both staff and patients [55].
12.2 Standard Equipment
X-ray source
Intra-oral x-ray units can be used for both conventional radiography using plain film and digital radiography.
Film selection
For conventional intra-oral radiography, film speeds available are D-speed, E-speed and F-speed, with F-speed being the fastest. The use of a faster film results in up to a 50 % decrease in exposure to the patient without compromising diagnostic quality. Film speeds slower than E-speed should not be used for dental radiographs. Digital radiography consists of image plates or sensors, which are available in exactly the same sizes as conventional film.
Collimation
Collimation limits the amount of radiation, both primary and scattered, to which the patient is exposed. A rectangular collimator decreases the radiation dose by up to fivefold as compared to a circular one, so radiographic equipment should provide rectangular collimation for exposure of peri-apical and bitewing radiographs. The use of a long source-to-skin distance up to 40 cm, rather than shorter distances of 20 cm, decreases exposure to the patient by 10–25 %.
Beam filtration
The operating potential of x-ray machines affects the radiation dose and backscatter radiation. Higher voltages produce lower contrast images that allow for better separation of objects with differing densities. The operating potential of dental x-ray machines should range between 60 and 80 kVp.
Patient protection equipment
Lead aprons are patient protective equipment that minimises exposure of scattered radiation. If all radiation protection recommendations are implemented, then theoretically a lead apron should not be used. To prevent cracks from occurring in the leaded shield, practitioners should ensure that all leaded aprons are hung and not folded.
Film holders
Film holders that align the film precisely with the collimated beam are recommended for both peri-apical and bitewing radiographs reducing geometric distortion. Heat-sterilisable film-holding devices are recommended for optimal infection control. Dental practitioners should not hold the beam-aiming device during exposure. By eliminating the patient’s finger from the x-ray field and any potential for displacement of the film, these devices help to minimise retakes, reduce radiation exposure and make it easier for both the patient and clinician to properly position the film (see Fig. 12.1).
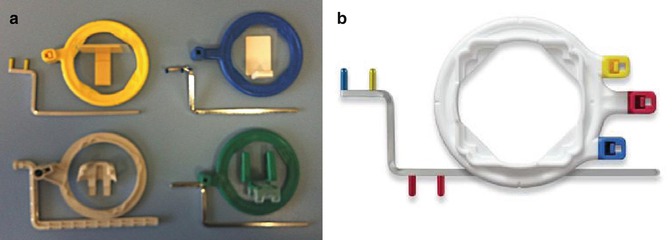
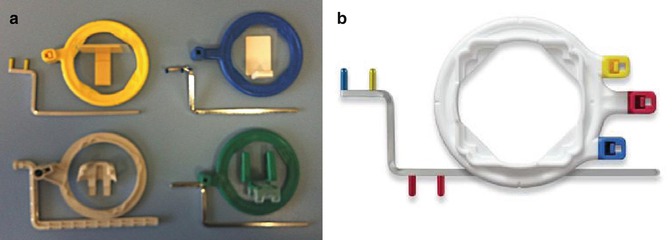
Fig. 12.1
Photographs demonstrating parallel film holder devices available commercially. Note (a) posterior (yellow), anterior (blue) and the endo-ray film holder (brown and green). (b) The XCP-ORA One ring and arm positioning system convenient for anterior (blue), posterior (yellow) and bitewing (red) radiographs
A number of commercial devices are available that position the film parallel and at various distances from the teeth including the Dunvale Snapex System, the EndoRay II endodontic film holder, the Uni-Bite film holder, the Snap-A-Ray film holder and the Snapex System film holder with aiming device. The EndoRay has been designed to help the clinician secure parallel working films with the rubber dam clamp in place. Generally these holders all have an x-ray beam-guiding device for proper beam/film relationship and a modified bite block and film holder for proper positioning over or around the rubber dam clamp.
Film exposure and processing
Exposure settings and film processing procedures affect the quality of the radiographic image. The operator must set the amperage and time settings for exposure of dental radiographs for optimal quality. The darkness of the resulting image (density) depends on the quantity and quality of radiation delivered, the size of the subject (thickness) and the developing and processing procedures.
Conventional plain film radiography requires strict processing according to manufacturer’s instructions regarding time, temperature and chemistry (developer and fixer solutions) (see Fig. 12.2). For the sake of expediency in the production of working films in endodontics, rapid-processing methods are available to produce relatively good films in less than 1–2 min. The contrast (degree of density) in using rapid-processing chemicals is lower than that achieved using conventional techniques; the radiographs have sufficient diagnostic quality to be used for treatment films that are obtained in less time. Rapid-processing solutions are available commercially, but they tend to vary in shelf life, in tank life and in the production of films of permanent quality.
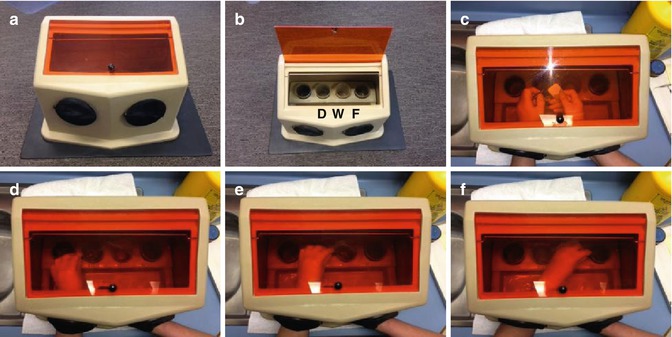
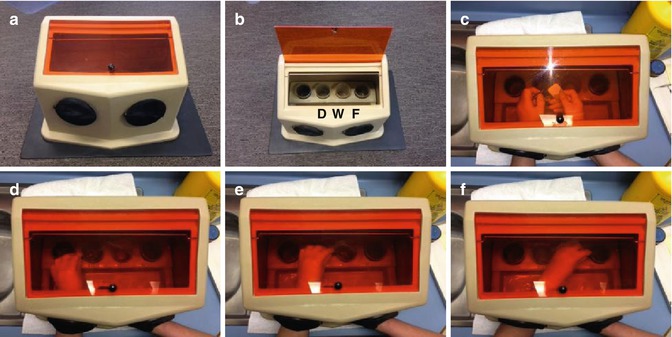
Fig. 12.2
Clinical photographs demonstrating film processing procedure using conventional plain film radiography. Note (a, b) manual chair-side film processing box with ruby red filter to ensure x-rays are developed under normal light safely. Plastic-covered cups hold developer, fixer and water inside (D, W, F). (c–f) Film processing procedure carried out according to time/temperature method. Manual film processing according consists of development, rinsing, fixing, washing and drying
It is recommended that after an image has been evaluated, it be returned to the fixer for 10 min more and then washed for 20 min and dried. This is to ensure that all radiographs taken during the course of endodontic treatment are preserved as a part of the patient’s permanent record.
Both lead foil from the film packet and film processing solutions (fixer solution) may contain hazardous waste, which must be disposed of appropriately.
Infection control
Universal standardised infection control policies must be adhered to when exposing dental radiographs. Prior to exposing the film, all equipment should be set out and the patient adjusted according to ideal chair and head position. During exposure of the film and handling of contaminated items, gloves should be worn at all times. Barrier-protected film and heat-sterilisable film holders should be used at all times. Digital sensors or plates should be covered with appropriate barrier protection. The film packet should be dried after exposure of the film. The protective barrier used in either conventional or digital radiography should be removed carefully to avoid further cross-contamination. The uncontaminated contents of the film packet or film sensor can then be handled without gloves or other precautions.
Image viewing
Clinicians should view the radiographs under suitable viewing conditions. An illuminated viewer is recommended for optimisation of high- and low-density areas on a conventional plain film radiograph. Magnification is recommended when needed.
Additional equipment in relation to digital radiography
A computer and high-resolution monitor are necessary to process and view digital images acquired. Often software bundled with the digital radiography system installed has basic image processing tools to allow for adjustment as well as annotation and measuring tools. It is recommended to ensure that the digital radiography software is compatible with the in-house practice management software used and whether integration of the radiographic images is feasible without causing network conflicts.
It may be necessary to purchase additional image receptor holders or positioning devices that have been adapted for a particular brand of digital image sensor used. For phosphor plate systems, conventional film-positioning devices such as Rinn XCP film-holding devices (Dentsply Rinn, Elgin) may be used. Devices such as the Snap-A-Ray film holder (Dentsply) or haemostats may damage the plates resulting in further expense and replacement.
12.3 Plain Film Radiography
Radiographs are an integral component to all phases of endodontic therapy. They aid in the diagnosis and the various treatment phases and help evaluate whether the treatment provided has been successful or failed. Root canal treatment relies on the clinical ability to obtain accurate radiographs; it is therefore necessary to master radiographic techniques that produce films that yield maximum diagnostic quality. Expertise in radiographic interpretation is obligatory for understanding both the limitations inherent with specific techniques and for the recognition of deviations from the norm, specifically non-odontogenic pathology that may mimic an endodontic lesion.
Conventional intra-oral radiographic film detects, stores and displays the radiographic image representing the x-ray shadow of patients’ internal structures. This is based on the interaction of x-ray photons with electrons of silver bromide crystals in the film emulsion. When the film has been exposed to x-ray photons, the silver halide crystals are sensitised producing a latent image. During the developing phase, the sensitised silver halide crystals are rendered black transforming the latent image into a visible one. The radiographic film produced may have a continuous density distribution, limited by the maximum and minimum values of density (black and white). Each optical density in between the maximum and minimum is related to the amount of light that passes through the film at a certain site. Based on this continuous density scale, conventional radiographic film-based images are known as analogue images.
Peri-apical radiography
Peri-apical radiography describes intra-oral techniques to show individual teeth and the surrounding structures around the apices and has been considered the primary radiograph of choice when carrying out endodontics. The paralleling and bisecting angle are two techniques commonly employed when using peri-apical radiography. The former is the preferred method of choice providing less image distortion, ensuring a high degree of reproducibility and reducing excess radiation to the patient and should always be attempted first. The latter can be reserved for patients unable to accommodate the positioning required for a true paralleling technique including patients with low palatal vaults and children. This technique is prone to image distortion and excessive radiation due to increased angulations resulting in unnecessary exposure of adjacent head and neck structures such as the eyes and thyroid gland.
Bitewing radiography
Parallel bitewing radiographs are also a useful adjunct in the initial endodontic workup providing additional information depicting the crowns of teeth, interproximal contacts and the height and relationship of the alveolar crest. Further diagnostic information such as the status of restorations, extent of caries, presence of pulp calcifications, external cervical root resorptive defects and coronal pulp chamber anatomy can be revealed. This information is helpful in not only determining the pre-endodontic assessment of the tooth and overall restorability but also aiding any future planning and correcting execution of any proposed root canal procedure (see Fig. 12.3).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses



