Dental professionals are often faced with challenges when formulating a treatment plan for patients presenting with a compromised tooth. A common dilemma involves the decision between tooth retention using endodontic treatment with crown restoration, and extraction and an implant-borne restoration. In this article the authors evaluate the 2 treatment modes, and observe that because outcomes are similar with both treatments, decisions should be based on the patient’s informed decision concerning restorability, costs associated with the procedures, esthetics, potential adverse outcomes, and ethical factors.
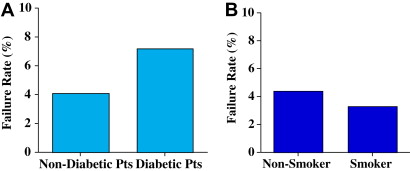
Dental professionals often face challenges when formulating a treatment plan for patients presenting with a compromised tooth, and have a duty to provide appropriate care for these patients to maintain dental health and esthetics. A common dilemma involves the decision between tooth retention using endodontic treatment with crown restoration, and extraction and an implant-borne restoration. Endodontic and implant restorations are performed daily by dentists and specialists. For endodontic treatment, estimates for the year 2000 were 30 million endodontic procedures annually (American Diabetes Association), while the number of patients receiving endosseous implants were estimated annually at 300,000 to 400,000 in 1996 and 910,000 in 2000 (Millennium Research Group). This may be a conservative estimate, according to the authors, because there has been an average growth rate increase of more than 40% annually for the 10-year period from 1997 to 2007 at the University of Minnesota ( Fig. 1 ). In the year 2008, for the first time, the authors had seen a drop in the number of patients receiving implants, and this may have been because of the economic downturn or the generational changes that were occurring (in that the authors are now seeing less completely edentulous patients, while their partially edentulous patient population continues to increase).
Outcomes
In deciding on an appropriate treatment plan, the outcomes of treatment play a key role. The definition of success for dental implant studies is often implant survival, whereas root canal studies measure the healing of existing disease and the occurrence of new disease. The use of lenient success criteria in implant studies may translate to higher success rates, whereas stringent criteria used in root canal studies may lead to lower success rates. To establish accurate comparisons, it is critical that the same outcome measures be used to assess endodontic and implant restorations. Because of these differences in the meanings of success, it is probable that survival rates will permit less biased, albeit less informative comparisons. Often the stringent criteria in past endodontic studies have labeled some cases as failures when they were healing.
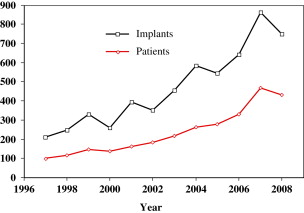
Other factors can also affect outcomes, such as the restorative impact with endodontics. It has been shown that unrestored endodontically treated teeth were significantly more likely (4 times) to undergo extraction. This restorative impact has been demonstrated by many investigators. Examples of how restorations on endodontically treated and severely damaged teeth fail are shown in Box 1 . Suggested restoration guidelines are shown in the flow chart shown in Fig. 2 . Before using the flow chart, preliminary steps need to be done, which are shown in Box 2 .
- 1.
Stress breaks anatomic crown at the neck of the tooth
- a.
Not strong enough ferrule (length and thickness)
- b.
Core/tooth structure interface fails, shell of tooth structure suffers from stress, tooth structure fracture, crown fracture
- a.
Solution : Unless there is adequate length and thickness of ferrule, extract the tooth. Unless there is enough tooth structure available for mechanical retention or bonding, use cast dowel and core.
- 2.
Cast dowel and core comes out from the root cement because it is not strong enough to withstand stress, especially under lateral or para-functional stress
Solution : Use resin cement for cast dowel and core and prefabricated post.
( Courtesy of Dr Wook-Jin Seong.)
- 1.
Complete evaluation of the whole mouth, in tandem with the particular tooth in question, so that a clear and comprehensive treatment plan can be formulated
- 2.
Data collection
- a.
Periodontal support
- b.
Quality of root canal treatment
- c.
Occlusal scheme
- d.
Para-function
- e.
Intended tooth function: single restoration or abutment of fixed partial denture, removable partial denture, and overdenture
- f.
Vertical space available for the crown
- a.
( Courtesy of Dr Wook-Jin Seong.)
When evaluating the quality of the root canal treatment, common misconceptions surround what can or cannot be addressed with retreatments, endodontic surgery, and other treatments. Unfortunately, many of these teeth are deemed hopeless when that is not the case.
Fig. 2 can be used as a guideline to assist in treatment planning, although it may not fit every scenario precisely.
Costs
In formulating patient treatment plans, costs often play an increasingly important role. Analysis of insurance data of 2005 concluded that restored single-tooth implants cost 75% to 90% more than similarly restored endodontic-treated teeth. Using mean United States fees, the implant restoration costs twice as much as endodontic restoration. Examination of treatment costs at university settings have shown that implants cost more than twice as much (230%) as similar endodontically restored teeth (Bowles WR, Drum MM, Eleazer PE, unpublished data, 2009). In addition, posttreatment complications are more common with implant restorations, and these problems may increase this cost difference.
Costs
In formulating patient treatment plans, costs often play an increasingly important role. Analysis of insurance data of 2005 concluded that restored single-tooth implants cost 75% to 90% more than similarly restored endodontic-treated teeth. Using mean United States fees, the implant restoration costs twice as much as endodontic restoration. Examination of treatment costs at university settings have shown that implants cost more than twice as much (230%) as similar endodontically restored teeth (Bowles WR, Drum MM, Eleazer PE, unpublished data, 2009). In addition, posttreatment complications are more common with implant restorations, and these problems may increase this cost difference.
New studies needed
Patients prefer that their dentists use the best techniques and materials available. These advances in endodontics and implant treatment make some older studies less relevant. Because advanced materials and techniques come into use, success rates may be affected, which suggests the need for new outcome studies. For example, the use of intracanal medicaments in endodontics has changed over time. Endodontic access openings are seldom left open, which allowed additional microbial contamination. A retrospective look at endodontic surgery using newer techniques and instruments (no root-end bevel, ultrasonic instruments) found a twofold increase in success rate compared with older methods (91.1% vs 44.2%). Endodontic treatment now includes the use of dental operating microscopes for better visibility, and hand instrumentation combined with nickel-titanium rotary instrumentation. Newer materials such as sustained-release antibacterial agents and new forms of mineral trioxide aggregate allow for potentially better treatment and call for additional outcome studies.
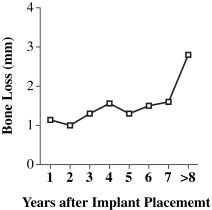
Advances in implants also continue to occur with improvements in such areas as shape, implant surface modifications, interface changes, and immediate placement. Previously, with implant placement 1.0 mm of bone loss during the first year of placement with an additional 0.1 mm annual loss was expected, but this can vary with newer implant designs and materials. Although longevity outcomes for implant restorations are high, one recently reported concern is that patients with dental implant restorations have significantly lower maximum bite forces and reduced chewing efficiency compared with contralateral natural teeth, or even with endodontic restorations.
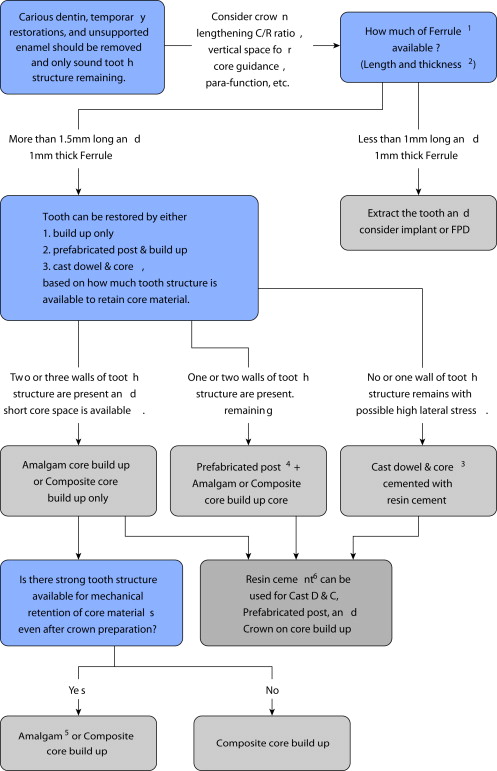
Using matched implant and endodontic restorations in patients, the authors found similar longevity outcomes for endodontic and implant restorations ( Fig. 3 ).
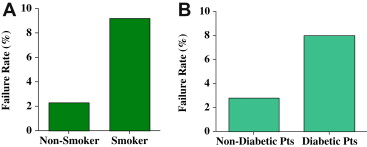
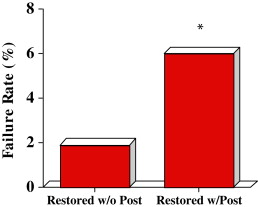
Several factors seem to be associated with higher failure rate of endodontic treatment. Smokers had an endodontic failure rate significantly (4 times) higher than nonsmokers ( Fig 4 A ), whereas diabetic patients had almost a threefold increase in their failure rate ( Fig 4 B). Smoking and diabetes have previously been found to be a risk indicator for apical periodontitis. In endodontic restorations, restoration with a post was also associated with a higher failure rate as seen in Fig 5 . Earlier studies had suggested that the presence of posts do not affect the outcome of endodontic treatment.
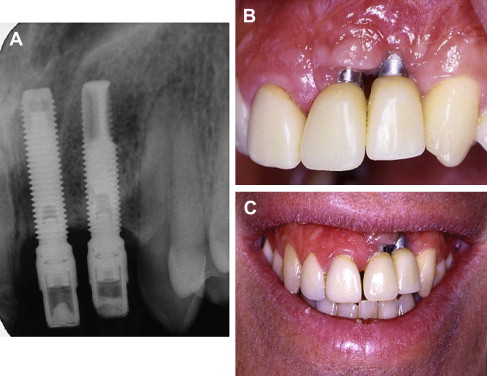
Outcomes for implant restorations can also be affected by several factors. Care must be taken to preserve the esthetics with anterior implants, while obtaining osseointegration of the implant ( Fig. 6 ). In earlier-implant patients, crestal bone loss occurred over the years; however, many newer implants may have decreased loss in the crestal bone. The authors have graphically presented the bone loss around implants over time ( Fig. 7 ) for patients in their current study. Significant bone loss can be observed in younger patients receiving implant treatment by the time they reach old age.
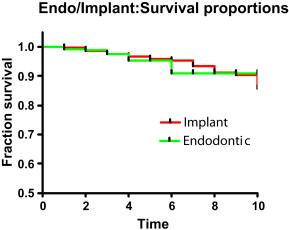
In the authors’ current study, implant restorations were less successful with diabetic patients, but did not seem to be affected by smoking, contrary to current literature results. Implant restorations in diabetic patients had a 7.2% failure rate, compared with a failure rate of 4.1% in nondiabetic patients ( Fig. 8 A ). Current literature suggests a 9% implant loss rate with controlled diabetes. There was no significant difference in failure rates with implant restorations in patients who smoked compared with those who did not smoke ( Fig. 8 B).