Protraction of mandibular posterior teeth requiring absolute anchorage has always been a challenge, especially when the space is located in the anterior region, since more teeth must be protracted. Traditionally, skeletal anchorage devices have been used for anchorage reinforcement during protraction. However, drawbacks such as requirement of a surgical step, inability to tolerate heavy forces, and patient willingness to undergo such surgical procedures can be limiting factors. Additionally, the mechanics involved can sometimes create undesirable side effects, thereby limiting their application in such situations. This report describes the use of a fixed functional appliance as an anchorage-reinforcement device for en-masse protraction of mandibular posterior teeth into a missing lateral incisor space.
Highlights
- 1.
En-masse protraction of mandibular posterior teeth was carried out.
- 2.
Dental effects of a fixed functional appliance were harnessed for anchorage reinforcement.
- 3.
Use of rigid stainless steel archwires assists in bodily protraction of the teeth.
Orthodontic mechanotherapy often entails treatment of patients with missing teeth. Treatment options for missing teeth commonly require either closing spaces or maintaining them for future restorative work. With endosseous implants generally the preferred method for restoring a missing tooth over fixed partial dentures, it is common for adolescents to have an extended retention or space maintenance phase for subsequent implant placement until facial growth and eruption of teeth have ceased. Often during the long retention phase, teeth may drift into the edentulous spaces, thereby increasing the risk for orthodontic retreatment for future implant placement.
Orthodontic space closure, although a viable alternative treatment option, is even more challenging than space maintenance because it commonly involves protraction of posterior teeth to close spaces. Anchorage control is often critical, and various forms of skeletal anchorage devices have been used for bearing the anchorage load; however, their usefulness for en-masse protraction of a segment of posterior teeth can be questioned. Failure of implants is not uncommon. Also, placement of such devices is technique sensitive: location, surgical skills, and the patient’s oral hygiene are critical factors for their successful placement. In addition, all patients may not necessarily be willing to have invasive procedures during orthodontic treatment. Therefore, it is desirable to develop alternative noninvasive methods that can provide absolute anchorage for en-masse protraction of posterior teeth.
Fixed functional appliances have traditionally been used for skeletal Class II correction. The effect of these appliances is reported to be primarily dentoalveolar, causing retroclination of maxillary incisors, proclination of mandibular incisors, distalization of maxillary teeth, and mesial movement of mandibular molars. The use of a fixed functional appliance and its effects on the dentoalveolar process are fully highlighted in this report. See Supplemental Materials for a short video presentation about this case report.
Diagnosis and etiology
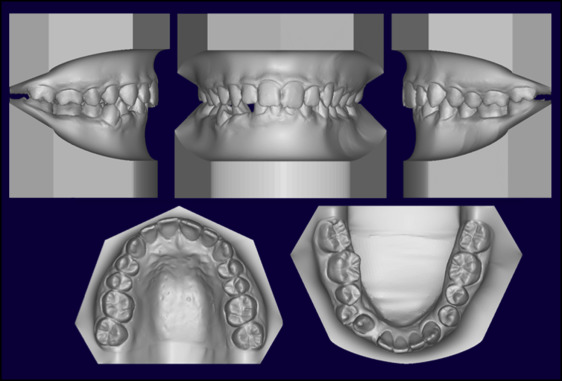
A boy, aged 13 years 8 months, came with a chief complaint of a missing tooth in the mandibular arch. He had a Class II subdivision (right) malocclusion on an underlying mild Class II skeletal base ( Table ) with a slightly forwardly placed maxilla and a normally placed mandible, an average growth pattern, and reduced lower facial height. In the mandibular arch, the patient had a congenitally missing right lateral incisor, severely rotated right canine, crossbite in relation to the right first premolars, spacing, a 2-mm overjet, and a 3-mm curve of Spee creating a 50% overbite.
| Pretreatment | Posttreatment | Retention | |
|---|---|---|---|
| SNA (°) | 87 | 87 | 88 |
| SNB (°) | 83 | 85 | 86 |
| ANB (°) | 5 | 2 | 2 |
| SN-GoGn (°) | 27 | 25 | 25 |
| FMA (°) | 23 | 20 | 20 |
| U1-SN (°) | 118 | 110 | 105 |
| U1-NA (°) | 18 | 23 | 17 |
| U1-NA (mm) | 3 | 3 | 1 |
| IMPA (°) | 94 | 92 | 92 |
| L1- NB (°) | 21 | 19 | 19 |
| U1-NB (mm) | 5 | 2 | 2 |
| E-line–upper lip (mm) | −4 | −6 | −6 |
| E-line–lower lip (mm) | −3 | −5 | −5 |
Extraorally, the patient had a mesoprosopic facial type with a convex soft tissue profile, right-angled nasolabial angle with 100% maxillary incisor display on smile. The upper midline was coincident with the facial midline, and no interlabial gap at rest was noted ( Figs 1-3 ).


Treatment objectives
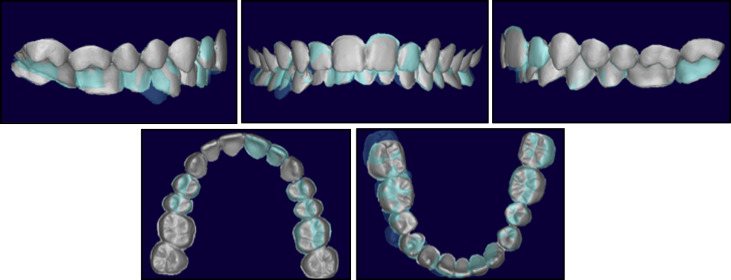
The treatment objectives were to close the space created by the missing lateral incisor by protraction of the posterior teeth so that the patient’s soft tissue profile could be maintained. Our goal was to create bilateral Class I molar and canine relationships. A diagnostic setup using emodel (GeoDigm Corporation, Falcon Heights, MN) was created to simulate the final outcome by protraction of the mandibular right posterior segment into the missing lateral incisor region ( Fig 4 ).
Treatment objectives
The treatment objectives were to close the space created by the missing lateral incisor by protraction of the posterior teeth so that the patient’s soft tissue profile could be maintained. Our goal was to create bilateral Class I molar and canine relationships. A diagnostic setup using emodel (GeoDigm Corporation, Falcon Heights, MN) was created to simulate the final outcome by protraction of the mandibular right posterior segment into the missing lateral incisor region ( Fig 4 ).
Treatment alternatives
The alternative treatment plan that was considered entailed maintaining the space for the missing lateral incisor and subsequent implant placement after the patient’s facial growth was completed. However, this required space maintenance for a long time. The patient’s parent did not agree to this treatment. Extractions of the maxillary first premolars and the mandibular left first premolar were also considered, but this could lead to adverse effects on the patient’s facial profile, which had to be maintained through treatment. Therefore, a nonextraction treatment plan involving protraction of the posterior teeth into the missing lateral incisor space was adopted.
Treatment progress
Treatment was initiated by bonding all teeth using a 0.022-in preadjusted edgewise appliance, with 6° of lingual crown torque on the mandibular anterior brackets. In the maxillary arch, initial leveling and alignment were done with 0.16-in nickel-titanium archwires. The archwire was gradually built up to a 0.021 × 0.0250-in stainless steel wire. In the mandibular arch, the initial leveling and alignment were done with 0.16-in nickel-titanium archwires. The archwire was gradually built up to a 0.019 × 0.0250-in stainless steel wire without engaging the severely rotated mandibular right canine. Elastic chains were applied from the buccal and lingual surfaces of the mandibular right canine to create a moment due to a couple to derotate the tooth ( Fig 5 ).
Once the canine was derotated and aligned, a crimpable hook was spot welded onto the 0.019 × 0.0250-in stainless steel archwire distal to the mandibular canine on the right side ( Fig 6 ). A passive Forsus Fatigue Resistant appliance (3M Unitek, Monrovia, Calif) (right side, 29; left side, 25) was placed bilaterally from the headgear tube in the maxillary arch to the mandibular archwire ( Fig 7 ). An elastomeric chain was placed from the molar tube on the mandibular arch to the crimpable hook delivering approximately 300 cN of force for en-masse protraction of the premolars and the first molar on the right side. The patient was recalled every 6 weeks, and the elastomeric chain was replaced to complete the space closure. The protraction phase lasted 10 months. During the space-closure phase, bracket breakages were found on 2 visits; this is a common side effect with a fixed functional appliance. However, instead of realigning the teeth, the brackets were bonded passively to continue with the space closure. The teeth were realigned during the finishing stages.




