Introduction
In this study, we compared the effectiveness of laser-aided circumferential supracrestal fiberotomy (CSF) and low-level laser therapy (LLLT) with conventional CSF in reducing relapse of corrected rotations.
Methods
The study included 24 patients who were at the finishing stage of orthodontic treatment and had at least 1 maxillary incisor with 30° to 70° of rotation before starting therapy. The subjects were divided into 4 groups by treatment: conventional CSF, Er:YAG laser-aided CSF, LLLT, and control. After alginate impressions were taken, the archwire was sectioned from the experimental incisors, and they were allowed to relapse. The second impression was taken 1 month later, and the degree and percentage of relapse were calculated in photographs taken from the dental models. Gingival recession, pocket depth, and pain were also measured in the CSF groups.
Results
The mean percentages of relapse were 9.7% in the conventional CSF, 12.7% in the Er:YAG laser-aided CSF, 11.7% in the LLLT, and 27.8% in the control groups. Relapse was significantly greater in the control than the experimental groups ( P <0.05), which were not statistically different from each other. The changes in sulcus depth and gingival recession were small and not significantly different among the CSF groups ( P >0.05), but pain intensity was greater in subjects who underwent conventional CSF ( P = 0.003).
Conclusions
Er:YAG laser-aided CSF proved to be an effective alternative to conventional CSF in reducing rotational relapse. LLLT with excessively high energy density was also as effective as the CSF procedures in alleviating relapse, at least in the short term.
Highlights
- •
Laser-aided fiberotomy is effective in diminishing relapse of rotations.
- •
Low-level laser therapy with high irradiation dosage alleviates rotational relapse in the short term.
- •
Pocket depth changes and gingival recession are similar in conventional and laser-aided supracrestal fiberotomy groups.
Relapse of corrected tooth rotations is a great challenge frequently facing orthodontists after orthodontic treatment. The slow turnover rate of supracrestal soft tissues is usually blamed for this phenomenon. Swanson et al reported an incidence of 48% for rotational relapse in patients 10 years out of retention. It has been demonstrated that the magnitude of relapse is in proportion to the severity of the initial rotation. Several strategies have been suggested as adjuncts to minimize relapse tendency of previously rotated teeth—eg, overrotation, early correction, and long-term retention—but the most applicable and efficacious method for this purpose is assumed to be circumferential supracrestal fiberotomy (CSF).
Introduced by Edwards in 1970, CSF consists of transecting the free gingival and transseptal fibers to increase their adaptation to the new tooth position. The effectiveness of the CSF procedure in reduction of periodontal relapse has been demonstrated in previous studies. However, some problems can occur during or after the CSF surgery, including bleeding, pain or discomfort, and the possibility of gingival recession and deepening of the gingival sulcus; these have resulted in relatively poor patient acceptability of the procedure. Therefore, alternative approaches such as CSF with electrosurgery or laser have been suggested.
Lasers have various applications in periodontal and orthodontic procedures, including removal of hyperplastic gingiva, exposure of impacted teeth, frenectomy, uncovering temporary anchorage devices, and CSF. It is believed that laser-aided CSF has numerous advantages compared with the conventional technique, including minimal pain and swelling, little or no bleeding, and lower probability of postoperative infection because the laser beam sterilizes the irradiated area.
Low-level laser therapy (LLLT) has been used in medicine and dentistry for more than 40 years. This treatment modality can have several biologic effects on cells and tissues, such as enhanced wound healing, reduced pain, and acceleration of the inflammation process. It is believed that the efficacy of LLLT depends on the dose applied. Arndt-Schultz proposed a therapeutic window (between 0.01 and 10 J/cm 2 ) at which the biostimulatory effects of low-power lasers are presented, whereas the inhibitory effects on physiologic activity can be observed at higher dosages. LLLT has been recently attempted in orthodontics for enhancing the stability of rotational movements, but the results of a previous study in this field were disappointing because significantly more relapse was observed in the LLLT group compared with the control group.
There are few studies regarding the efficacy of LLLT and laser-aided CSF in preventing rotational relapse, and the pathologic sequelae of laser CSF on the periodontium has not been investigated. Therefore, this study was conducted to (1) investigate the efficacy of the Er:YAG laser-aided CSF procedure and LLLT compared with conventional CSF in alleviating relapse of orthodontically corrected rotations, and (2) compare the magnitudes of pain, gingival recession, and pocket depth alteration after conventional and laser-aided CSF procedures.
Material and methods
The pretreatment maxillary occlusal photographs of patients at the finishing stage of orthodontic treatment were evaluated to find those with at least 1 (up to 4) rotated maxillary incisor(s) with 30° to 70° of rotation before orthodontic therapy. The patients were under treatment at the Department of Orthodontics, School of Dentistry, Mashhad University of Medical Sciences, Mashad, Iran, and at 1 private office in Mashhad, Iran. The participants had no systemic diseases and exhibited good oral hygiene. Patients with gingival inflammation or periodontal problems and those with proximal caries, deep caries extending to the cementoenamel junction, or anatomic abnormalities in the experimental teeth were excluded from the sample. The exclusion criteria also involved patients who consumed medicine that interrupted bone metabolism and those with conditions for which laser therapy could be contraindicated (eg, pregnancy). Twenty-four subjects with 47 rotated maxillary incisors satisfied the inclusion criteria and agreed to participate in the study. The patients (20 females, 4 males) ranged in age from 16 to 32 years (mean age, 24.5 ± 5.1 years). The study protocol was reviewed and approved by the ethics committee of Mashhad University of Medical Sciences, and an informed consent document was obtained from each participant after complete explanation of the treatment process. The subjects were divided into 4 groups by treatment: group 1 (conventional CSF), group 2 (Er:YAG laser-aided CSF), group 3 (LLLT), and group 4 (control).
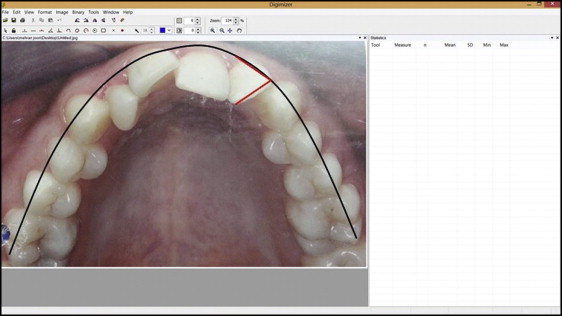
To measure the initial rotation of the maxillary incisors, the pretreatment (T0) occlusal photograph of the maxillary arch was scanned and imported into the Digimizer image analysis software (version 4.1.1.0; MedCalc Software, Mariakerke, Belgium). The esthetic line of occlusion was then drawn in each photograph, and the steep angle formed between a line passing through the incisal edge of the rotated incisor and the line tangent to the esthetic line of the dentition in the area of the rotated tooth was calculated ( Fig 1 ).
To assign teeth with severe rotations evenly in the study groups, the teeth were divided into 2 groups with 30° to 50° (moderate) or 51° to 70° (severe) rotations, as measured in the pretreatment occlusal photographs. The subjects were then randomly allocated into the 4 groups so that the teeth with moderate (31 teeth) or severe (16 teeth) rotations were evenly distributed among the groups. The mean (± standard deviation) degrees of initial rotation were 43.86° (±10.4°) in group 1, 48.12° (±8.01°) in group 2, 45.67° (±8.48°) in group 3, and 49.23° (±11.21°) in group 4. The procedures performed in the study groups were as follows.
Group 1 (conventional CSF) consisted of 6 patients with 13 rotated incisors who underwent conventional CSF surgery. Before the surgical procedure, the sulcus depth of each tooth was determined by a periodontal probe. The maximum depth of inserting the blade was considered as the sum of the sulcus depth and the biologic width (about 2 mm). Local anesthesia was used with infiltration of 2% lidocaine combined with 1:100,000 epinephrine, and then the CSF was performed by inserting a number 11.0 surgical blade into the gingival sulcus up to the level of the alveolar crest. The blade was moved around the tooth circumference to sever the free gingival and transseptal fibers. A periodontal pack was then placed on the tooth and remained for 24 hours. The patients were asked to maintain good oral hygiene. After the CSF procedure, the archwire was retained for 1 month to allow reattachment of the periodontal fibers in the ideal tooth position.
Group 2 (laser-aided CSF) included 6 subjects with 11 rotated teeth subjected to laser-aided fiberotomy. The device used was an Er:YAG laser (Smart 2940D; Deka Laser, Florence, Italy) emitting a wavelength of 2940 nm. The laser operated with 100 mJ of energy, pulse repetition rate of 10 Hz, and air and water spray. A contact handpiece with a 1.1-mm-diameter sapphire tip was used for tissue incision. The maximum depth of inserting the laser tip was determined similar to that in group 1. After local anesthesia, laser-aided CSF was performed by inserting the laser tip intrasulcularly at an angle of 10° to 15° to the radicular surface of the tooth. Since the light is irradiated from the end of the tip, the handpiece was moved in an apicocoronal direction during the CSF surgery. Little or no bleeding was observed, and no periodontal pack was inserted after the procedure. The patients were asked to maintain good oral hygiene. Similar to group 1, the archwire was retained for 1 month after surgery to allow reattachment of the gingival and periodontal fibers in the ideal tooth position.
Group 3 (LLLT) involved 12 rotated incisors in 6 patients who were treated with a low-level gallium-aluminum-arsenide diode laser (DD2 Control Unit; Thor, London, United Kingdom) to alleviate relapse of orthodontically corrected rotations. The laser emitted a wavelength of 810 nm and operated in continuous wave mode with maximum power of 200 mW. The laser probe was positioned in contact with gingival tissue in the coronal third of the root, and the irradiation was performed on 4 points around the tooth, including mesiobuccal, distobuccal, mesiolingual, and distolingual areas. The laser was irradiated for 50 seconds per point, and thus each tooth received 200 seconds of laser irradiation. The energy dose at each area was calculated to be 35.7 J/cm 2 , considering the surface area of 0.28 cm 2 for the probe. LLLT was performed twice a week for 4 weeks.
Group 4 (control) included 6 patients with 11 rotated incisors; no intervention to minimize relapse was performed.
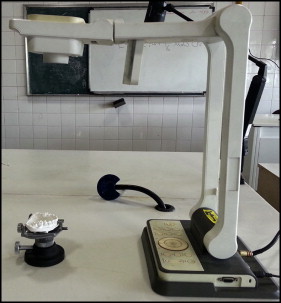
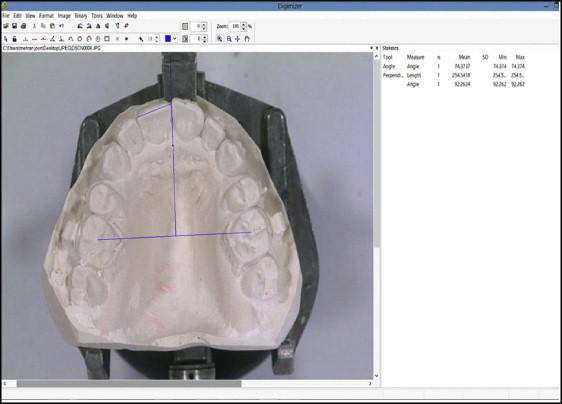
To determine the amount of relapse, the finishing archwire was removed from the maxilla, and an alginate impression was taken (T1). This initial impression was taken 1 month after performing conventional and laser-aided CSF in order to allow healing of supracrestal soft tissues following the surgical intervention. The impression was poured with orthodontic plaster, and the dental models were positioned on a prosthetic surveyor, so that the occlusal plane of the model was positioned horizontally. The dental models were then photographed at constant magnification with a digital camera (AVerMedia Technologies Inc, New Taipei City, Taiwan) that was fixed at a distance of 50 cm over the casts ( Fig 2 ). The images were then imported into the Digimizer software in which a reference line was drawn that was perpendicular to the line linking the central fossae of the first molars and passing through the midline of the maxillary dentition. The angle formed between the incisal edge line of the experimental incisor and the reference line was then calculated ( Fig 3 ) and rounded to 0.1°.
After taking the first impression, the archwire was sectioned from the experimental incisors, and they were allowed to relapse. The remaining teeth in the arch, however, were ligated to each other, and the archwire was maintained on them to prevent dental movements in other parts of the maxilla.
The second alginate impression was taken 30 days after removing the orthodontic archwire from the previously rotated teeth (T2; 2 months after CSF in groups 1 and 2), and the angle formed between the incisal edge of the tooth and the reference line was measured again. The mean relapse was reported as an absolute value calculated by subtracting the angle obtained at T1 from the corresponding value at T2. The percentage of relapse was also calculated relative to the initial angle of rotation according to the following formula:
The percentage of relapse = the amount of relapse the initial degree of rotation × 100
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


