Introduction
In this study, we tested the efficacy of a tooth sealant polish (Biscover LV; Bisco, Schaumberg, Ill) to prevent enamel demineralization (white spot lesions) for the full duration of orthodontic treatment with fixed appliances. The trial design was an alternating-tooth split-mouth design.
Methods
Patients starting treatment with bonded appliances in a private practice were enrolled. The 6 maxillary anterior teeth received the test sealant or no sealant. The nonblinded orthodontists visually examined the teeth immediately after debonding and rated the presence and severity of white spot lesions using a 4-point scale. The difference in incidence of white spot lesions on treated and control teeth was tested with multivariate binary logistic regression for repeated measures by using the generalized estimating equations approach.
Results
Sixty-five subjects were enrolled, and 3 were lost to follow-up, leaving 62 for analysis. There was a slightly lower incidence of white spot lesions on treated teeth (13.5%; 95% confidence interval, 8.6-18.4) compared with the control teeth (17.7%; 95% confidence interval, 12.4-23.7). This difference was statistically significant in the multivariate model (Wald chi-square, 5.07; df = 1; P = 0.024). The odds ratio was equal to 0.68 (95% confidence interval, 0.47-0.95) that treated teeth would show white spot lesions relative to the control teeth. White spot lesion severity was nearly the same for treated and control teeth (mean ± SD = 1.17 ± 0.47 and 1.20 ± 0.48, respectively; Wald chi-square, 3.03; df = 1; P = 0.082). No serious adverse effects were reported.
Conclusions
The sealant did not prevent all white spot lesions for the full duration of treatment. The sealant demonstrated a clinically small but statistically significant ability to prevent white spot lesions.
White spot lesions are unesthetic decalcifications of the tooth enamel; although they might remineralize after debonding, all too often they remain visible after the fixed appliances are removed. This creates a real concern for both patients and orthodontists whose goal is to improve esthetics. Most orthodontists take steps to minimize their occurrence, but white spots remain a problem in up to 50% of orthodontic patients. The use of fluoride is effective in reducing decalcification in susceptible patients and is routinely prescribed in various forms during orthodontic treatment. However, the rate of compliance is low. Fluoridated vs nonfluoridated composites for bonding orthodontic brackets and fluoride-releasing elastomerics have also been evaluated.
Although white spot lesions can occur on any teeth, they are most frequently seen on the facial surfaces of the maxillary lateral incisors and mandibular canines. The use of sealants in orthodontics for the prevention of decalcification is not new. However, previous studies have shown that most chemically cured sealants do not effectively seal smooth enamel surfaces because of oxygen inhibition of polymerization when the sealant is in contact with the air in a thin layer. Light-cured sealants have been shown in vitro to cure completely on smooth surfaces and prevent demineralization. However, a subsequent clinical study did not support the results of the in-vitro study. The sealants used previously were either unfilled or lightly filled. Also, most studies were in vitro; when they were in vivo, the follow-up duration was short. New highly filled sealants have been developed by manufacturers, who claim that they stand up to mechanical and chemical erosion by oral fluids and tooth brushing. Leizer et al found no statistically significant difference between a filled resin sealant and a nonfilled resin sealant in vivo.
The effectiveness of materials other than sealants has also been evaluated. A few, antibacterial monomer-containing adhesives, fluoride-containing adhesives, self-etching primers, fluoride varnishes, and MI Paste Plus, have shown some protection in the short term. The discovery of a material that does not depend on patient compliance and can protect the teeth through the entire duration of orthodontic treatment in a clinical setting would benefit patients and orthodontists alike.
To our knowledge, the efficacy of a sealant for preventing the formation of white spot lesions in vivo for the full duration of orthodontic treatment has not been tested. Biscover LV (Bisco, Schaumburg, Ill) was developed to totally eliminate the formation of the oxygen-inhibited layer by chemical means. It is a low-viscosity, light-cured resin formulation that leaves a smooth glazed finish on the tooth surface, exhibits low wear to abrasion, and does not adversely affect bond strength, even in the presence of saliva and blood. The specific aim of this study was to assess the efficacy of this sealant in the prevention of white spot lesions during orthodontic treatment. The hypothesis tested was that application of BisCover LV can prevent white spot lesions on treated teeth compared with untreated teeth over the full duration of fixed appliance therapy. The study took place in the private practices of orthodontists who are participants of the National Practice-Based Research Network of the University of Texas Health Science Center at San Antonio. These orthodontists in private practices are dedicated to the advancement of orthodontic knowledge and the improvement of orthodontic care through research.
Material and methods
The subjects of the study were 62 male and female patients starting orthodontic treatment with bonded appliances in the private practices of 5 orthodontists in the National Practice-Based Research Network. Eligibility criteria included (1) bonded brackets to be placed on all 6 anterior maxillary teeth (canine to canine), (2) all 6 anterior maxillary teeth fully erupted, and (3) age at entry to the study between 12 and 26 years. Exclusion criteria included (1) any of the study teeth missing, restored, carious, or malformed (eg, microdontia, enamel dysplasia); and (2) any of the study teeth affected by clinically visible white spots. Prospective patients were screened for eligibility and exclusion criteria during standard clinical examinations, and those who were eligible were invited to volunteer after receiving a full disclosure of all study procedures and risks. The study was approved by the institutional review board of the University of Texas Health Science Center at San Antonio, and each participating orthodontist completed a mandatory course in human research ethics. The principal investigator (J.P.H.) at the coordinating center filed all interim progress reports. All adult subjects gave their written informed consent to participate. Parents gave informed consent for their minor children to participate, and the children gave written informed assent.
Consistent with the goal of preventing all white spot lesions, the study was powered to detect a clinically large effect size. The projected sample size was based on a recent pilot study of private orthodontic practices in San Antonio. From the pilot study, we estimated that the incidence of white spot lesions on unsealed teeth would be approximately 31% (range, 0%-67%), and that the incidence on sealed teeth would be near zero. Under these assumptions, an exact sign test for paired proportions would provide statistical power greater than 0.99 when n = 100 and α = .01.
The test sealant was purchased commercially from the manufacturer with general funds provided by the Department of Orthodontics at the coordinating center and distributed to the participating orthodontists. The product was stored and used as recommended in the Biscover LV Material Safety Data Sheet dated August 30, 2006. The test sealant was applied as follows. The enamel surface was cleaned with a slurry of pumice and water. The entire enamel surface was etched for 30 seconds, rinsed with water for approximately 10 to 20 seconds, and dried thoroughly. A thin layer of the material was applied in 1 direction with a smooth stroke on the enamel surfaces of the test teeth with a brush applicator. The sealant was allowed to remain on the enamel surface for 15 seconds for evaporation and then light cured for 30 seconds with a light-emitting diode curing light with a minimum output of 500W/cm 2 at close range of 0 to 2 mm. The light intensity was verified by a radiometer. The brackets were then bonded to the teeth and light cured.
The study was executed with an alternating-tooth split-mouth design. The 6 maxillary anterior teeth were alternately assigned to receive the test sealant or to be bonded with only the primer normally used in the practice. The left canine was randomly assigned to be sealed with the test sealant or to remain unsealed. This method of assignment balanced the allocation of the test material to central incisors, lateral incisors, and canines, and also to the left and right halves of the dental arch. With this method, the allocation of individual teeth was not independently random and concealable. However, it prevented the clinician from controlling which treatment each tooth received and balanced the treatment over the 3 tooth types. Unlike some other sealants or polishes, the test sealant does not release fluoride, so crossover effects from sealed to control teeth was eliminated. Since our objective was to prevent the occurrence of all white spots for the full duration of treatment, the primary outcome measure was the presence of any white spots on the test sealant and control teeth at the end of treatment when the bonded appliances were removed.
Baseline data, collected before randomization, included age, sex, and self-reported ethnic group as well as clinical data concerning tooth preparation methods, brackets, adhesives, ligation methods, oral hygiene, and compliance. Subject recruitment and baseline data collection occurred between December 14, 2007, and September 16, 2008. These data were used to characterize the subject sample and the participating orthodontic practices, and in the secondary subgroup analyses.
Treatment allocation of the left canine was stratified by practice site. The coordinating center prepared a treatment allocation schedule for each practice with a computer algorithm ( www.randomization.com ). Each practice received a series of note cards, sealed in heavy opaque envelopes, that indicated whether the left canine would be a test or a control tooth. The envelopes were identified on the outside by a code corresponding to the practice site and a serial number that identified each subject in that practice, and this information was transferred to all study data collection forms by each practice.
This study placed no restrictions on the orthodontic care administered to the subjects. Consistent with the philosophy of practice-based research, the study orthodontists were free to use their typical treatment methods and free to alter treatment methods at any time as guided by their professional judgment about best care. The subjects were encouraged to brush their teeth on a regular schedule with a fluoridated tooth paste. Fluoride-containing adhesives or elastics were allowed if they were applied to all study teeth. If white spots appeared during the study, the orthodontists were allowed to intervene with fluoride treatments or other methods; the only restriction was that the treatment should be applied to the whole mouth or to all 6 study teeth. Behavior modification programs and incentives for oral hygiene were allowed. Methods used for prophylaxis and treatment of white spots were recorded, and their associations with outcomes were analyzed.
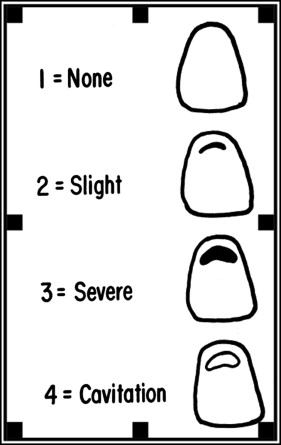
The a priori primary outcome measure was the incidence of white spot lesions immediately after debonding using the Gorelick scale ( Fig ). An incident white spot lesion was recorded if any tooth received a Gorelick scale score greater than 1.0. White spot lesion severity, defined as the sum of the Gorelick scores over the 6 teeth, was the secondary outcome measure. The adhesive and the sealant were removed from the teeth with a carbide friction grip debonding bur at slow speed. To ascertain that all adhesive was removed, the teeth were air dried and inspected for remaining adhesive. Then the unblinded orthodontist inspected the entire labial enamel surface of each study tooth under good light and a dry field to assess the presence or absence, and to grade the severity, of enamel demineralization using the Gorelick scale. Endpoint assessments occurred between December 17, 2009, and October 17, 2011.
Data were analyzed at the coordinating center using SPSS software (version 19; IBM, Armonk, NY). A generalized estimating equations approach was used to carry out a binary logistic regression analysis. The primary outcome measure was a binary variable coded 0 if no white spot lesions were present at the final examination and coded 1 if any white spot lesions were present. All analyses included the 185 teeth that received the sealant and the 186 control teeth; all teeth were analyzed within the condition to which they were randomized: ie, intention-to-treat analysis. The final analysis model was selected based on theoretical considerations and statistical goodness-of-fit indexes. The final model included the following independent variables. Treatment was included as a repeated measure variable coded as 1 if the tooth received sealant and coded as 0 if it was a control tooth. Tooth type was included as a categorical repeated measures variable with 3 levels corresponding to canines, lateral incisors, and central incisors. An exchangeable correlation matrix provided the best-fitting solution. Subject age in years, treatment duration in days from bonding to debonding, and oral hygiene rated on a 5-point scale by the orthodontist, with 1 as “one of the worst” and 5 as “one of the best,” were included as covariates to adjust for these risk factors. It was planned to examine the consistency of the treatment effect across the different practice settings; however, because practice B enrolled only 1 subject, this could not be estimated directly. This issue was approached in 2 ways, first by excluding practice B and second by pooling practices B and A. The effect of practice setting was estimated from these analysis models. In addition, although subjects were clustered within practices, and practices could be considered a random effect, the practices were treated as a fixed effect for this analysis because of the small number of participating practices and the small number of subjects enrolled by some practices.
There was 1 major protocol deviation in which 1 practice neglected to perform the final visual examination on its subjects. Therefore, white spot lesion incidence and severity were estimated from photographs taken at debonding for the 6 subjects of this practice.
Results
Three subjects were lost to follow-up because they moved away and transferred their care, leaving 62 subjects for analysis. Information about the participating orthodontic practices and the patients is shown in Tables I and II .
| Practice | Subjects enrolled | Subjects lost to follow-up | Practice location | Brackets | Adhesive | Ligatures | Fluoride |
|---|---|---|---|---|---|---|---|
| A | 30 | 1 moved away | New Jersey | Roth prescription, GAC | Grengloo, Ormco | GAC | None |
| B | 1 | None | Michigan | Innovation-C, GAC | Transbond, 3M Unitek | GAC | None |
| C | 19 | 2 moved away | Puerto Rico | Microarch V-slot, GAC | Assure, Reliance | American Orthodontics | Prevident, Colgate Oral Pharmaceutical |
| D | 6 | None | Texas | SPEED self-ligating bracket, SPEED | Transbond Plus, 3M Unitek | None | None |
| E | 9 | None | Texas | American edgewise straight wire, American Orthodontics | Transbond XT, 3M Unitek | Unitek | None |
| Age in years, mean ± SD (range) | |
| Children, n = 55 | 13.7 ± 1.8 (10.1-17.9) |
| Adults, n = 7 | 21.2 ± 2.6 (18.2-25.4) |
| Total | 14.6 ± 3.0 (10.1-25.4) |
| Sex, number (%) | |
| Male | 19 (30.6) |
| Female | 43 (69.4) |
| Race/ethnic group, number (%) | |
| African American | 14 (22.6) |
| Asian | 7 (11.3) |
| Hispanic/Latino | 22 (35.5) |
| Non Hispanic white | 17 (27.4) |
| Other | 2 (3.2) |
| Treatment duration in days, mean ± SD (range) | 799.6 ± 154.3 (497-1,176) |
| Hygiene, mean ± SD | 3.3 ± 1.2 |
| Compliance, mean ± SD | 3.3 ± 1.1 |
The full-analysis model is given in Table III . Taken over all teeth, there was a slightly lower incidence of white spot lesions on the treated teeth (rate, 13.5%; 95% confidence interval [CI], 8.6-18.4) compared with the control teeth (rate, 17.7%; 95% CI, 12.4-23.7; risk ratio, 0.763), but this difference was statistically significant after adjusting for the other variables in the model (Wald chi-square, 5.29; df = 1; P = 0.021). The odds ratio was equal to 0.661 (95% CI, 0.464-0.941) that treated teeth would show white spot lesions relative to the control teeth ( Table IV ). The white spot lesion severity, as indexed by the mean Gorelick score over all teeth, was nearly the same for the treated and the control teeth (mean ± SD, 1.17 ± 0.47 for treated teeth vs 1.20 ± 0.48 for control teeth; Wald chi-square, 3.03; df = 1; P = 0.082). Table IV displays the incidence and severity of white spot lesions for the test and control teeth.
| Effect | Regression parameter | SE | Wald chi-square | df | P value | Odds ratio | 95% Wald CI for odds ratio | |
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | |||||||
| Constant | −0.017 | 2.243 | ||||||
| Treatment: sealed vs unsealed teeth | −0.414 | 0.180 | 5.287 | 1 | .021 | 0.661 | 0.464 | 0.941 |
| Canine vs central incisor | −0.785 | 0.374 | 4.413 | 1 | .036 | 0.456 | 0.219 | 0.949 |
| Canine vs lateral incisor | −1.056 | 0.334 | 10.010 | 1 | .002 | 0.348 | 0.181 | 0.669 |
| Age | −0.262 | 0.091 | 8.286 | 1 | .004 | 0.770 | 0.644 | 0.920 |
| Treatment duration | 0.004 | 0.002 | 3.212 | 1 | .073 | 1.004 | 1.000 | 1.008 |
| Oral hygiene | 0.913 | 0.347 | 6.907 | 1 | .009 | 2.492 | 1.261 | 4.922 |
| Practice A vs E | 0.243 | 0.930 | 0.068 | 1 | .794 | 1.275 | 0.206 | 7.892 |
| Practice C vs E | 1.892 | 0.935 | 4.092 | 1 | .043 | 6.630 | 1.061 | 41.447 |
| Practice D vs E | 1.559 | 1.080 | 2.084 | 1 | .149 | 4.756 | 0.572 | 39.515 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


