Introduction
This prospective observational study evaluated changes in the 3-dimensional position and remodeling of the mandibular rami, condyles, and chin at splint removal and 1 year after mandibular advancementsurgery.
Methods
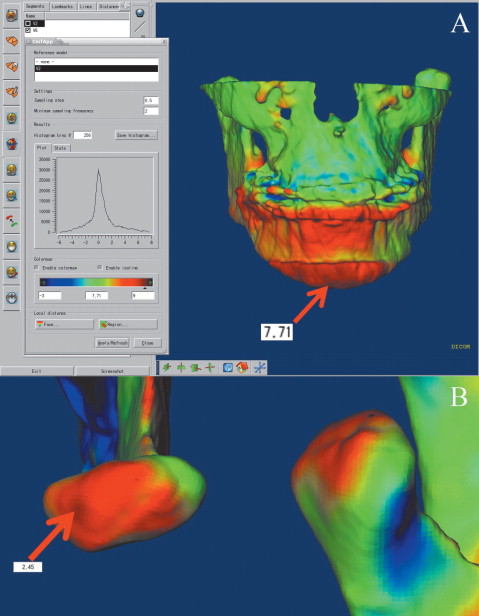
Presurgery, splint removal (4–6 weeks postsurgery), and 1-year postsurgery cone-beam computed tomography scans of 27 subjects were used. Superimposition on the cranial base was used to assess positional or remodeling changes in the anatomic regions of interest. Surface distance displacements were visually displayed and quantified by 3-dimensional color maps. A 1-sample t test was used to assess the average postsurgical changes of each region of interest. The level of significance was set at 0.05.
Results
After antero-inferior chin displacement with surgery (mean, 6.81 ± 3.2 mm at splint removal), the average 1-year postsurgery displacement was not statistically significant ( P = 0.44). Postsurgical adaptations greater than 2 mm were observed in 48% of the patients: 16% with an additional anterior-inferior displacement of the chin of 2 to 4 mm, and 4% with 4 mm; 20% hadpostero-superior movement of 2 to 4 mm, and 8% had postero-superior movement of 4 mm. The condyles tended to move, on average, 2 mm supero-posteriorly with surgery, and this small positional displacement was maintained 1 year postsurgery (right condyle, P = 0.58; left, P = 0.88). The rami exhibited outward (lateral) movements with surgery, with greater displacement of the inferior part of the rami (2 mm in 65% of the subjects). This torque of the ramus with surgery was stable 1 year postsurgery.
Conclusions
Three-dimensional assessment of skeletal changes with mandibular advancement surgery shows that nearly half of the patients have >2 mm change in chin position from splint removal to the 1-year follow-up, with approximately equal chances of anterior and posterior movement. Torque of the rami usually occurs with mandibular advancement surgery.
Read the full text online at: www.ajodo.org , pages S53.e1–S53.e12.
Editor’s comment
Cone-beam computed tomography (CBCT) has become a popular diagnostic tool in implant dentistry. Its 3-dimensional (3D) capabilities permit the surgeon to more accurately plan for implant replacement, especially in patients with questionable bony support. In the past, radiographic machines, such as the NewTom, iCAT, PreXion, Kodak, and others were too expensive for private practitioners. But today, these machines are affordable and are purchased by oral and maxillofacial surgeons to provide the information necessary to successfully and predictably place implants. With the growth of this radiographic technique, clinicians in private practice are now looking for other uses of this technology. Could CBCT be a valuable adjunct in the management of patients undergoing orthognathic surgery? If so, what types of information can be obtained from a 3D image that previously unavailable from conventional 2-dimensional (2D) radiographic techniques?
These authors compared the 3D changes in the position of the mandible in subjects who had undergone mandibular advancement surgery. CBCT scans were made before jaw surgery, immediately after surgery, and 1 year postoperatively. The authors superimposed the resulting skeletal maps to determine what happened to the chin, rami, and condyles. Although their methodology documented some interesting findings, they stated that their results corroborate results from previous studies with traditional 2D radiographic techniques—ie, submentovertex radiographs. Yes, there were differences in the chin position between the 3D and 2D radiographic interpretations, but does the increase in radiation exposure justify this limited increase in information? A study published in 2003 from the Department of Diagnostic Sciences from the same institution showed that a CBCT scan results in a 3- to 7-times increase in radiation exposure compared with a panoramic radiograph. So, with that in mind, I am posing 4 questions to the authors.
Vincent G. Kokich