Chapter 13
Ectopic eruption of maxillary first permanent molar
Ari Kupietzky and Jane A. Soxman
Introduction
A smooth transition from the primary to the permanent dentition is of utmost importance in managing a pediatric dental patient. Ectopic eruption (EE) of the maxillary first permanent molar is a common occurrence in the developing mixed dentition and is many times diagnosed first by the pediatric dentist.
EE is defined as a tooth erupting in an abnormal position or orientation (Gehm & Crespi, 1997). EE of the first permanent molar is a local disturbance characterized by eruption of the molar under the distal undercut of the second primary molar and its failure to erupt to the normal occlusal plane (Chintakanon & Boonpinon, 1998). The first permanent molar may become impacted and cease to erupt, causing premature resorption of the distobuccal root of the neighboring primary molar (Figures 13.1 and 13.2). Early correction of ectopically erupting maxillary first permanent molars is an integral part of interceptive orthodontics and is crucial for the proper development of a stable occlusion. If left untreated, EE may cause serious sequelae, including early loss of the second primary molar, space loss, and impaction of second premolars (Figure 13.3a). Future corrective treatment may be complicated, lengthy, costly, and may include the distalizing and uprighting of the permanent molar by use of headgear and fixed or removable appliances with subsequent long-term space maintenance (Figure 13.3b, 13.3c, and 13.3d).
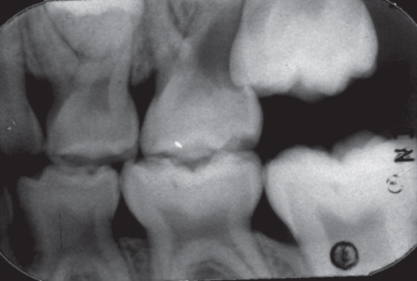
Figure 13.1 The first permanent molar may become impacted and cease to erupt, causing premature resorption of the neighboring primary molar as seen in routine bitewing radiograph.
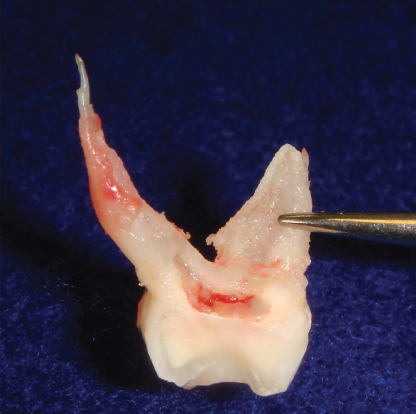
Figure 13.2 Extracted second primary molar with distobuccal root resorption.
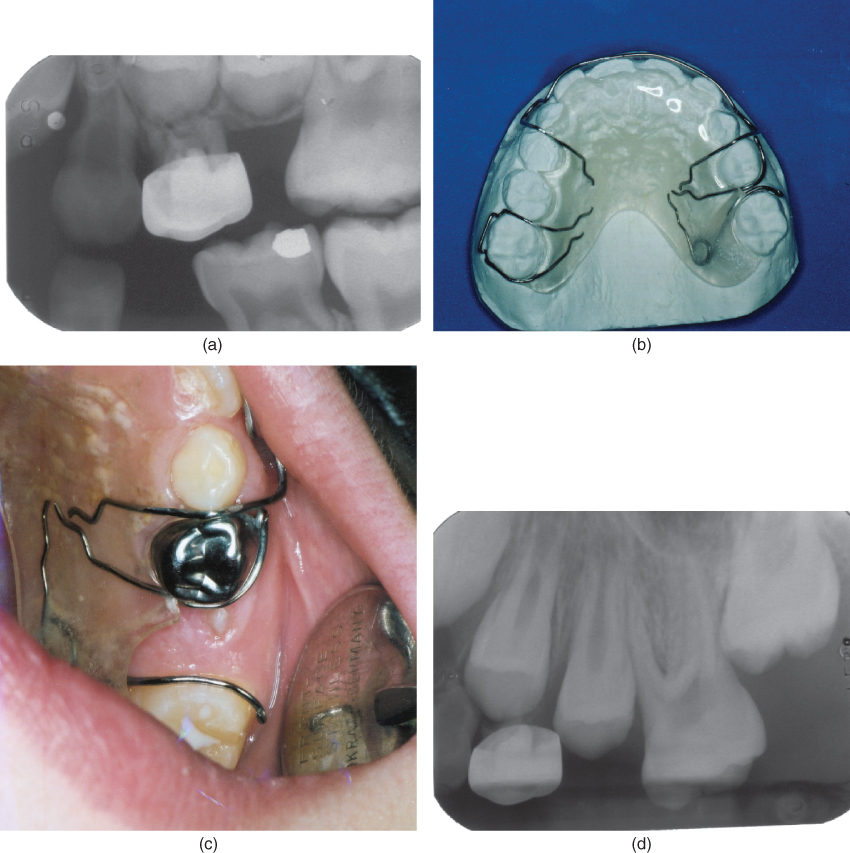
Figure 13.3 (a) If left untreated, EE may cause serious sequelae, including early loss of the second primary molar, space loss, and impaction of second premolars. (b) A removable appliance is used to distalize the permanent first molar and allow proper eruption of the second premolar. (c) Space has been regained allowing eruption of the blocked out tooth. (d) The periapical radiograph demonstrates eruption of the second premolar.
Treatment of EE includes a broad spectrum of procedures, including observation with follow-up, elastomer separation, disking the distal of the adjacent second primary molar, the distal brass wire separation, fixed or removable appliance therapy, or extraction of the second primary molar and subsequent space regaining followed by space maintenance.
Treatment modalities may be divided into two categories: interproximal wedging and distal tipping. The former type of treatment has traditionally been used in cases of minimal to intermediate impaction of the first permanent molar on the distal aspect of the second primary molar. When the impactions are severe, distal tipping techniques with or without second primary molar extraction have been indicated. Distal tipping techniques use fixed or removable appliances (examples include Humphrey appliance, sectioned wire with open coil spring, slingshot type appliances, hemisection of adjacent primary tooth, and others).
This chapter presents step-by-step procedures for treatment of EE with separators and a brief description of more complicated treatment modalities.
Identification
EE of the maxillary first permanent molar usually presents between the ages of 5 and 7 years on radiographic examination. The position of the unerupted first permanent molars on bitewing radiographs should be noted and documented in the patient’s chart, for example, first permanent molar in good position or not visualized (Figure 13.4).
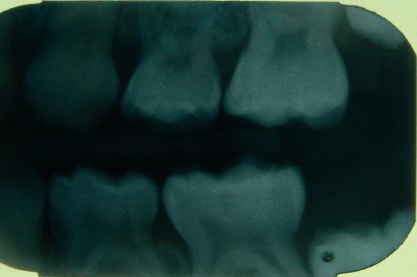
Figure 13.4 Bitewing radiograph of unerupted maxillary left first permanent molar in good position.
Observation
In many cases other than severe impaction, a conservative approach is suggested. Spontaneous correction occurs in 69.4% of cases and 14.3% progress to pulpal exposure of primary molar (Figure 13.5) (Barberia-Leache et al., 2005). The parent/guardian and child are advised to notify for discomfort, sinus tract and/or mobility of the second primary molar during the observation period (Figure 13.6).
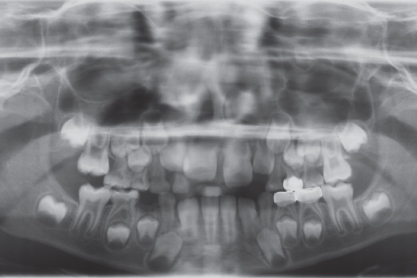
Figure 13.5 Panoramic radiograph showing impaction of maxillary right first permanent molar and spontaneous correction of ectopic maxillary left first permanent molar.
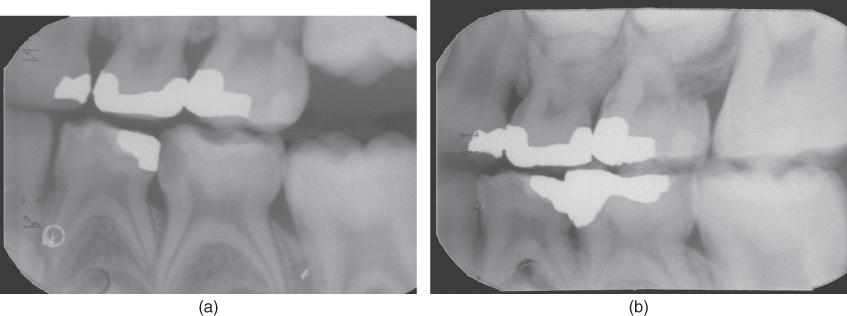
Figure 13.6 In many cases other than severe impaction, a conservative approach is suggested. (a) The unerupted maxillary first permanent molar in the bitewing radiograph was followed. (b) The molar erupted 6 months later without intervention.
Elastomer separators
The simplest method for correction uses a sequence of elastic separators. The technique can be used to resolve many of these impactions efficiently and effectively, with minimal patient discomfort (Cerny, 2003).
Conventional elastomeric ring separators come in two sizes: green – 3 mm diameter, 0.75 mm thick; blue – 4 mm diameter, 1 mm thick (Figure 13.7). These sizes are easy to fit and effective at moving teeth apart as much as 1 mm. However, in more severe impactions, a larger and thicker elastomer has been suggested (Cerny, 2003).
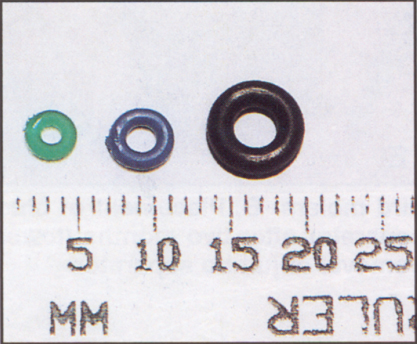
Figure 13.7 Elastomers of variable sizes: green (standard) – 3 mm diameter, 0.75 mm thick; blue (standard) – 4 mm diameter, 1 mm thick; black (jumbo) – 6 mm diameter, 2 mm thick.
(reprinted with permission from Cerny (2003))
Separators may be placed using separator pliers or floss (Figure 13.8a, 13.8b, 13.8c, 13.8d, and 13.8e).
Figure 13.8 (a) Separator plier. (b) Placing elastomer with separator plier. (c) Elastomer with floss. (d) Placing elastomer with floss. (e) Deimpacted maxillary first permanent molar.
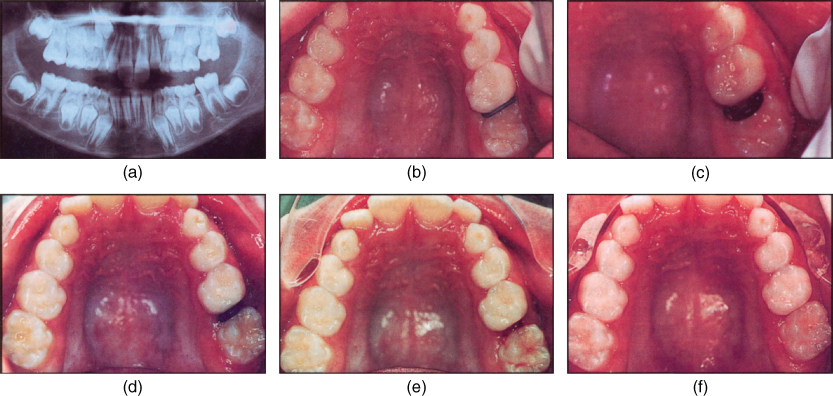
When used in sequence with the smaller orthodontic separators, “jumbo separators”: 6 mm diameter × 2 mm thick can move teeth apart as much as 2 mm, which is often enough to free many partially impacted molars (Figure 13.9a, 13.9b, 13.9c, 13.9d, 13.9e, and 13.9f). The jumbo separators should be soaked in hot water for 2–3 min before fitting. This makes them more pliable and less susceptible to fracture. Care should be taken not to overstretch the separator while attempting to place it between the two teeth. Stretching the separator by no more than one-third of its diameter allows easy placement, with little distortion and deactivation. Patients should be instructed to continue routine tooth brushing but not to floss or use toothpicks around the separators.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


