This case report describes the treatment of a girl, age 11 years 10 months, with a cleft lip and palate and a postsurgical scar. The clinical examination showed a concave profile, a retrusive maxilla, an asymmetric face, severe dental crowding, a Class III dental relationship, and a complete dental crossbite. Maxillary expansion and distraction, chincap, and high-pull headgear were used to moderate the skeletal discrepancy. These approaches, combined with tooth extraction and fixed orthodontic appliances, finally established a functional and esthetic occlusal relationship, normal overjet and overbite, and a well-balanced facial appearance.
A skeletal Class III malocclusion has been acknowledged to be the most challenging problem confronting orthodontists, especially when it is associated with cleft lip and palate. Primarily because of the unpredictable and potentially abnormal growth in patients with this skeletal pattern, treatment planning for most young patients with Class III malocclusion has been directed at growth modification. Although early treatment of these patients commonly achieves a relatively more normal jaw relationship, there have been few case reports of early intervention for a Class III malocclusion in a patient with cleft lip and palate.
Most patients with cleft lip and palate have altered and deficient maxillary growth as a result of postsurgical scar contraction or anatomic anomalies, and even may have dental arch deformities. Our aims of orthodontic treatment for these patients are to solve or moderate these deformities and to establish an ideal maxillomandibular relationship. This case report describes the treatment of a girl, age 11 years 10 months, with cleft lip and palate and a postsurgical scar, a Class III malocclusion, maxillary anterior crowding, and a complete dental crossbite.
Diagnosis and etiology
The girl and her parents came for orthodontic treatment with chief complaints of a crossbite and an unesthetic smile. She had received surgery at the age of 4 years and had no contraindication to orthodontic therapy. The pretreatment examination ( Fig 1 ) and the dental casts ( Fig 2 ) showed a concave profile (suggesting maxillary retrusion) and an asymmetric face (suggesting mandibular deviation).

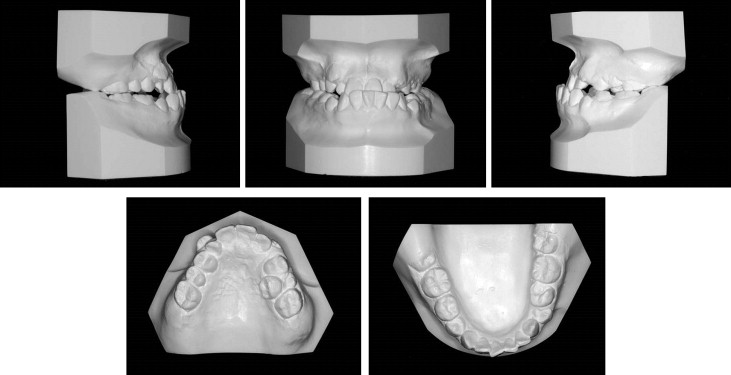
There was severe dental crowding (13 mm), and a left deciduous second molar remained in the maxilla; in the mandible, the deciduous second molars remained on both sides, with mild dental crowding. She had a Class III dental relationship on the left side and a Class I relationship on the right, as well as a complete dental crossbite. The maxillary midline deviated 3 mm to the right from the facial midline, and the mandibular midline was shifted 1 mm to the left.
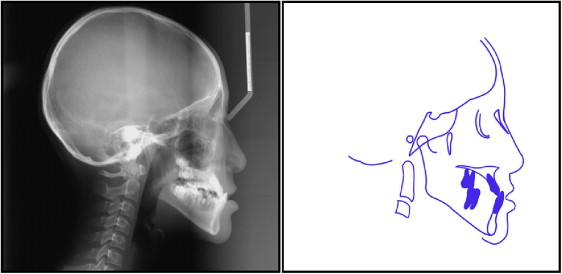
The cephalometric tracing ( Fig 3 ) and analysis ( Table ) showed a vertical skeletal pattern (MP-FH, 34°; PFH, 64.1°; AFH, 105.1°; FHI, 0.6) and a Class III skeletal relationship with maxillary retrusion (SNA, 81.2°; SNB, 84.1°; ANB, −2.9°). The mandibular incisors were retroclined (IMPA, 77.5°; 1.NB, 20°; 1-NB, 3.8 mm). The concave profile was due to a sagittally deficient maxilla (Z-angle, 79.6°; ULP, −2.8 mm; lower lip-E plane [LLP], 2.4 mm; nasolabial angle, 96°). Both the left and right second premolars were developing and could be seen on the panoramic radiograph ( Fig 4 ). The right mandibular ramus length was slightly shorter than that of the left side.
| Measurement | Average | Initial | Final | 2 years after treatment |
|---|---|---|---|---|
| Skeletal | ||||
| SNA (°) | 82.3 ± 3.5 | 79.8 | 82.1 | 82.3 |
| SNB (°) | 78.9 ± 3.5 | 83.6 | 82.8 | 82.2 |
| ANB (°) | 3.4 ± 1.8 | −3.8 | −0.7 | −0.1 |
| Convexity (°) | 1.6 ± 4.8 | −7.3 | −3.5 | −3.8 |
| MP-FH (°) | 28.8 ± 5.2 | 33.9 | 37.2 | 38.3 |
| Gonial angle (°) | 131.0 ± 5.6 | 133.6 | 133.7 | 133.4 |
| SL (mm) | 41.9 ± 6.2 | 45.5 | 45.3 | 44.8 |
| SE (mm) | 20.6 ± 2.7 | 15.7 | 14.5 | 14.9 |
| NP-FH (°) | 88.6 ± 3.2 | 89.4 | 86 | 85.7 |
| PFH (mm) | 45.0 | 63.2 | 69.9 | 69.8 |
| AFH (mm) | 64.0 | 105.4 | 111.5 | 113.3 |
| FHI (PFH/AFH) | 0.7 | 0.6 | 0.6 | 0.6 |
| Y-axis (°) | 65.4 ± 5.6 | 61.4 | 66.5 | 66.9 |
| Dental | ||||
| U1-FH (°) | 111.1 ± 5.5 | 115 | 112.9 | 111.1 |
| U1-L1 (°) | 120.3 ± 10.1 | 133.8 | 129.3 | 134.7 |
| FMIA (°) | 54.6 ± 6.5 | 66.7 | 64.4 | 65.8 |
| IMPA (°) | 96.3 ± 5.8 | 79.4 | 78.4 | 75.9 |
| 1.NB (°) | 31.0 ± 6.6 | 23 | 20.6 | 18.8 |
| 1-NB (mm) | 7.8 ± 2.4 | 5.1 | 4 | 3.6 |
| 1.NA (°) | 24.7 ± 5.2 | 30.7 | 27 | 27.2 |
| 1-NA (mm) | 6.2 ± 1.9 | 6 | 6.4 | 6.4 |
| Soft tissues | ||||
| Z-angle (°) | 69.11 ± 4.74 | 80.5 | 70.3 | 69.9 |
| Nasolabial angle (°) | 100 | 95 | 93 | 89 |
| ULP (mm) | −2.5 ± 1.5 | −2.7 | −4.0 | −3.1 |
| LLP (mm) | 2.6 ± 1.5 | 2.5 | −1.7 | −2.4 |

Treatment objectives
Since this patient had a cleft lip and palate with a Class III malocclusion and a vertical skeletal pattern, the realistic and ideal treatment objectives were to (1) correct the maxillomandibular skeletal discrepancy; (2) obtain a normalized, functional, and stable occlusion; (3) create satisfactory overbite and overjet; (4) align the maxillary and mandibular dentitions and correct the midline; and (5) improve the dental esthetics and provide a favorable facial profile.
Treatment objectives
Since this patient had a cleft lip and palate with a Class III malocclusion and a vertical skeletal pattern, the realistic and ideal treatment objectives were to (1) correct the maxillomandibular skeletal discrepancy; (2) obtain a normalized, functional, and stable occlusion; (3) create satisfactory overbite and overjet; (4) align the maxillary and mandibular dentitions and correct the midline; and (5) improve the dental esthetics and provide a favorable facial profile.
Treatment alternatives
All alternatives made during the diagnosis were presented to the patient and her parents. Because she still had some maxillomandibular growth potential to accomplish ideal treatment goals, a nonsurgical approach was considered to be the best treatment option.
For an 11-year-old girl with cleft lip and palate, fixed orthodontic appliances alone had limitations, and the assistance of some other dental specialties was required to camouflage certain skeletal and dental factors of her malocclusion and to help improve esthetics and function. The options considered included (1) maxillary and mandibular first premolar extractions, compensation mechanics, and further occlusal adjustment with Class III elastics; (2) rapid maxillary expansion and distraction as well as a high-pull chincap to moderate or correct the Class III skeletal relationship, with extraction of the maxillary and mandibular first premolars to correct the crowding, overjet, and anterior crossbite; and (3) combined therapy of orthodontic-orthognathic surgery after she reached 18 years old.
Treatment progress
Treatment began with maxillary expansion using a jackscrew expansion appliance soldered to 2 banded teeth per side ( Fig 5 , A ). The appliance was activated at a rate of 0.5 mm per day for 15 days, until the posterior crossbite had been moderated.




