Early Detection
and Treatment of
Eruption Problems
Tooth eruption is an occlusal physiologic movement of the tooth within the jaw from its developmental position to its functional position in the occlusal plane. Active eruption starts when crown formation is completed and the root begins to form. The eruption process moves the tooth toward its functioning position. Massler et al1 defined tooth eruption as the “movement of a tooth from its site of development within the alveolar process to its functional position in the oral cavity.”
An understanding of the mechanisms of eruptive tooth movement is essential in all areas of dentistry. In general, tooth eruption is a complex process that involves a regulated interrelationship of root genesis and cementogenesis. Bosshardt and Schroeder2 stated that prefunctional development of the roots of permanent teeth is a protracted phenomenon in humans and may continue for 5 to 7 years prior to emergence of the tooth in the oral cavity. Tooth eruption, which is a continuous process to maintain the vertical dimension of every individual, continues throughout life. Movement can be observed following occlusal wear or as overeruption when a tooth is unopposed.
Early orthodontic treatment affords clinicians the opportunity to use this phenomenon in young patients. With proper mechanics, the eruption process can be used to increase or control vertical dimension during tooth eruption in patients with an overbite or underbite. There are also situations in space management when the space and mesiodistal position of a tooth must be controlled and overeruption of opposing teeth must be prevented (if a tooth is congenitally missing or has been extracted in one arch).
Tooth buds and the alveolar process develop simultaneously, and when a crown is completed it is enclosed in a crypt within alveolar bone. When eruption and movement of the tooth start, localized bone resorption begins to produce an eruption pathway for the tooth. At the same time, bone starts to form to fill the space left behind by the moving crown and growing root. During this complex interaction of tooth movement and jaw growth, the teeth move in three-dimensional space to maintain their position in the growing jaw and to compensate for masticatory function.
Phases of Tooth Eruption
For convenient categorization and for descriptive purposes, physiologic tooth movement is described in three phases:
1. Pre-eruptive phase
2. Eruptive phase
3. Posteruptive phase
Pre-eruptive phase
The pre-eruptive phase starts with follicular growth when the crown is being formed within its bone crypt. Growing teeth move in various directions to maintain their position in the expanding jaws. These movements in permanent teeth are mainly the result of primary tooth eruption and alveolar growth.
Pre-eruptive movement within the crypt wall occurs during bone remodeling. When there is bone resorption on one side and bone apposition on the opposite side, the tooth germ moves bodily as a filling-in process. However, when eccentric growth takes place and only bone resorption occurs on one side, the shape of the crypt changes, and the tooth germ moves according to this shape.
Primary tooth germs are very small when they develop, have plenty of space in the developing jaw, and grow very rapidly. However, they become crowded; further jaw growth in all directions accommodates all tooth germs.
Successional tooth germs develop on the lingual aspect of their primary predecessors, in the same bony crypt, and as the jaw develops they shift from their positions. For example, the permanent incisors and canines eventually occupy a position lingual to the roots of their primary predecessors, and the premolar tooth germs are positioned between the divergent roots of the primary molars.
Permanent molar tooth germs, which have no predecessors, develop from a backward extension of dental lamina. Maxillary molar tooth germs develop first, with their occlusal surfaces facing distally, and after sufficient jaw growth they swing into normal inclination. Mandibular permanent molars develop with their axes showing a mesial inclination, which becomes vertical when sufficient jaw growth has occurred.
All movements in this phase take place within the crypts of the developing and growing crowns before root formation.
Eruptive phase
The eruptive, or prefunctional, phase begins with the initiation of root formation and ends when the teeth reach occlusal contact. The mechanisms of eruption for primary and permanent teeth are similar, and many histologic changes occur around the tooth structure to accommodate tooth eruption. These changes include the following:
• Root formation
• Development of the periodontal ligament, which develops only after root formation has been initiated (the periodontal ligament must be remodeled to accommodate continued eruptive tooth movement)
• Resorption of primary roots
• Resorption of overlying bone
Any disturbances during these histologic processes can disturb tooth eruption.
This stage of tooth eruption is a relatively rapid phase that lasts until the teeth reach the occlusal level. In a radiographic study, Shumaker3 observed that each tooth starts to move toward occlusion at approximately the time of crown completion. The interval from crown completion and the beginning of eruption until the tooth is in full occlusion is approximately 5 years for permanent teeth.
Posteruptive phase
The posteruptive, or functional, phase begins when the teeth reach occlusion. During this period the teeth continue to move occlusally, alveolar processes increase in height, roots continue to grow to accommodate jaw growth, alveolar bone density increases, and principal fibers of the periodontal ligament establish themselves. Posteruptive changes have been divided into three categories:
1. Juvenile occlusal equilibrium: This is a phase of very slow eruption that parallels the rate of vertical growth of jaws.
2. Circumpubertal occlusal eruptive spurt: This is the second phase of active eruption, coinciding with the skeletal growth spurt and compensatory alveolar growth to maintain the freeway space and increase lower facial height. This phase has a faster rate of eruption, which slows between the ages of 11 to 16 years as facial growth reaches maturity.
3. Adult occlusal equilibrium: This is an extremely slow rate of eruption that occurs throughout life, in order to maintain facial height in response to situations such as occlusal tooth wear or tooth loss in one arch and overeruption of the tooth in the opposing arch.
Mechanisms of Eruptive Tooth Movement
The mechanism of tooth eruption still is not fully understood, but a review of this subject leads to the conclusion that eruption is a multifactorial process. Several theories to explain tooth eruption have been proposed.
Root formation
Because tooth eruption coincides with root formation, some investigators, such as Massler et al,1 considered that root elongation is a force responsible for tooth eruption. Shumaker,3 in a radiographic study, indicated that eruption starts at approximately the time of crown completion. In a study of dogs, in which the tooth germs were removed and replaced with dead crown shells and synthetic substitutes, Marks and Cahill4 showed that the follicular changes and the path of eruption were no different from those seen in normally erupting teeth. They concluded that the tooth itself played no part in the eruptive process. Marks and Cahill4 described the movement of the teeth during eruption as a three-dimensional movement and concluded that root elongation cannot move the tooth in three dimensions; it may, however, accelerate eruption speed.
Through animal histologic experiments and root dissection, Berkovitz and Thomas5 also showed that eruption of rootless teeth continues in the same manner as eruption of teeth with normal roots. The normal eruption of teeth that had been subjected to irradiation and consequently had shortened root formation is another example.6
Considering the high position of the maxillary canine before eruption and the long distance it moves during eruption, this tooth would have a long root formation if the root were responsible for the eruption process, which is not the case.
Hydrostatic pressure
Some studies have demonstrated that a differential hydrostatic pressure exists between the tissues investing the crown and its apical extent (ie, higher tissue pressure or accumulation of tissue fluid in the apex during apex development pushes the tooth germ toward occlusion).
Van Hassel and McMinn,7 in a study of dogs, found that the tissue pressure apical to the erupting tooth was greater than that found occlusally and thus advocated the theory that tissue pressure generates an eruptive force. However, they did not demonstrate any association between the magnitude of the force and the rate of eruption. Surgical excision of the growing root and associated tissues and elimination of the periapical vasculature did not stop eruption.
In root-resected incisors of rats, Chiba and Ohshima8 investigated the effect of a single injection of colchicine and daily injections of hydrocortisone on eruption rate. The study found that the agents had opposite effects on tooth eruption; colchicine and hydrocortisone caused a marked reduction and a marked increase, respectively, in unimpeded eruption rates. Root-resected and normal, nonresected incisors responded identically to these two drugs, supporting the view that the eruptive process following root resection is physiologic. No direct evidence was found to confirm or refute the hydrostatic pressure or periodontal fibroblast hypothesis of tooth eruption.
Dental follicle
The soft tissue of the dental follicle, which is located between the bony crypt and unerupted crown, exhibits osteo-clastic activity and occlusal bone resorption and creates an eruption tunnel to facilitate eruption. Simultaneously, new bone forms to fill the space left behind the crown and growing root.
Marks9 studied crypt surfaces during eruption and confirmed the polarization of alveolar bone metabolism around a tooth with respect to both bone cells and mineralized surface topography. In experimental studies of tooth eruption, he showed that the dental follicle, the dense connective tissue investment of the tooth, is necessary for eruption and that neither bone resorption nor bone formation occurs without the adjacent part of the dental follicle.
Wise et al10 used scanning electron microscopy to study bone formation in the base of the alveolar crypt of the first molar in the rat as a potential motive force of tooth eruption. Results indicated that the motive force of tooth eruption is likely bone formation at the base of the alveolar crypt and that this osteogenesis may relate to production of bone morphogenetic protein 2 in the dental follicle.
Gubernaculum dentis
At an early stage, the primary tooth and its successor share one bony crypt, but eruption and alveolar growth cause the permanent bud to be located in an inferior crypt. The gubernaculum dentis attachment acts to maintain the relative position of the follicle within the alveolar process and to prevent the tooth from submerging; in addition, it acts as a guide for the path of eruption.
Cahill and Marks,11 through radiographic and histologic evaluation in dogs, studied the roles of the gubernaculum dentis, root formation, the tooth crown, and the dental follicle in prefunctional eruption of a mandibular premolar. They concluded that the dental follicle was the only one of these structures required for the coordinated enlargement of the eruption pathway and formation of bone in the base of the bony crypt.
Periodontal ligament
Two mechanisms have been suggested to support the theory that the periodontal ligament influences tooth eruption. One involves the maturation of fibers, and the other suggests that the periodontal ligament may function as myofibroblasts to induce tension, moving the tooth toward occlusion:
• As the collagen fibers of the intermediate plexus mature, they contract and, as they are vertically inclined, draw the tooth vertically.
• Recent studies report a contractile protein in some fibroblasts of periodontal ligament that act as muscle cells.
Ten Cate12 supported the theory that the periodontal ligament has a major role in determining tooth eruption. He stated that the periodontal ligament, which is derived from the dental follicle, provides the force required for eruption and that the cells responsible are the fibroblasts within the periodontal ligament, which have contractile potential.
In a discussion of the role of fibroblasts in the remodeling of periodontal ligament, Ten Cate et al13 explained the role of fibroblasts in phagocytosis during remodeling. According to these investigators, increased fibroblastic activity during eruption plays a key role in physiologic tooth movement. However Marks9 stated that a limited period of growth and the presence of a periodontal ligament do not assure tooth eruption.
Berkovitz14 favored Ten Cate et al’s theory13 of fibroblast contraction, although he recognized the limitations of in vitro tissue studies. He indicated that formation and renewal of the periodontal ligament are associated with the continuous eruption of permanent incisors in rodents.
Bone remodeling
Bone remodeling in the pre-eruptive phase is theorized to move teeth by selective deposition and resorption in the immediate neighborhood of the tooth. Brash15–18 proposed that the formation of bone apical to developing teeth is one mechanism for tooth eruption.
Marks and Cahill’s experiment4 in dogs showed that the dental follicle must be present for tooth eruption and that bone remodeling occurs around the erupting follicle, regardless of the presence or absence of a tooth crown. The investigators suggested that the remodeling process may be under the control of the dental follicle because the periodontal ligament, cementum, and alveolar bone proper are derivatives in part of the follicle, so that later events could be controlled by these and other related tissues.
Alveolar bone growth, tooth development, and eruption are interdependent phenomena, and bone formation itself is not sufficient for tooth eruption. Cleidocranial dysostosis (also known as cleidocranial dysplasia) is a good example of a disorder in which eruption is delayed, absent, or ectopic, despite the fact that bone formation is normal.
Cellular and Molecular Bases of Tooth Eruption
Review of the mechanisms of tooth eruption and exploration of the different proposals and hypotheses related to tooth eruption suggest that tooth eruption requires the presence of three important components: the dental follicle, alveolar bone resorption for creation of an eruption pathway, and alveolar bone formation at the base of the bony crypt. In order for a tooth to erupt, resorption of alveolar bone must take place to remove the overlying bone covering the tooth bud and open a pathway; then the tooth bud must erupt through the formed pathway through a biologic process, and alveolar bone must form at the base of the bony crypt.
Marks and Cahill4 stated that tooth eruption is a series of metabolic events in alveolar bone characterized by bone resorption and formation on opposite sides of the dental follicle; the tooth itself does not contribute to this process. The question is, what biologic process regulates both the osteoclastic activity and the osteogenesis needed for tooth eruption?
In a comparison between human premolars and rodent molars, Bosshardt and Schroeder2 used light and electron microscopy and various measurements to assess the development and repair of cementum during and after root formation and tooth eruption. They indicated that cementum is a highly responsive mineralized tissue, and its biologic activity is necessary for root integrity and for bringing and maintaining the tooth in its proper position. They added that cementum formation and periodontal fiber attachment in premolars are characterized by a long-lasting phase of prefunctional development and that initial cementogenesis and root development last an average of 5 to 7 years in human premolars.
Larson et al19 removed the external layer of the enamel organ (dental follicle) before eruption in 13 mandibular premolars in dogs and followed eruption clinically, radiographically, and histologically to determine the role of the enamel organ in eruption. They found that none of the teeth without dental follicles erupted, but three teeth from which the follicle was separated and then replaced did erupt. They concluded that the enamel organ cannot support tooth eruption without the dental follicle.
As mentioned earlier, Wise et al10 examined bone formation in the base of bony crypts as a potential motive force of tooth eruption. They used scanning electron microscopy to study the rat mandibular molar from postnatal days 3 to 18 and concluded that the motive force of tooth eruption is bone formation at the base of the alveolar crypt. They suggested that this osteogenesis may relate to production of bone morphogenetic protein 2 in the dental follicle.
In another study aimed at finding what mechanism regulates both osteoclastogenesis and osteogenesis, which molecules are needed to initiate this regulation, and which cells and tissues are involved in this process, Wise20 reported the existence of a major burst of osteoclastogenesis in the rat mandibular first molar at day 3 and a minor burst at day 10 postnatally. Therefore, the osteoclastogenesis and osteogenesis needed for eruption are regulated by differential gene expression in the dental follicle both chronologically and spatially.
Stages of Permanent Tooth Eruption
The process of tooth eruption is an organized sequence of events that starts when crown formation is completed and the root begins to form. During this process, the tooth moves from its crypt through bone and soft tissue to its functional position. Tooth emergence is a part of the eruption process that starts with the appearance of any part of the cusp or crown through the gingiva.
Philbrick et al21 demonstrated that the time interval from crown completion and the beginning of eruption to full occlusion of permanent teeth is approximately 5 years.
After a review of the literature, Suri et al22 described the process of eruption as a dynamic process encompassing completion of root development, establishment of the periodontium, and maintenance of a functional occlusion.
During this complicated process, jaw growth is also interacting with numerous skeletal growth changes, such as increase in size, change in shape, and change in position. Normal bone remodeling under the control of genetic and environmental factors is another process necessary for progression of tooth eruption, which is occurring within the jaws.
The exfoliation of primary teeth and eruption of permanent successors result from a series of complex, reciprocal interactions between the root and surrounding structures. These interactions are controlled by a series of biochemical and biologic events that occur under the influence of several genetic signals. All of these events are consecutive steps; every step is a prerequisite for the next to occur and facilitates normal permanent tooth eruption after primary tooth exfoliation.
The following are the consecutive steps for replacement of a primary tooth by a permanent successor that can be seen at a site of normal dental transition. These steps can be a useful guide in monitoring tooth eruption to detect problems and design a treatment plan accordingly:
1. Resorption of the primary tooth root
2. Lengthening of the permanent tooth root
3. Exfoliation of the primary crown
4. Resorption of overlying bone to clear the path of eruption
5. Bone apposition under the moving tooth germ to fill the space left behind
6. Alveolar vertical growth and increasing alveolar height according to vertical tooth eruption
7. Movement of the permanent tooth through bone
8. Piercing of the alveolar crest at two-thirds’ root formation
9. Piercing of the gingival margin at three-quarters’ root formation
10. Root completion after several months in occlusion
Early detection of developmental problems at their initial stage of development is the most important step in early intervention in orthodontics. Many dental anomalies arise during tooth formation and eruption, and recognition of these problems requires a thorough understanding of these developmental changes. Longitudinal panoramic radiograph monitoring of these changes can be very helpful in early detection of and intervention in these abnormalities (see chapter 3).
Factors That Can Disturb Tooth Eruption
Numerous in vivo animal experiments and radiographic studies in humans have been performed to better understand the process of tooth eruption. As previously mentioned, Cahill and Marks11 stated that tooth eruption is a series of metabolic events in alveolar bone, characterized by bone resorption and formation on opposite sides of the dental follicle, and that the tooth itself does not contribute to this process. In a molecular study, Wise and King23 revealed more precisely that eruption is a tightly coordinated process regulated by a series of signaling events between the dental follicle and the osteoblasts and osteoclasts found in the alveolar bone.
Any disruption in this process can affect normal tooth eruption; outcomes range from delayed eruption to a complete failure of eruption. These abnormalities can occur as part of a syndrome or as a nonsyndromic disorder (isolated or familial).
Defects in tooth formation and eruption have been attributed to three general factors, categorized as systemic factors, genetic factors, and local factors. These factors can disturb matrix formation or the calcification process of tooth formation, resulting in structural defects such as decalcification and demineralization of tooth structure or abnormal tooth form. These factors can also arrest tooth development (hypodontia) or cause extra bud formation (hyperdontia). Likewise, if the apposition-resorption mechanism in alveolar bone is defective for any reason, the eruption process can be affected. Depending on the stage of eruption, syndromic and nonsyndromic problems can range from delayed eruption to a complete failure of eruption, including tooth ankylosis, primary failure of eruption (PFE), secondary failure of eruption, transposition, ectopic eruption, and impaction.
There is variation in the normal chronologic range of eruption of primary and permanent teeth because ethnic, racial, sex, and individual variations can influence this phenomenon. However, attentiveness to severe deviations of eruption time, sequence, and other disturbances in the tooth eruption process is critical to the timing and selection of different orthodontic treatment modalities. The purpose of this discussion is to provide a review of etiologic factors affecting normal eruption processes and the pathogenesis and differential radiographic interpretation of impaired tooth eruption.
Systemic factors
Disturbances of endocrine glands have a profound effect on the entire body, including tooth eruption. Baume and Becks24 assessed the response of the incisors of rats to growth hormone and thyroxine and the combination of both. The growth hormone resulted in an increase in size without hastening the eruption rate. Thyroxine treatment increased tooth dimensions and accelerated the eruption rate 36% in the young group and 46% in the older group.
To elucidate the effects of parathyroid hormone–related protein (PTHrP) on osteoclast regulation, Philbrick et al21 established a primary culture of epithelial stellate reticulum cells and mesenchymal dental follicle cells surrounding the teeth. The addition of osteoclastogenesis inhibitory factor resulted in a decrease in the number of osteoclasts formed in the co-cultures, suggesting that osteoclast formation is mediated by osteoclast differentiation factor. They concluded that PTHrP seems to regulate osteoclast formation via mediation of the dental follicle, in a manner analogous to the osteoblast-mediated process in the peripheral skeleton.
Tse Mdo et al25 used hemidecortication to investigate the effect of thyroid hormone in rats. This procedure, which consists of removing one cerebral hemisphere and leaving the thalamus and hypothalamus intact, produced hypothyroidism. The investigators also found a significant decrease in the weekly eruption rate of the maxillary incisors and partial recovery after the administration of thyrotropin-releasing hormone in rats.
Congenital hypothyroidism
Congenital hypothyroidism, also known as cretinism, is the result of the absence or underdevelopment of the thyroid gland and insufficient levels of thyroid hormone at birth. Today hypothyroidism is routinely diagnosed and corrected at birth. If undetected and untreated, hypothyroidism causes mental deficiency and disproportionate dwarfism. In addition, development of the dentition is delayed in all stages, including primary tooth eruption, exfoliation, and eruption of permanent teeth. The teeth are usually normal in size but crowded.
Juvenile hypothyroidism (acquired hypothyroidism)
Juvenile hypothyroidism is the result of a malfunction of the thyroid gland that is usually seen around the age of 10 to 12 years. Because most of the growth has been completed by this age, the body disproportion is not present, as it is in congenital hypothyroidism, but some degree of obesity is found. Development of the dentition is slow, and delayed exfoliation and delayed permanent eruption are common.
Hypopituitarism
Pituitary dwarfism is the result of an early hypofunction of the pituitary gland. Delayed eruption of the dentition is characteristic in patients with hypopituitarism; the primary teeth may be retained throughout the life of the person.
Extraction of the primary teeth is not indicated, because eruption of the permanent teeth cannot be ensured. The dental arch has been reported to be smaller than normal; thus, it cannot accommodate all the teeth, and crowding develops. The roots of the teeth are shorter than normal in conditions of dwarfism, and the supporting structures are retarded in growth.
Achondrodysplasia (achondroplastic dwarfism)
Achondrodysplasia is an autosomal-dominant disorder that causes disproportionate dwarfism. In this abnormality, growth of cartilage, or endochondral ossification, is disturbed; thus, the secondary displacement of the nasomaxillary complex is insufficient, and consequently the upper face is retruded, and the bridge of the nose is depressed. The maxilla is deficient, with resultant crowding of the teeth and a tendency for a Class III sagittal relationship and open bite. The development of the dentition is slightly delayed.
Defects in development of cartilage, especially of long bones, result in arrested growth and dwarfism that are usually diagnosed in babies or children. The head is disproportionately large, although the trunk is normal in size. The fingers may be almost equal in length.
In a radiographic study of the jaws and teeth in a group of 48 individuals with pituitary dwarfism, Kosowicz and Rzymski26 found an absence of root resorption and delayed exfoliation of primary teeth, marked delay in eruption of the permanent teeth, deep retention of permanent teeth in the maxillary and mandibular sockets, small jaw size, and crowding.
Barbería Leache et al27 studied 50 children with growth deficit regarding their endocrine and dentition status. They planned to investigate the relationship between the chronology of tooth eruption and delayed growth, regardless of whether the delayed growth is associated with low genetic height or caused by hormones. They concluded that retardation in bone age does not necessarily imply retardation in the dentition.
Genetic factors
Eruption defects have been found to be a feature in many genetic disorders and syndromes, including cleidocranial dysostosis and Down syndrome. Both the sequence and timing of eruption seem to be largely genetically determined. The recent finding that the parathyroid hormone receptor 1 (PTH1R) gene can be a causative factor for familial cases of PFE28 suggests that other disturbances in tooth eruption may have a genetic etiology.
Cleidocranial dysostosis
Cleidocranial dysostosis is a condition that primarily affects the development of the bones and teeth. Depending on the severity of the problem, signs and symptoms of cleidocranial dysostosis can vary widely, even within the same members of the family. Cleidocranial dysostosis occurs in approximately one individual per million worldwide.
Individuals with this syndrome usually have underdeveloped or absent collarbones (clavicles). As a result, their shoulders are narrow and sloping, and they can bring their shoulders unusually close together in front of the body. Delayed closure of cranial sutures and fontanels is another characteristic of this condition. Fontanels that usually close in early childhood may remain open into adulthood in people with this disorder.
Researchers believe that the RUNX2 protein acts as a master switch, regulating a number of other genes involved in the development of cells that build osteoblasts for bone formation. This protein is essential for osteoblastic differentiation and skeletal morphogenesis. It is believed that the RUNX2 gene provides instructions for making a protein that is involved in bone and cartilage development and maintenance.29
In individuals with cleidocranial dysostosis, the development of the dentition is delayed, resulting from delayed resorption of the primary teeth, and delayed eruption of the permanent teeth is common. Retarded eruption, failure of eruption, impaction of multiple teeth, the presence of supernumerary teeth, and the absence of other teeth are other dental problems that complicate occlusion.
Down syndrome
Down syndrome, or trisomy 21 syndrome, is a congenital anomaly. The cause of this syndrome is the presence of three copies of chromosome 21 rather than the normal two (diploid).
In patients with Down syndrome, delayed eruption of the teeth is common. Sometimes the first primary teeth may not appear until the individual is 2 years old, and the primary dentition may be completed at 5 years of age. The eruption often follows an abnormal sequence, and some of the primary teeth may be retained until age 15 years.
Because of the special characteristics of facial patterns, diagnosis is not difficult. The bridge of the nose is more depressed than normal, the orbits are small, and the eyes slope upward.
The tongue tends to be larger than normal and is usually protruded because the mandible is smaller.
Another characteristic of Down syndrome in most children is mental disability in the mild-to-moderate range.
Local factors
Many local factors can cause defects of tooth eruption. These defects can be classified as nonsyndromic types of tooth eruption disorders. The first step in early intervention in and treatment of these types of eruption problems is differential diagnosis and understanding of the initial cause of the problem. For example, lack of eruption can result from an obvious cause, such as inadequate arch length, or it can represent a PFE with many possible causes.
Examples of local factors that can interfere with normal eruption processes include supernumerary teeth, odontomas, cysts, other pathologic conditions, primary tooth ankylosis, remaining primary tooth roots, fibrotic soft tissue, bone barriers, lack of space due to early primary tooth loss, overretained primary teeth, primary periapical lesions that may hasten permanent eruption, or habits and muscle dysfunction. In addition, extraction of primary teeth has some effect on the eruption of their permanent successors.
In a study of 874 children, Gron30 observed that tooth emergence is associated more closely with the stage of root formation than with the chronologic or skeletal age of the child. By the time of clinical emergence, approximately three-quarters of root formation has occurred. Teeth reach occlusion before root development is complete.
Posen31 reviewed records of children with unilateral extraction of primary molars. He reported that eruption of premolars is delayed when primary molars are extracted by age 4 or 5 years. Delayed eruption is decreased when primary molars are lost after age 5 years. He also found that a significant acceleration of premolar eruption occurs when primary molars are lost at 8, 9, and 10 years of age.
Types of Eruption Disturbance
Before any treatment is planned for eruption disorders, the type of problem and the etiologic factors disrupting normal eruption must be determined. Eruption disturbances can be broadly classified into two general types:
1. Disturbances related to the time of eruption, such as delayed or premature eruption or failure of eruption
2. Disturbances related to the position of the affected tooth, such as ectopic eruption, tooth transpositions, and impactions
Box 10-1 lists different eruptive disturbances that can result from different systemic or local factors.
| Box 10-1 | Classification of eruptive disturbances |
| Disruptions in timing • Delayed tooth eruption • Early exfoliation of primary teeth and premature eruption of permanent teeth • Failure of eruption (PFE and secondary failure of eruption) • Retarded tooth development • Abnormal sequence of eruption |
Disruptions in position • Ectopic eruption • Transposition • Impaction • Ankylosis |
Delayed Tooth Eruption
Emergence that is outside the normal chronologic range of eruption includes delayed or early types of tooth eruption. According to numerous population studies conducted over the past century, there are variations in dental chronology based on race, ethnicity, and sex as well as environmental factors. Therefore, eruption that is early or delayed by a few months is not harmful unless there are local or systemic problems preventing normal eruption.
Delayed tooth eruption (DTE) is a common clinical finding that can occur in both the primary and permanent dentitions as a localized condition caused by local factors or as a sign of a generalized condition caused by systemic or genetic factors. Eruption of primary teeth usually occurs around 6 to 8 months of age, but, because of genetic or constitutional factors, the dentition sometimes may be delayed up to 1 year. A 1-year-old child with no primary teeth cannot be ignored and must be assessed for the possibility of some systemic disorder or syndromic conditions.
In such children, if there is no evidence of any ectopic tooth position, physical obstruction, or structural defect of tooth and the eruption status is within normal limits, periodic observation is the best treatment option to follow. However, any clinically detected instance of early or late eruption that is beyond the chronologic norms of emergence must be evaluated and monitored radiographically, especially if it is asymmetric. This condition must not be ignored, especially if eruption is delayed more than 10 months beyond the normal chronologic standard of emergence.
Timely screening and follow-up by the practitioner can prevent or minimize consequences that can develop at a later age and affect the patient’s dentition and health. Longitudinal panoramic radiograph monitoring of different stages of the dentition can be very helpful in early detection of and intervention in these abnormalities.
Etiology
There is considerable controversy regarding the terminology and pathogenesis of DTE. Suri et al22 published a table listing the terminology used for DTE. These terms include primary retention, embedded teeth, late eruption, retarded eruption, arrested eruption, impaired eruption, and others. Box 10-2 lists causes of delayed eruption in both the primary and permanent dentitions.
| Box 10-2 | Causes of delayed eruption |
| Primary teeth • Constitutional delay • Vitamin D deficiency in rickets (affects calcium metabolism, causing delayed eruption of teeth and bone abnormalities) • Hypothyroidism (low synthesis of thyroid hormone causes delayed development, including delayed eruption of teeth) • Hypopituitarism (results in developmental delay and DTE) • Cleidocranial dysostosis • Gardner syndrome • Apert syndrome • Down syndrome • Cerebral palsy • Protein-energy malnutrition, or protein-calorie malnutrition (a form of malnutrition caused by inadequate protein intake that occurs most frequently in infants and young children and is the leading cause of death in children in some developing countries) |
Permanent teeth • All of the factors that cause delayed emergence of primary teeth can also cause delayed emergence of permanent teeth • Crowding of the jaw and space deficiency • Supernumerary teeth and odontomas • Odontogenic cysts or other pathologic lesions • Overretained primary teeth or remaining roots • Tooth deformity and defective tooth development • Sclerotic gingiva or bone barrier covering the tooth |
Diagnostic procedures
Diagnostic procedures for DTE consist of careful intraoral and extraoral examinations, assessment of medical and dental histories, and radiographic evaluation. As mentioned earlier, longitudinal panoramic radiograph monitoring can help in early detection and differential diagnosis of disrupted tooth eruption before its complete development.
The patient’s medical and family histories and information related to eruption problems of the patient and close relatives are very important parts of the examination. A wide variety of disorders have been reported in association with DTE.
Clinical examination
Clinical examination must begin with the overall physical evaluation of the patient. For example, the presence of syndromes is usually obvious, but in patients with mild forms only a careful examination can reveal abnormalities and alert the clinician to perform further investigation if needed.
Specific oral examination
Specific oral examinations should include inspection, palpation, percussion, and necessary radiographic examinations to assess tooth eruption problems. Inspection includes evaluation of the number and morphology of the teeth present by assessing tooth counts, eruption timing, and eruption sequence.
The examination must also include clinical inspection of the alveolar ridge both buccally and lingually. The size and shape of the alveolar ridges usually show the characteristic bulge of a tooth in the process of eruption and can help to reveal DTE. A thin alveolar ridge indicates the absence of teeth in the area close to the ridge, and a wide and full alveolar ridge indicates the presence of a tooth. Palpation of the ridge can indicate the condition of an unerupted tooth, whether it is in the bone or is close to piercing the soft tissue. Careful observation and palpation of the alveolar ridges and soft tissue can also reveal the presence of swelling, scars, and fibrous or dense tissue.
Another important component of intraoral evaluation is assessment of the general tooth eruption pattern in the mandible and maxilla and especially comparison of the left and right segments of each arch. Any asymmetric pattern of eruption, including overretained primary teeth or asymmetric eruption of the permanent dentition on the left and right sides of the arch (more than 6 months’ difference), can be an important sign of eruption problems (Figs 10-1 and 10-2).
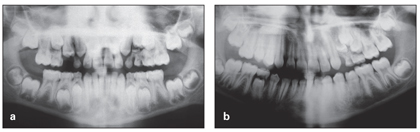
Fig 10-1 (a) Developing, detectable eruption problem in the maxillary left segment, which received no intervention. (b) Result of asymmetric eruption in the maxillary left segment.

Fig 10-2 (a) Original, normal eruption pattern. (b) Developing asymmetric eruption. (c) Resulting problem.
Diagnostic procedures for eruption problems cannot be completed without careful radiographic evaluation. Several kinds of radiographic techniques are available for this purpose (see chapter 3).
Systemic factors also must be considered in clinical examination. Further evaluation and consultation with other medical professionals might be required. Delayed eruptions caused by systemic factors are usually associated with a generalized delayed timing in all tooth emergence and show no change in the sequence of eruption. In contrast, when delayed eruption has a local cause, the number of affected teeth are few (in a short segment), and the order of tooth eruption is also altered, such as an asymmetric type of eruption on the left and right sides of the arch.
Radiographic evaluation
Gron30 reported that the basis for distinguishing a delayed eruption is the root length at the time of eruption. Under normal circumstances, tooth emergence begins when three-quarters of the final root length is established. The lengths of roots at the time of eruption are not exactly the same for different teeth, however. For example, the canines and permanent second molars erupt after three-quarters’ root length has been completed, and mandibular incisors and permanent first molars erupt before completion of three-quarters’ root length.
DTE resulting from local factors or abnormalities in tooth or root development, such as ankylosis, space loss, or the presence of any obstacle, such as a supernumerary tooth, odontoma, or cyst, can be diagnosed by careful radiographic evaluation. DTE might be the result of defective tooth formation, and the first step in examination should be to assess whether the defect is localized or generalized. Retarded formation and eruption of mandibular second premolars is a common problem that must be carefully evaluated in all kinds of treatment planning and especially before serial extraction and space management (Fig 10-3).
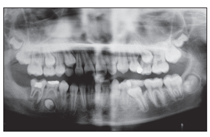
Fig 10-3 Retarded development of the mandibular right premolar. The left premolar shows complete development.
As mentioned earlier, several local and general factors can delay eruption of the permanent dentition, including ankylosis, cyst formation, tooth displacement, supernumerary teeth, and space deficiencies (Figs 10-4 to 10-7).
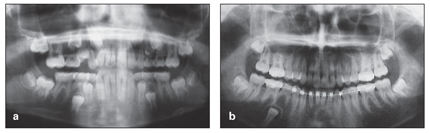
Fig 10-4 Mandibular right premolar, unerupted because of ankylosis. (a) Panoramic radiograph taken in the late mixed dentition. (b) Panoramic radiograph taken 3 years later, showing changes to the right premolar, which should have been extracted earlier.
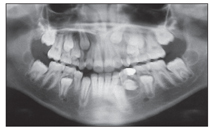
Fig 10-5 Cyst formation, preventing eruption of the mandibular left canine and premolar.
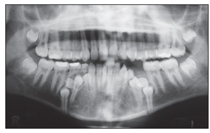
Fig 10-6 Four supernumerary teeth, preventing eruption of all mandibular premolars. The supernumerary teeth should have been extracted long ago.
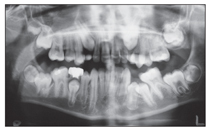
Fig 10-7 Space loss, preventing eruption of both mandibular left premolars.
Therapeutic considerations
DTE presents a challenge for orthodontic treatment if it is not diagnosed and treated at the initial stages of development. The best management of DTE, when the teeth do not erupt at the expected age, is early detection through longitudinal monitoring of panoramic radiographs and timely intervention in the problem.
If the problem has already developed, a careful evaluation should be performed first to establish the etiology of the problem and the stage of the problem; then the treatment plan can be designed accordingly. After careful examination, determination of the problem and the etiologic factors, and establishment of the type and stage of DTE, a number of options are available for management of this abnormality:
• If all diagnostic data indicate a poor prognosis and hopeless situation for the affected tooth, the management is extraction of the affected tooth or teeth and subsequent space closure or prosthodontic or implant replacement. These types of teeth include unerupted and deeply ankylosed permanent teeth and unerupted teeth with severely deformed tooth structure (see Fig 10-4).
• If DTE has affected a primary tooth, it must first be kept under close observation. An unerupted primary tooth with serious defects should be extracted, and, depending on the condition of the succedaneous tooth and stage of eruption, space must be maintained until permanent tooth eruption.
• If the affected tooth is severely malformed, permanent teeth usually must be extracted, but the extraction can be postponed until after close observation of the growth period and appropriate development and preservation of the surrounding alveolar ridge. Occasionally, defective teeth can be saved after eruption with a crown or to serve as abutments for restorative options.
• If an obstacle is preventing normal eruption, the best option is surgical elimination of the obstacle to facilitate eruption. This obstacle can be fibrotic tissue, a bone barrier, an ankylosed primary molar, a remaining root, a cyst, a supernumerary tooth, or an odontoma. If the DTE results from a lack of space and crowding, the best option is space regaining or space creation, space maintenance, and guidance of eruption. Depending on etiologic factors and the type of problem, different options might be needed after surgical removal of the obstacle:
– Some patients may need only a period of observation or space maintenance for the unerupted tooth and then observation.
– Some patients may need space regaining after removal of the obstructing factor if the space has been lost and then observation.
– Some patients, even after surgical removal of the obstacle, may also need orthodontic traction of the delayed or unerupted tooth, which can be achieved by bonding an attachment to the affected tooth and then initiating tooth traction.
• If clinical and radiographic evaluation of DTE indicates no obvious developmental defect, such as root deformity, ectopic tooth position, or physical obstruction, periodic observation is recommended.
• If observation indicates that the tooth is lagging in its eruption status and the root has reached two-thirds its length, active orthodontic treatment and traction must be implemented.
• If DTE has a systemic or syndromic cause, a team of specialists might be required for proper testing and treatment procedures.
Early Exfoliation of Primary Teeth and Premature Eruption of Permanent Teeth
In the same way that the timing of eruption of primary and permanent dentition may vary, the timing of exfoliation may differ among individual children. There are also certain occasions when early exfoliation of primary teeth and early eruption of permanent successors might need attention and management.
Etiology
Local factors
Untreated and severe caries affecting primary teeth and mouth injuries suffered during sports or accidents are common factors in early tooth loss. The most frequent cause of premature loss of teeth is accidents, especially in children. The teeth that are lost with the greatest frequency are the maxillary central incisors, especially in children with severe overjet due to severe incisor protrusion.
Local factors that can cause early exfoliation of the primary teeth are longstanding periapical abscess and aggressive periodontitis, which cause early shedding of primary teeth and early resorption of the covering bone of permanent successors and early permanent tooth eruption. Figure 10-8 shows panoramic radiographs of two patients who lost their right primary molars due to local infection and abscess, resulting in early eruption of the first premolars, which have short roots, are mobile, and will need to be maintained. In contrast, on the left side the primary molars are present, and the permanent successor is far from eruption.
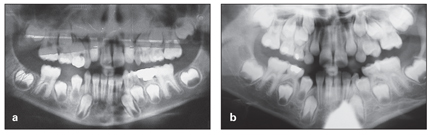
Fig 10-8 (a and b) Early eruption of the mandibular right premolar, which has very short roots and is very mobile.
Pathologic and systemic factors
Although premature loss of the primary teeth in conjunction with early eruption may be of no clinical significance, early exfoliation in children younger than 5 years of age without any history of trauma should not be overlooked by the clinician. These situations need special attention because they can be related to pathologic conditions of local or systemic origin. The following are some examples of systemic conditions that cause early exfoliation.
Hypophosphatasia. Hartsfield32 stated that premature loss of teeth associated with systemic disease results from some change in the immune system or connective tissue. The most common of these conditions appear to be hypophosphatasia and early onset of periodontitis. Hypophosphatasia is a rare inherited metabolic disease that affects bone mineralization due to mutations in the ALPL gene. The ALPL gene plays an important role in signaling the production of an enzyme called alkaline phosphatase, which plays an essential role in mineralization of the skeleton and teeth. The loss of function that results from mutation of the ALPL gene disrupts the process of mineralization; deposition of minerals such as calcium and phosphorus in developing bones and teeth is affected.
Hypophosphatasia can appear anywhere from before birth to adulthood. The most severe forms of this disorder occur before birth and in early infancy. Because of mineral deficiency, bones are weak and soft, causing skeletal abnormalities similar to those found with rickets. Childhood forms are less severe, and early loss of anterior primary teeth associated with deficient cementum is one of the first signs of the condition in children. Tooth loss may be spontaneous or may result from slight trauma to the anterior teeth.
Agranulocytosis. Agranulocytosis, also known as agranulosis or granulopenia, is an acute condition in which there is a severe decrease in the production of granulocytes, most commonly neutrophils, so that a pronounced neutropenia affects the body, leaving it defenseless against bacterial invasion. Agranulocytosis is associated with gingival diseases such as gingival bleeding, hypersalivation, halitosis, osteoporosis, destruction of the periodontal ligament, and consequently early exfoliation of teeth.
Severe oral infection. Early exfoliation and tooth loss can also be seen in patients with severe oral infections caused by other disorders, such as Wiskott-Aldrich syndrome, diabetes mellitus, or herpes zoster.
Wiskott-Aldrich syndrome was described first by Wiskott in 1937 and later by Aldrich in 1954. It is a rare, X-linked recessive immunodeficiency disease characterized by eczema, thrombocytopenia (low platelet count), immune deficiency, and bloody diarrhea (secondary to thrombocytopenia).
Periodontitis. Another cause of early tooth loss is periodontitis. The term periodontitis is used to describe a group of multifactorial diseases that can result in the progressive destruction of the periodontal structures, including the periodontal ligament, cementum, and alveolar bone, and ultimately lead to tooth loss.
Acrodynia. Acrodynia, also known as mercury poisoning or pink disease, is a disease caused by exposure of young children to mercury or its compounds. Clinical manifestations of acrodynia include fever, anorexia, desquamation of the soles and palms (causing them to be pink), sweating, tachycardia, gastrointestinal disturbance, and hypotonia.33 The oral findings include inflammation and ulceration of the mucous membranes, excessive salivation, loss of alveolar bone, and premature exfoliation of teeth.
Radiation therapy. Radiation therapy for malignancies of the orofacial region causes xerostomia resulting from salivary gland destruction; the hyposalivation is responsible for the development of cervical caries. Another complication is osteonecrosis, which in many instances is initiated by severe periodontal involvement. Loss of teeth is the end result of these secondary radiation effects.
Failure of Eruption
Another kind of eruption problem is complete failure of eruption of the tooth. PFE is a rare and poorly understood condition usually characterized as a nonsyndromic failure of eruption of permanent teeth when no mechanical obstruction is present.
PFE affects posterior quadrants and causes a dramatic posterior open bite that requires a complex management strategy. Proffit and Vig34 stated that failure of posterior teeth to erupt fully into occlusal contact is the cause of this kind of open bite. According to Proffit and Vig,34 this problem cannot be attributed to a mechanical interference with the eruptive process (eg, ankylosis or soft tissue interference). PFE affects all teeth distal to the most mesial involved tooth, while mechanical failure of eruption affects only the involved tooth or teeth and is primarily the result of ankylosis or soft tissue interference with eruption. Early distinction between PFE and mechanical failure of eruption is clinically important because it determines whether all posterior teeth, or only an individual affected tooth, will not respond to orthodontic force (Fig 10-9).
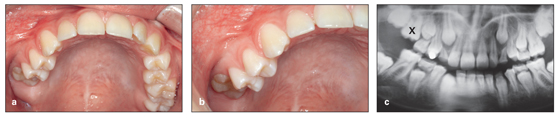
Fig 10-9 (a to c) Primary failure of eruption of the maxillary right first molar.
Periodic radiographic assessment is recommended to monitor the pattern of eruption of the teeth distal to the most mesial affected tooth. PFE usually manifests as a unilateral involvement of the maxillary and mandibular quadrants, but it can be bilateral.
Etiology
Rasmussen and Kotsaki35 explained that unerupted primary teeth are rare and that most cases of failure involve the primary second molars. They classified instances of this anomaly as those in which the impaction is primary, meaning that the teeth have never erupted, or secondary, meaning that after partial eruption the teeth stop erupting and become reimpacted. They concluded that inheritance was the etiology of PFE in the patients they examined and explained that the mode of transmission was autosomal dominant.
Tooth eruption requires the presence of a dental follicle; as Wise20 indicated, the dental follicle regulates the osteoclastogenesis and osteogenesis needed for alveolar bone resorption to create an eruption pathway, alveolar bone formation at the base of the bony crypt, and tooth eruption. Philbrick et al21 concluded that PTHrP seems to regulate osteoclast formation via mediation of the dental follicle, in a manner analogous to the osteoblast-mediated process in the peripheral skeleton.
Recent studies show that PFE is inherited. Mutations in PTH1R genes explain several familial cases of PFE. Therefore, genetic analysis can be combined with clinical diagnostic information to ensure improved orthodontic management of PFE. Frazier-Bowers et al36 investigated the etiology of eruption disorders by using a network pathway analysis in a rat model and found that PTH1R acts in a pathway with genes such as PTHrP that have been shown to be important in bone remodeling and eruption.
In one of the largest and most detailed analyses of teeth affected by PFE, Ahmad et al37 conducted a systematic review of 40 cases in the literature. The review found a family history of eruption failure in almost 50% of the sample. Ahmad et al37 reported that 60% of the affected patients were female, and first and second molars were the teeth most commonly affected. Incisors, canines, and premolars were also involved but with less frequency. There were no significant differences in incidence between the maxilla and mandible or between the left and right sides.
In a more recent study, Proffit and Frazier-Bowers38 reviewed pre-emergent and postemergent eruption, with particular emphasis on distinguishing between isolated molar ankylosis, PFE, and genetic considerations in eruption problems. The study revealed that, in conditions of PFE, all teeth distal to the most mesial affected tooth will fail to erupt and cannot be moved orthodontically. If the problem is isolated ankylosis of the first molar, however, the second and third molars are likely to be normal and will erupt on their own and can be moved orthodontically into the first molar area when the ankylosed tooth is removed.
The study concluded that PFE is an often overlooked cause of posterior open bite and that the diagnostic distinction between isolated ankylosis and PFE is critically important in planning treatment. Proffit and Frazier-Bowers38 also added that genetics is an important consideration in the mechanism and control of tooth eruption and becomes a factor in differential diagnosis of eruption failure.
Stellzig-Eisenhauer et al28 conducted a clinical and molecular genetics study in four families where at least two members were affected by nonsyndromic PFE. The study indicated that nonsyndromic PFE has an autosomal-dominant mode of inheritance. Molecular genetic analysis of the PTHR1 gene revealed three distinct heterozygous mutations, while unaffected persons exhibited no mutations. The researchers concluded that the genetic causes of non-syndromic PFE can be used for the differential diagnosis of eruption failure.
Therapeutic considerations
Primary failure of tooth eruption can cause severe posterior open bite with a poor treatment prognosis that sometimes requires a complex management strategy. Depending on the age of the patient, the number and position of affected teeth, the developmental stage of the roots, and the severity of infraocclusion, various treatment approaches have been proposed, some with successful results, and some with failure.39,40 Simple procedures include extraction of ankylosed primary molars, space control, and monitoring of the permanent teeth for eruption. In more complicated cases, surgical luxation followed by elevation and orthodontic traction of the affected teeth and stabilization of the lux-ated teeth in young patients with incomplete root formation have also been proposed.
When primary molars fail to erupt, orthodontic guidance of eruption is rarely indicated if problems can be detected early and managed properly. Early detection and removal of affected primary molars at the proper time, space maintenance, and monitoring of canine and premolar eruption seem to encompass the first preventive stage for managing this problem; this sequence usually facilitates permanent tooth eruption. In some cases, orthodontic traction may be needed; however, in rare cases, traction and tooth eruption may result in failure and extraction of permanent teeth. Control of space availability and removal of bone barriers and overlying soft tissue can also facilitate premolar eruption.
Mc Cafferty et al39 reported on an 8-year-old boy with severe posterior open bite due to PFE; both right permanent first molars failed to erupt. No significant medical history was present, and the siblings had no similar dental abnormalities. The infraoccluded right primary first and second molars were extracted, and the right permanent first molars were surgically exposed. Eruption of the premolars and molars was monitored over the next 2 years. The premolars showed signs of eruption and continued root development. Exfoliation of the remaining primary teeth proceeded as usual. The right permanent first molars did not erupt and were subsequently extracted. When the patient was 13 years old, orthodontic extrusion was used to further reduce the interdental distance between the canine and premolars.
Lygidakis et al40 reported on a 7.5-year-old boy who presented with localized secondary eruption failure of the mandibular right permanent first molar with infraocclusion. There was no history of eruption failure or ankylosis in any other family member. Treatment was surgical luxation of the tooth, followed by elevation to the occlusal plane and immobilization to the adjacent primary molar. The splint was removed after 4 weeks. Three years’ follow-up revealed successful results and no clinically or radiologically evident pathosis of the area. Root development of the affected tooth was arrested; there was no sign of pulpal necrosis.
Retarded Tooth Development
Retarded eruption of the second premolars is occasionally encountered during the transitional dentition and requires careful attention before treatment planning. This type of eruption disturbance is different from eruption problems commonly observed after space loss and following premature loss of the primary molars and subsequent tilting of the permanent molar that can cause eruption difficulties for second premolars. Retarded eruption of the second premolars is a rare anomaly that is associated with late development of tooth germs. In these cases, eruption of the premolars is excessively late, and it is difficult to predict the time of their emergence (see Fig 10-3). Because of the developmental delays, radiographic evaluation can even lead retarded tooth formation to be misdiagnosed as congenital absence of teeth (Fig 10-10).
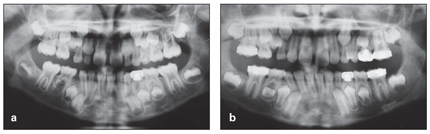
Fig 10-10 (a) Initial panoramic radiograph, considered to reveal congenital absence of the mandibular right premolar. (b) Panoramic radiograph taken 3 years later, revealing a premolar with retarded formation.
According to Massler et al,1 calcification of the second premolar usually begins at the age of 2 to 3 years, and crown formation is usually completed by 6 to 7 years. However, there is always a wide variation in individual timing of premolar calcification and crown formation. In individuals with retarded premolar calcification, the appearance of the tooth germ may not be recognized even at 8 to 12 years.
This eruption disturbance is usually seen unilaterally but can occur bilaterally. In cases of unilateral occurrence, the degree of tooth formation on the contralateral side may help to predict the approximate age of emergence of the affected side.
In an evaluation of five unusual cases of anomalous eruption of the maxillary second premolars that related to late development of the germs, Taguchi et al41 reported that the affected premolars emerged between the ages of 12 years, 3 months and 14 years, 6 months. The study also found that, in some cases, this anomaly is associated with microdontia. Peterka et al42 reported a higher prevalence of retarded tooth development in the affected side of patients with unilateral cleft palate.
In a study assessing the timing of exchange of the maxillary primary and permanent teeth in boys with three types of orofacial clefts (unilateral, bilateral, and isolated cleft), Peterka and colleagues43 concluded that the developmental disturbances of the maxilla and maxillary teeth in patients with orofacial clefts are also associated with alteration of timing of dental exchange.
If a defect or retardation of tooth formation is present, the first step should be to assess whether the defect is localized or generalized. Local delayed eruption can be due to retardation of tooth development. Mandibular and maxillary second premolars are the most common teeth to show retardation in development that is of unknown etiology and disharmonious with the development of adjacent teeth. Therefore, the eruptive development of these teeth must be watched more carefully during the transitional dentition. Treatment planning in the absence of a clear-cut understanding of the condition of these teeth can complicate proper treatment.
Abnormal Sequence of Eruption
A normal sequence of eruption is an important aspect of occlusal development. Variations in the sequence of tooth eruption can have direct effects on the development of the dentition and can be more problematic than tooth eruptions that are a few months early or late. Individual variations in sequence of eruption can play an important role in orthodontic treatment planning and can have a direct clinical application in occlusal guidance and early orthodontic treatment.
According to Moorrees et al, “exactly how the leeway space is utilized depends on the sequence of shedding and eruption of the maxillary and mandibular posterior teeth and the molar occlusion.”44 The normal sequence of exfoliation of the primary dentition plays an important role in the normal sequence of eruption of permanent canines and premolars and in preservation of leeway space for the permanent dentition. Any disruption during the transitional stage, such as premature loss or overretention of primary teeth, may interfere with normal tooth transition and development of occlusion. (The mechanism of the transitional dentition is discussed in more detail in chapters 2 and 5.)
The sequence of eruption of the primary and permanent dentition has been studied extensively over the past several decades. In 1953, Lo and Moyers45 studied the sequence of eruption in 236 Canadian schoolchildren by intraoral examination and radiographs. The study attempted to determine the most frequent sequence of eruption and the final effects of the different sequences on occlusion (according to Angle’s classification). The researchers found 18 different sequences in the maxilla. The most frequent sequence was 6 1 2 4 5 3 7, in 48.72% of children studied, and the second most frequent sequence was 6 1 2 4 3 5 7, in 16.01% of subjects (1= central incisor, 2 = lateral incisor, 3 = canine, 4 = first premolar, 5 = second premolar, 6 = first molar, and 7 = second molar). In the mandibular arch, 17 eruption sequences were observed. The most common sequence was 6 1 2 3 4 5 7, occurring in 45.77% of children, and the second most common sequence was 6 1 2 3 4 7 5, seen in 18.64% of children.45
In a cross-sectional examination of 6,000 children, Garn and Smith46 studied the timing of tooth emergence and reported that the most common sequence in the maxilla was 6 1 2 4 3 5 7 and the most common sequence in the mandible was 6 1 2 3 4 5 7.
Different alterations in the sequence of eruption of the permanent teeth can have different clinical signs and different harmful effects on the occlusion, which are discussed in the following sections.
Eruption of the second molars before the premolars
If the second molars erupt prior to the premolars, the mesial force of second molar eruption can push the permanent first molar and decrease the space available for the second premolar. This may block the second premolar from the arch.
Eruption of the maxillary canines before the premolars
If the maxillary canine erupts before the maxillary first premolar, it can cause crowding or impaction of the second premolar. If the maxillary canine erupts at the same time as the first premolar, the canine will be forced labially. This condition can develop into a more complicated condition if the maxillary molar also shifts forward and the problem of space loss is added to the abnormal sequence of eruption.
Eruption of the mandibular first premolars before the canines
In normal occlusion, the mandibular and maxillary incisors are positioned in such a way that the mandibular dentition is confined within the parameters of the maxillary arch. After premature loss of the mandibular primary canines or primary first molar, the mandibular incisors tip lingually, and arch length is decreased anteroposteriorly. A normal eruption sequence and positioning of the mandibular permanent canines with a strong root and slightly distal position provide a strong support for normal mandibular incisor positioning. Any disturbances in the sequence between mandibular canine and first premolar can cause lingual tipping of the mandibular incisors and lingual or buccal displacement of the mandibular canines.
When the sequence of eruption in the mandibular arch is normal (3 4 5) and slight crowding is observed in the mandibular incisor area, the canine erupts into the space created by the exfoliation of the primary canine and moves slightly distally, creating a small amount of space for those crowded incisors.
Sampson and Richards47 stated that, depending on the timing and sequence of eruption of the canine, various contact points are formed between the lateral incisor and the canine. They reported that incisor crowding seems to be greatest when the canine erupts buccally.
When incisor crowding is severe and tooth size–arch size discrepancy is present, the canine may be impeded in its eruption by the primary first molar, or exfoliation of the primary first molar may be accelerated, and the first premolar consequently may erupt before the canine. In this situation, the first and second premolars will occupy leeway space, causing canine impaction. If mandibular canines and first premolars erupt, occupying some leeway space, impaction or lingual eruption of the second premolars is possible.
Eruption of the maxillary canines before the first premolars
The sequence of eruption of the maxillary canine and premolar usually proceeds from the posterior to the anterior region of the arch. If the canine erupts before the premolar and space is deficient, the canine can push the maxillary incisors forward to create space or push the first premolar out of the arch. If the maxillary primary second molar is exfoliating, it can cause second premolar impaction.
Eruption of the maxillary second molars before the mandibular second molars
This abnormal sequence can push the maxillary first molar mesially and cause a Class II molar relationship. This condition occurs more easily if the maxillary and mandibular permanent first molars are in an end-to-end relationship.
Eruption of the maxillary lateral incisors before the central incisors
There are some occasions when the lateral incisors may erupt before the central incisors, such as in the presence of overretained primary central incisors, when there is very premature loss of primary central incisors, after development of sclerotic tissue, in the presence of a dense bone barrier, or in the presence of a mesiodens. Any of these conditions and the consequent potential for eruption of lateral incisors before central incisors requires early detection and intervention. It is important to eliminate the cause and maintain the space for the central incisors, or crowding, uneruption, and impaction of the central incisors are inevitable.
Asymmetric eruption in the left and right sides of the arch
In all types of eruption sequences, usually there is a symmetric pattern between the left and right sides of the arch with some time variation among different individuals. Most investigators accept a maximum of 6 months’ difference between left and right sides of the arch as normal. Asymmetric eruption between the left and right sides of the arch that persists for more than 6 months indicates the presence of some problem and requires a careful radiographic evaluation (Fig 10-11).
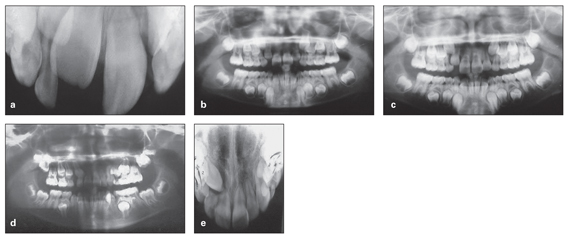
Fig 10-11 Asymmetric eruption that, due to negligence, was not evaluated at the proper time and caused various occlusal problems. (a) Occlusal radiograph taken in 1999, showing asymmetric eruption of the central incisors. (b) Panoramic radiograph taken in 2000, showing asymmetric eruption continuing with the lateral incisors. (c) Panoramic radiograph taken in 2003, showing the continued asymmetric eruption of the lateral incisors and the proximity of the maxillary right canine to the lateral incisor root. (d) Panoramic radiograph taken in 2004, showing complete resorption of the lateral incisor root. (e) Occlusal radiograph taken in 2004.
Application of longitudinal panoramic radiograph monitoring during the transitional dentition can be very helpful in the early detection of asymmetric eruption or abnormal sequence of eruption, and careful intervention can prevent damage to the occlusion. Utilization of permanent molar anchorage, such as a lower holding arch, Nance appliance, or transpalatal arch, and guidance of eruption by selective grinding or primary tooth extraction can change the pattern of tooth eruption and intercept many future occlusal problems (see chapters 3 and 5).
The case shown in Fig 10-11 is an example of asymmetric eruption that, due to negligence, was not evaluated at the proper time and caused various occlusal problems. Two early radiographs show evidence of asymmetric eruption of the central and lateral incisors (see Figs 10-11a and 10-11b). The next panoramic radiograph, taken 3 years after the first one, shows continuation of the asymmetric eruption of the lateral incisors and the close proximity of the maxillary right canine crown to the lateral incisor root (see Fig 10-11c). No early intervention was initiated at this time, and the parents were asked to bring the child back for a checkup within 6 months. Unfortunately, they returned 2 years later. The final radiographs, taken 2 years later when the child was brought to clinic with a mobile maxillary right lateral incisor, show the complete resorption of the root (see Figs 10-11d and 10-11e).
Ectopic Eruption
Ectopic eruption, or ectopia, is defined as eruption that is out of the normal position. Ectopic eruption is a developmental disturbance in the eruption pattern of the teeth causing alteration of the tooth’s eruption pathway and creating problems for adjacent teeth.
Prevalence
According to Weinberger,48 the incidence of ectopic eruption ranges from 2% to 4.3% of the population. It occurs more often in the maxilla and more often unilaterally. The teeth that are most frequently found to be ectopic are maxillary first molars, maxillary canines, mandibular second premolars, and mandibular canines.
Ectopic eruption of permanent first molars
Ectopic eruption of the permanent first molar is a common problem during the early mixed dentition. In this situation, the permanent first molar erupts at a mesial angulation toward the primary second molar, resulting in a cessation of eruption that causes atypical resorption of the adjacent primary molar (Fig 10-12a). The ectopic permanent tooth may get locked in this position or can correct itself without treatment and erupt into a normal position later. These two types of ectopia are classified as reversible (jump) and irreversible (hold) ectopic eruption.
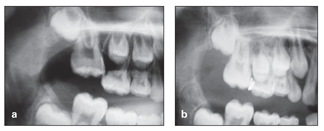
Fig 10-12 (a) Ectopic eruption of the maxillary right first molar, causing resorption of the primary second molar. (b) Wedging technique for distalization of the molar. Brass ligature wire has been placed between the first molar and adjacent teeth.
Etiology of ectopic molar eruption
Reports indicate some familial tendency for ectopic molars.49 Several local factors can contribute to this anomaly:
• Large primary or permanent molars
• Convexity of the distal surface of the maxillary primary second molar
• Convexity of the mesial surface of the maxillary permanent first molar
• Missing maxillary second premolar
• Growth deficiency of the maxillary tuberosity and posterior positioning of the maxilla
• Mesially directed path of eruption of the permanent first molar
• Delayed development of the permanent first molar
Sequelae
Early detection and proper intervention can prevent many destructive sequelae. Delayed correction of this anomaly can have consequences such as pulpal infection of the primary second molar, abscess formation, premature loss of the primary second molar, space loss and tipping of the permanent first molar, and impaction of the second premolar.
Treatment options for ectopic molars
Traditionally, three different strategies have been applied in the management of ectopic permanent molars: observation, extraction of the primary molar, and distalization of the permanent first molar. An alternative treatment for mandibular molar ectopia involves disking of the distal surface of the primary second molars, which allows the permanent molars to erupt.
Observation. One option is to observe the area for 5 to 6 months; not all ectopic molar eruptions require treatment. For example, treatment is not necessary if the permanent first molar has moved less than 2 mm toward the primary second molar and the long axis of the permanent molar shows minimal tipping.
Extraction of the primary molar. The second option is extraction of the primary molar—if pain or mobility is present— or waiting for exfoliation of the primary second molar, followed by an orthodontic approach, which involves distalization of the permanent molar and space regaining.
Distalization of the permanent first molar.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


