Introduction
White spot lesions that form during orthodontic treatment are a problem for patients and clinicians. Lesion infiltration with low-viscosity light-cured resin has been proposed as a treatment to inhibit further demineralization. The purpose of this study was to assess the durability of assimilation of white spot lesions and sound adjacent enamel achieved over 6 months with resin infiltration.
Methods
Twenty-one consecutive subjects with 231 noncavitated, unrestored white spot lesions after multibracket treatment were recruited at the Department of Orthodontics, University of Göttingen (Germany), for lesion infiltration. A simple randomized, split-mouth, controlled design was used to allocate subjects to the treatment and control groups. In the treatment group, white spot lesion infiltration of the anterior teeth was performed with low-viscosity light-cured resin after enamel conditioning with a 15% HCl gel. Color and lightness of the white spot lesions and the sound adjacent enamel were assessed with a spectrophotometer before infiltration and after 1 day, 1 week, 4 weeks, 3 months, and 6 months, using the system of the Commission Internationale de l’Eclairage. Multifactorial analysis of variance with repeated measures and pair-wise comparisons were used to analyze the effects of infiltration and time elapsed on the color differences at an α level of 5% and a power of 80%.
Results
Analysis of 20 subjects and 39 quadrants in each group (108 teeth in the control group; 111 teeth in the treatment group) showed that both parameters of treatment and time duration had globally a highly significant influence on the color difference values. Assimilation of white spot lesion color to the surrounding enamel after infiltration was stable with no significant changes over 6 months; the mean color difference of white spot lesions vs sound adjacent enamel (ΔE baseline vs 6 months) was 2.55 (95% confidence interval [CI], 1.431-3.678). The untreated control teeth showed no significant changes over 6 months compared with the baseline: mean (ΔE), 0.29 (95% CI, −0.335-0.928). No important adverse events or side effects were observed.
Conclusions
Resin infiltration improves the esthetic appearance of demineralized teeth. The results showed sufficient durability over 6 months.
Orthodontic corrections are mostly achieved with fixed orthodontic appliances. One negative side effect is the formation of white spot lesions and incipient caries. This is due to the facts that (1) oral hygiene is more difficult in patients with multibracket orthodontics than without fixed treatment, (2) orthodontic patients develop significantly more white spot lesions than nonorthodontically treated persons, and (3) nontreatment of white spot lesions results in progression to carious lesions and esthetic problems. White spot lesion formation has been described as an extremely rapid process of a few weeks’ duration, with a sharp increase in white spot lesion numbers within the first 6 months. Moreover, inattentive surplus orthodontic etching and inadequate oral hygiene have been shown to have significant triggering or deteriorating effects on white spot lesion formation. Optimal oral hygiene is considered a prerequisite for the prevention of white spot lesions. Other preventive strategies include the application of fluoride-releasing sealers or bonding materials, daily rinsing with sodium fluoride mouth rinse, and chlorhexidine applications. However, despite all preventive measures, white spot lesions are still a problem to some orthodontic patients: almost half (46%) of those with fixed appliances develop at least 1 white spot lesion after 12 months of treatment, and other authors have found an incidence of at least 1 new white spot lesion in 72.9% of patients, in whom 2.3% of the lesions were cavitated.
Whereas for cavitated lesions, restoration is essential, noncavitated lesions should receive preventive therapy aimed at arresting and remineralizing the lesion.
As a new way of treating white spot lesions, lesion infiltration with low-viscosity light-curing resins (Icon infiltrant; DMG, Hamburg, Germany) has been recently proposed to inhibit further demineralization. Case reports and short-term in-vitro studies have indicated reduced visibility of infiltrated white spot lesions as an additional positive side effect; this is due to the similar refractive index of the infiltrant and the sound enamel areas.
Although a number of studies have been carried out to investigate the ability of infiltration to inhibit the progression of white spot lesions, randomized controlled long-term in-vivo studies of the camouflage effect are needed to achieve a valid estimate of the durability of potential masking effects.
The aim of this study was to assess the extent and durability of color and lightness changes after 6 months between white spot lesions and sound adjacent enamel areas after resin infiltration compared with an untreated control group under in-vivo conditions. We used the system of the Commission Internationale de l’Eclairage (CIE) involving 3 color parameters: lightness (L), red/green chromaticity (a), and yellow/blue chromaticity (b).
The null hypothesis of no significant color difference (ΔE) values (white spot lesions vs sound adjacent enamel) between the treatment and control groups after 6 months was tested.
Material and methods
This was a single-center, split-mouth, controlled, simple randomized trial, with an allocation ratio of control and treatment quadrants (clusters) of 1:1. The subjects were recruited with the exclusion criteria of cavitated lesions and filled, restored, and deciduous teeth. Control or treatment quadrants consisted of each incisor and canine that met the inclusion criterion of a white spot lesion after debonding; if 1 exclusion criterion applied for 1 tooth, the subject was excluded from the trial.
Sample size calculation (ΔE threshold value, 3.0; SD, 4.5 units; alpha error, 5%; power, 80%) based on completed assessment cycles of the first 13 subjects indicated that 20 subjects (each with a mean of 8.3 trial teeth) were needed. Because subjects who are willing to participate in a long-term trial and are eligible for infiltration therapy are not abundant, we decided to use a split-mouth (cluster) design, which results in matching or decreased variance between the quadrants (clusters), thereby reducing the required sample size. On the other hand, clustering results in correlated data and increases the required sample size.
Of 23 consecutive subjects between 12 and 19 years of age who had received multibracket treatment, 21 (10 male, 11 female; mean age, 15.5 years) with white spot lesions (231 teeth: 114 control and 117 treatment) were included in the trial.
Table I shows detailed information regarding the subjects as well as the lapse of time between debonding and infiltration.
| Subject | Complete etching duration (min) | Time elapsed after debonding (mo) | Trial teeth (n) | Treated teeth (n) | Control teeth (n) | Missed appointments (time points) |
|---|---|---|---|---|---|---|
| 1 | 6 | 8 | 8 | 4 | 4 | — |
| 2 | 6 | 3 | 11 | 5 | 6 | — |
| 3 | 6 | 5 | 12 | 6 | 6 | T1: 4 images not analyzable |
| 4 | 6 | 5 | 11 | 5 | 6 | — |
| 5 | 6 | 11 | 12 | 6 | 6 | T4 |
| 6 | 6 | 9 | 12 | 6 | 6 | — |
| 7 | 6 | 8 | 12 | 6 | 6 | T2 |
| 8 | 6 | 12 | 12 | 6 | 6 | — |
| 9 | 8 | 6 | 12 | 6 | 6 | — |
| 10 | 6 | 9 | 12 | 6 | 6 | — |
| 11 | 8 | 7 | 11 | 6 | 5 | — |
| 12 | 8 | 9 | 12 | 6 | 6 | T2 |
| 13 | 6 | 3 | 12 | 6 | 6 | T4, T5 |
| 14 | 7 | 1 | 8 | 4 | 4 | — |
| 15 | 7 | 1 | 12 | 6 | 6 | — |
| 16 | 7 | 1 | 11 | 6 | 5 | — |
| 17 | 8 | 4 | 12 | 6 | 6 | — |
| 18 | 8 | 1 | 12 | 6 | 6 | — |
| 19 | 8 | 2 | 7 | 5 | 2 | — |
| 20 | 8 | 1 | 8 | 4 | 4 | — |
| 21 | 6 | 1 | Excluded | Excluded | Excluded | T2, T3, T4, T5 |
| Total: 219 | Total: 111 | Total: 108 |
The white spot lesions were treated on the front teeth of either quadrants 1 and 3, or 2 and 4, with the other two acting as controls. Simple randomized cluster (quadrant) allocation was performed by lot before the start of the trial by the second author, and the allocations were concealed in opaque envelopes (lots) by a person not connected with this study. The patients received the same type of toothbrushes (Oral-B Classic Care; Procter & Gamble, Schwalbach am Taunus, Germany) and dentifrice (elmex; GABA, Lörrach, Germany) for use during the trial.
This study received approval by the ethics committee of the University of Göttingen in Germany, and all patients and their guardians gave informed consent before the start of the trial.
The extent of assimilation and durability of effect was assessed by comparing CIE L*a*b data collected before infiltration (baseline), directly after infiltration (1 day), and 1 week, 4 weeks, 3 months, and 6 months later. The primary outcome measure was the difference between the summarized color and lightness values (ΔE of white spot lesions vs sound adjacent enamel) between the treatment and the control quadrants, and their development over 6 months.
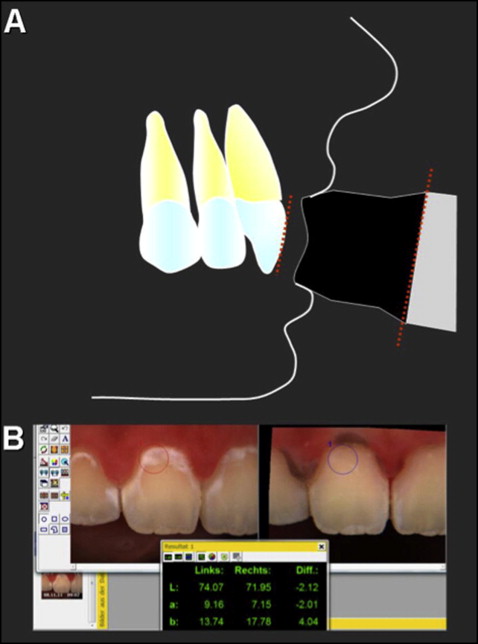
The color assessments were standardized to the highest possible degree using a spectrophotometer (ShadePilot; Degudent, Hanau-Wolfgang, Germany) with closed lips to exclude sources of error typical for in-vivo setups, such as ambient light or varying head position on dental color values ( Fig 1 , A ). The assessment field was captured using a system-immanent target caption. Locations of assessment field outlines were stored by the system and used for retrieval of the masked white spot lesions and sound adjacent enamel in follow-up assessments ( Fig 1 , B ). All assessments and infiltration treatments were performed in the Department of Orthodontics at the University of Göttingen by 1 operator (A.E.); therefore, there was no blinding of the assessor to the intervention or the control quadrants. Also, blinding of the patients to the treatment or the control teeth was not feasible and not considered necessary, because an objective color assessment was performed, not the patient’s subjective perception of color changes.
White spot lesion infiltration (Icon; DMG) in the treatment quadrants was carried out according to the manufacturer’s instructions, including preparation of the white spot lesions and sound adjacent enamel surface by 15% hydrochloric acid gel (Icon-Etch) and subsequent drying with the ethanol desiccation solution (Icon-Dry) supplied by DMG. In compliance with the instructions, the etching was repeated for deep lesions. The need for additional etching was determined visually after the dry solution was used; this provided a preview of the esthetic result to be expected after infiltration, thereby adjusting frequency of etching to the surface hardness and the depth of the white spot lesions. A note was made of the total etching time needed for each subject ( Table I ).
Statistical analysis
Color and lightness characteristics (L*a*b*) of the respective white spot lesions and sound adjacent enamel assessment areas were each summarized for intergroup and intragroup area comparisons in each group at distinctive time points as ΔE values:
Δ E ( PAR 1 − PAR 2 ) = [ ( L PAR 1 − L PAR 2 ) 2 + ( a PAR 1 − a PAR 2 ) 2 + ( b PAR 1 − b PAR 2 ) 2 ] 1 / 2
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


