http://evolve.elsevier.com/Haveles/pharmacology
The term cardiovascular disease refers to a variety of diseases of the heart and blood vessels. Examples of these diseases are hypertension, angina pectoris, coronary artery disease, arrhythmias, and heart failure (HF). Although cardiovascular disease is the leading cause of death in the United States, patients with cardiovascular disease are now living longer, more productive lives because of cardiac care units, comprehensive drug therapy, and intensive screening procedures. These developments explain why cardiovascular disease affects such a large proportion of the dental patient population.
The dental hygienist first identifies the patient with cardiovascular disease while taking the medical or drug history. It is common for such a patient to have several cardiovascular conditions, such as HF, hypertension, and hypercholesterolemia. For each disease, a patient may take one or more medications.
Because cardiovascular medications are often given for the patient’s lifetime, knowledge of the actions, problems, and effects of these drugs on dental treatment is essential. Both the disease and the drugs used in its treatment can affect the management of a patient’s dental care.
Before each group of drugs is discussed in this chapter, the disease for which the drugs are used is briefly described, beginning with general considerations concerning the dental treatment of patients with cardiovascular disease.
Dental implications of cardiovascular disease
Contraindications to Treatment
Although most patients with cardiovascular disease can be safely treated in the dental office, circumstances may arise in which dental treatment should be delayed until the patient’s disease is under better control. Patients who have suffered a myocardial infarction should wait 6-months before receiving any type of oral health care in order to give the heart a chance to heal. Bacteria from the mouth can enter the bloodstream and weaken an already weakened heart. If oral health care is necessary before 6-month have elapsed one should consult with the patient’s cardiologist or general practitioner to determine whether or not the patient’s heart has healed sufficiently.
Certain medical situations, listed in Box 14-1, are absolute contraindications to dental treatment until a consultation with the patient’s provider has identified any special treatment alterations that might be warranted. These absolute contraindications apply only to uncontrolled or severe cardiovascular diseases. Examples of absolute contraindications to elective dental treatment include very high blood pressure and uncontrolled arrhythmias. Most patients with cardiovascular disease can be treated in the dental office. The type of procedure anticipated, the stress of the procedure, and the fact that many procedures are elective must be considered. Once a thorough health history is obtained, a determination can be made about whether the patient’s provider should be consulted before dental treatment is begun. When the health care provider is contacted, it is important to explain the procedure(s) indicated for the patient.
Vasoconstrictor Limit
When a local anesthetic containing a vasoconstrictor is used in the treatment of a patient with cardiovascular disease, the severity of the patient’s disease must be considered. The majority of cardiovascular patients should benefit from the use of epinephrine in the local anesthetic agent. The amount and effect of the epinephrine administered must be weighed against the fact that poor pain management can produce the release of endogenous epinephrine. Limiting the dose of epinephrine to the cardiac dose may be warranted in a few severely affected patients (see Chapter 9 for a detailed discussion of vasoconstrictor limits).
Using a slow rate of injection and appropriate aspiration techniques to avoid intravascular injection reduces the chance of vasoconstrictor adverse reactions. A “fight-or-flight” reaction related to the patient’s anxiety also results in the release of endogenous epinephrine indistinguishable in effect from that of the exogenous epinephrine. (So, being really scared feels exactly like epinephrine because one is making epinephrine.)
Periodontal Disease and Cardiovascular Disease
Researchers and government agencies continue to investigate the possible relationship between periodontal disease and cardiovascular disease. Studies both support and reject such a relationship. Researchers do agree that more studies are needed. Regardless of study outcomes, it is very important that patients maintain optimal oral health care by receiving oral health care twice a year, brushing teeth a minimum of twice a day, regularly flossing teeth, and making sure that dentures fit properly.
Heart failure
The incidence of HF in the United States has remained relatively stable, at almost 650,000 cases diagnosed annually. Approximately 5.1 million Americans have clinical symptoms of HF, and its prevalence is expected to rise. The incidence of HF rises with age. The incidence in those 65-69 years is 20 per 1000, and in those older than 85 years, it is more than 80 per 1000 individuals.
The heart functions as a pump, ensuring adequate circulation of the blood to meet the oxygen needs of all the body’s tissues. When oxygen needs are increased, as in exercise, the normal heart adjusts its output to meet them higher. If the heart is unable to keep up with the body’s needs, it becomes a “failing” heart, and the pumping mechanism becomes inefficient. This occurs because the heart muscle has suffered an injury and cannot keep up its work. Some enlargement of the heart produces a more efficient heartbeat and cardiac output (Starling’s law). However, over time, additional cardiac enlargement occurs (cardiac muscle stretched past its maximum effectiveness by the presence of excess blood that it cannot pump out), and the patient becomes tachycardic. This inefficient pumping mechanism results in an inadequate cardiac output and unsatisfactory circulation. Various forms of injury to the heart, such as myocardial infarction (MI) (heart attack), arrhythmias, and valvular abnormalities from rheumatic heart disease, can contribute to a failing heart.
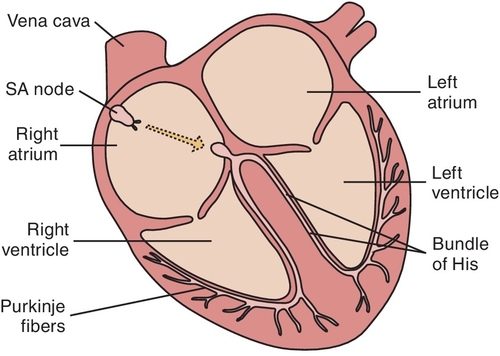
The heart has two sides: the right and the left (Figure 14-1). In HF, the heart does not provide adequate cardiac output to provide for the oxygen needs of the body. Over time, the blood accumulates in the failing ventricle(s). The ventricle(s) enlarge(s) and finally become(s) ineffective as a pump.
One or both sides of the heart can fail. Usually, the left side fails first. If the left side of the heart fails, the blood backs up into the pulmonary circulation (lungs). Pulmonary edema results, producing dyspnea and orthopnea. Dental patients with left heart failure may need to be in a semireclined position to undergo dental treatment. If the right side of the heart fails, then the right ventricle is unable to remove all the blood from that side of the heart. Right-sided heart failure causes systemic congestion. Symptoms include peripheral edema with fluid accumulation evidenced by pitting edema (pedal edema). Over time, many patients experience failure of both sides of the heart, with symptoms of failure on both sides.
Treatment of Heart Failure
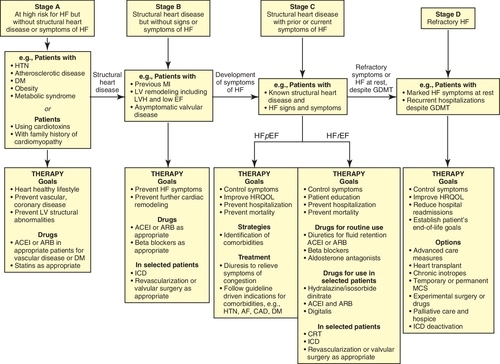
Heart failure therapy is based on the American Heart Association (AHA) stage of heart failure and whether or not the patient has any comorbid conditions (Figure 14-2). Once the patient has been evaluated the physician can treat him or her with the drugs reviewed in this section. Many patients may require a combination of medications. The following discusses the role of the listed classes of medication and their role in treating HF. A detailed discussion of their pharmacologic effects can be found in the section on hypertension.
Diuretics
Most patients with HF have edema, or fluid retention. Diuretics are used in these patients to relieve the symptoms of HF. The American College of Cardiology (ACC) and AHA recommend that all patients who have evidence of fluid retention and most patients with a history of fluid retention be prescribed a diuretic. In clinical trials, patients taking a combination of a diuretic and other drugs used to treat HF had better survival. Loop diuretics, such as furosemide, appear to be more effective than thiazide diuretics, although some patients may show a more favorable response to other diuretics (i.e., bumetanide, torsemide) because of their increased oral bioavailability. Diuretics should be combined with angiotensin-converting enzyme inhibitors (ACEIs), angiotensin receptor antagonists or blockers, beta-blockers, or aldosterone antagonists.
Angiotensin-Converting Enzyme Inhibitors
Current guidelines from the ACC and the AHA now recommend prescribing an angiotensin converting enzyme inhibitor (ACEI) for all patients with symptomatic (stage C) heart failure and for asymptomatic patients with a decreased left ventricular ejection fraction (LVEF) or a history of MI unless there are contraindications to an ACEI. ACEIs improve symptoms in patients with heart failure within a period of 4-12 weeks, decrease the incidence of hospitalization and MI, and prolong survival. ACEIs are now considered first-line therapy and are the cornerstone of HF therapy. Unless there are contraindications, an ACE inhibitor should be used in combination with a β-blocker.
Angiotensin Receptor Blockers
Angiotensin receptor blockers (ARBs) have also been shown to reduce mortality and symptoms. They are recommended for patients who cannot tolerate ACEIs and are also considered first-line therapy for HF. These drugs may be used as alternatives to ACEIs in the patient already taking an ARB for a comorbid condition such as hypertension.
β-Adrenergic Blockers
The ACC/AHA guidelines now recommend β-blockers for patients with symptoms of HF and for asymptomatic patients with decreased LVEF or a history of an MI unless otherwise contraindicated. Although it has been customary to start a β-blocker after an ACEI, the results of several clinical trials suggest that starting with a β-blocker may be equally, if not possibly more, effective. The ACC/AHA guidelines recommend bisoprolol, carvedilol, and sustained-release metoprolol for patients with current or prior symptoms of heart failure with decreased LVEF to reduce morbidity and mortality.
Aldosterone Antagonists
Aldosterone antagonists are recommended for patients with New York Heart Association (NYHA) class II through class IV HF with an LVEF of 35% or less to reduce morbidity and mortality. Unless contraindicated, aldosterone antagonists are also recommended for patients with a LVEF of 40% or less who have recently had an MIand are showing symptoms of HF or who have a history of diabetes mellitus,. In one clinical trial, the addition of spironolactone to standard therapy reduced the risk of mortality and hospitalization. In another clinical trial, the addition of selective aldosterone antagonist eplerenone to standard therapy reduced both all-cause mortality and cardiovascular mortality in patients with acute MI complicated by left ventricular systolic dysfunction and HF.
Vasodilators
Hydralazine, an arterial vasodilator, lowers peripheral resistance through arterial vasodilation. With a reduction in the afterload, the work of the heart is decreased. Isosorbide dinitrate, a venous dilator, reduces the preload, in turn decreasing the work of the heart. With this combination of agents, the heart is pumping against less resistance and less blood is returning to it (some blood remains in the venous circulation). The heart’s workload is reduced, and symptoms of HF subside. The addition of hydralazine and isosorbide dinitrate to standard therapy in black patients with class III to IV HF significantly lowered mortality and the rate of hospitalization and improved quality-of-life scores. Unless otherwise contraindicated, the same combination can be used in patients with current or prior symptomatic HF and LVEF reduction who cannot take an ACEI or ARB because of poor tolerance to the drug, hypotension, or renal insufficiency.
Cardiacglycosides
Digitalis Glycosides
Digoxin was first described by William Withering in 1785. At first, he thought that cardiac glycosides affected the kidneys because they produced diuresis. Later, these substances were referred to as cardiac or digitalis glycosides: cardiac because they affect the heart and glycoside because of their chemical structure. Digoxin (di-JOX-in) (Lanoxin) is the most commonly used cardiac glycoside. Once the first-line agent for the treatment of heart failure, digoxin is now used only in selected patients with stage C HF and reduced LVEF.
Pharmacologic Effects
The major effect of digoxin on the failing heart is to increase the force and strength of contraction of the myocardium (positive inotropic effect). It allows the heart to do more work without increasing its oxygen use. When the contractile force of the heart is improved, the heart becomes a more efficient pump and the cardiac output increases. After the patient takes digoxin, the heart is reduced to a more efficient size and can function more effectively.
Digoxin also reduces the edema that occurs with HF. As a result of the improved pumping action, more blood circulates through the kidneys (increase in glomerular filtration rate), which mobilizes the edema from the tissues, producing diuresis. The diuresis is not a result of an effect on the kidneys; it is a result of digoxin’s indirect effect in improving the heart’s function. The size of the heart is reduced as the excess blood volume that has collected there is removed via the kidneys.
Digoxin can affect automaticity, conduction velocity, and refractory periods of different parts of the heart in different ways. It slows atrioventricular (AV) conduction, prolongs the refractory period of the AV node, and decreases the rate of the sinoatrial (SA) node. When the refractory period of the AV node is prolonged, fewer impulses are transmitted to the ventricle and the heart rate falls. These effects are useful in the treatment of certain arrhythmias.
Uses
The most common use of digoxin is in the treatment of HF. It is also used for atrial arrhythmias, including atrial fibrillation (AF) and paroxysmal atrial tachycardia (PAT). Patients with HF and normal sinus rhythm may not experience long-term benefit in terms of a lower mortality with the use of digoxin.
Adverse Reactions
Because of digoxin’s narrow therapeutic index (see Chapter 3), toxic effects are not uncommon. Even slight changes in dose, absorption, or metabolism can trigger toxic symptoms. Toxicity is more likely to occur in the elderly.
Gastrointestinal effects
Early gastrointestinal signs of digoxin toxicity include anorexia, nausea and vomiting, and copious salivation. A reduction in the dosage of digoxin usually alleviates these adverse reactions.
Arrhythmias
If a sufficient overdose is given, severe cardiac irregularities can develop. These arrhythmias can progress to ventricular fibrillation and death. Diuretics, often used in the treatment of HF, can produce hypokalemia, which can predispose a patient to serious arrhythmias. One should note that digitalis is used to treat arrhythmias and that its toxicity can cause arrhythmias.
Neurologic effects
The neurologic signs of toxicity include headache, drowsiness, and visual disturbances (green and yellow vision, halo around lights). A pain in the lower face resembling that of trigeminal neuralgia has been reported as a neurologic symptom of digitalis toxicity. Weakness, faintness, and mental confusion have also been reported.
Oral effects
Increased salivation is associated with digoxin toxicity. An increase in the gagging reflex, which may interfere with taking a dental impression, has also been reported with this agent.
Dental Drug Interactions
With either increased or decreased blood digoxin levels, serious problems can occur when the digoxin interacts with other drugs. One drug interaction, between digoxin and a sympathomimetic, both of which can cause ectopic pacemaker activity, may increase the chance of arrhythmias if they are administered concomitantly.
For this reason, the vasoconstrictors added to local anesthetics, which are sympathomimetics, should be used with caution. In patients with severe cardiac disease, the epinephrine dose should be limited to the cardiac dose (see Chapter 9). Erythromycin and tetracycline can increase the toxicity of digoxin in some patients.
Management of the Dental Patient Taking Digoxin
Box 14-2 summarizes the management of the dental patient taking digoxin.
Gastrointestinal effects
If a patient complains of nausea or vomiting, special care must be taken to prevent emesis. These symptoms may be associated with digitalis toxicity, and the patient’s physician should be consulted if the nausea and vomiting have been protracted.
Epinephrine administration
Because digoxin toxicity can sensitize the myocardium to arrhythmias, epinephrine should be used cautiously or limited to the cardiac dose in patients taking digitalis. Patients taking digitalis should be questioned about toxic symptoms before epinephrine is administered. Hypokalemia from diuretics can exacerbate this arrhythmogenic potential.
Pulse monitoring
Because digitalis can cause bradycardia or arrhythmias, the patient’s pulse should be checked before each dental appointment for a normal rate and a regular rhythm. An abnormally slow rate or an irregular rhythm should be reported to the patient’s provider for evaluation.
Antiarrhythmic agents
The terms arrhythmia (ar, insensibility; rhythmos, rhythm) and dysrhythmia (dys, bad; rhythmos, rhythm) are used interchangeably to mean “abnormal rhythm.” Arrhythmias may result from abnormal impulse generation or abnormal impulse conduction. Cardiac diseases, such as myocardial anoxia, arteriosclerosis, and heart block, can cause arrhythmias. The antiarrhythmic agents are drugs that are used to prevent arrhythmias.
Automaticity
The cells of the cardiac muscles, unlike those of skeletal muscles, have an intrinsic rhythm called automaticity. “Pacemaker” cells spontaneously produce action potentials as they undergo slow spontaneous depolarization during diastole (as they rest, they leak ions). If any heart muscle cell is left undisturbed and isolated from the rest of the heart with appropriate nutrients and oxygen, it will beat spontaneously at its own rate. Each type of cardiac cell differs in its automaticity, depending on the function of the particular cell. The cells that specialize in conduction functions have a faster rate of automaticity than other cardiac cells. This design ensures that the heart will beat in a coordinated manner.
The SA node has the fastest rate of depolarization and therefore directs all the other cells in the heart. It normally fires impulses approximately 80 times/min. The SA node is innervated by both the parasympathetic nervous system (PNS) and the sympathetic nervous system (SNS). The SA node sends a message (action potential) to the AV node via the atrial muscle. When the impulse arrives at the AV node there is a slight delay because the muscles beyond the AV node are thinner. The AV node sends the message via the bundle of His to the Purkinje fibers. The Purkinje fibers then send the message to the cardiac muscle cells, to the apex of the ventricles, directing them all to contract as they get the message. This system is repeated with each heartbeat.
In the normal patient, this system functions seamlessly. In the patient with cardiac arrhythmias, diseased parts of the heart can produce abnormal conduction pathways, which may result in arrhythmias.
Arrhythmias
The many types of arrhythmias produce various abnormalities of the heartbeat. These arrhythmias are usually divided into supraventricular (atrial) and ventricular types, depending on the location of the genesis of the arrhythmia. Abnormal arrhythmias may result in tachycardia or bradycardia of the supraventricular (atrial) or ventricular parts of the heart or from ectopic foci. The ectopic foci are “emergent leaders” that preempt the SA or AV nodal rate. The electrical impulses begin at the SA node and travel to the AV node. At the conduction level, different patterns of conduction include the normal pattern, bifurcation (conduction splits and goes two ways), reentry, unidirectional block (action potential is blocked from being stimulated from one side of the tissue but not from the other), and prolonged refractory period.
Several recent deaths of fit adolescents during athletic events have been linked to congenital presence of a prolonged QT interval (torsades de pointes, previously undiagnosed).
Antiarrhythmic Agents
Antiarrhythmic agents are divided into four groups (Table 14-1). The specific actions of these agents are complicated. They work by depressing parts of the heart that are beating abnormally.
Table 14-1
Classification and Mechanism of Action of the Antiarrhythmics
AP, action potential; AV, atrioventricular; CCBs, calcium channel blockers; ERP, effective refractory period; K+, potassium; Na+, sodium; SA, sinoatrial.
Antiarrhythmics may change the slope of depolarization, raise the threshold for depolarization, and alter the conduction velocity in different parts of the heart. For example, decreasing the slope of depolarization reduces the frequency of discharge, and the rate slows. If the threshold for producing an action potential is raised, extra beats may be suppressed. Examples of specific actions of these drugs are decrease in the velocity of depolarization, decrease in impulse propagation, and inhibition of aberrant impulse propagation. Tables 14-1 and 14-2 describe the classification and mechanisms of action of the antiarrhythmics, the dental-related adverse reactions, and the dental implications of the antiarrhythmics.
Table 14-2
Management of Dental Patients Taking Antiarrhythmics
| Specific Antiarrhythmic(s) | Implications and Management |
| All | Check for abnormal or extra heart beats when taking patient’s blood pressure and pulse. Record the type of arrhythmia and the drug therapy. |
| Atrial fibrillation | Patient taking warfarin—check international normalized ratio. |
| Amiodarone | Liver toxicity, blue skin discoloration, photosensitivity—to dental light |
| Calcium channel blockers | Gingival enlargement (verapamil most reported) |
| Disopyramide | Anticholinergic xerostomia |
| Procainamide | Reversible lupus erythematosus–like syndrome, 25-30%; central nervous system depression; xerostomia |
| Quinidine | Nausea, vomiting, diarrhea; cinchonism with large doses; atropine-like effect; xerostomia |
| Phenytoin | Gingival enlargement |
| β-Blockers, nonspecific | Drug interaction with epinephrine; limit to cardiac dose if patient’s condition warrants |
CCBs, calcium channel blockers; CNS, central nervous system; INR, international normalized ratio.
Digoxin
Although digoxin is not included in the antiarrhythmic groups, it is used to treat some arrhythmias. It shortens the refractory period of atrial and ventricular tissues while prolonging the refractory period and diminishing conduction velocity in the Purkinje fibers. Toxic doses of digoxin can result in ventricular arrhythmias.
Antianginal drugs
Angina Pectoris
Angina pectoris is a common cardiovascular disease characterized by pain or discomfort in the chest radiating to the left arm and shoulder. Pain can also be reported radiating to the neck, back, and lower jaw. The lower jaw pain can be of such intensity that it may be confused with a toothache. Angina occurs when the coronary arteries do not supply a sufficient amount of oxygen to the myocardium for its current work. Anginal pain can be precipitated by the stress (increased workload on the heart) induced by physical exercise or by emotional states such as the anxiety and apprehension generated by a dental appointment.
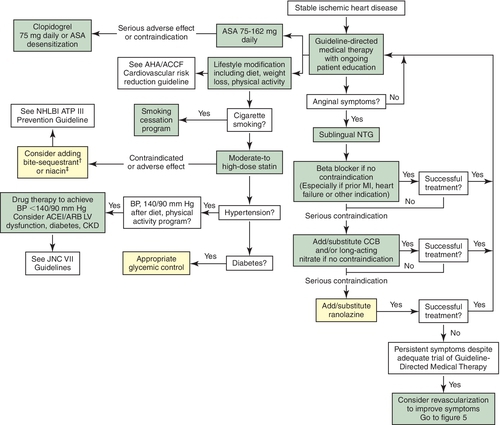
According to the most current ACC/AHA guidelines regarding the treatment of chronic stable angina, the primary goals of therapy are to prevent MI and death and to completely or nearly completely eliminate ischemic symptoms. Goals also include treating both risk factors and comorbid disease states that can precipitate or worsen angina and increase the risk for cardiovascular problems. Figure 14-3 reviews the most current recommendations.
The basic pharmacologic effect of drugs used to manage angina is reduction of the workload of the heart through a decrease in the cardiac output, the peripheral vascular resistance, or both. The oxygen requirement of the myocardium is in turn reduced, relieving the painful symptoms of angina. It is important, however, to keep in mind that these drugs are not curative, and the dental team should be alert to the fact that an anginal episode could occur at any time. Appropriate emergency procedures to manage an acute anginal attack should be reviewed before a patient with angina is treated in the dental office (see Chapter 24). Table 14-3 lists the major antianginal drugs and some of their more pertinent characteristics.
Nitroglycerin-Like Compounds
Nitroglycerin (nye-troe-GLI-ser-in) (NTG) is by far the nitrate most often used for the management of acute anginal episodes (see Table 14-3). In addition to the long-acting nitrates, NTG is also used to prevent anginal attacks induced by stress or exercise. Box 14-3 provides guidelines for managing the patient taking NTG-like compounds.
Mechanism
NTG is a vasodilator that produces relaxation of vascular smooth muscle throughout the body. Indirectly, the work of the heart is reduced by the effect on both the venous and the arterial sides of the circulation. The venous dilation decreases the amount of blood returning to the heart (preload) and thereby lowers the heart’s workload. The arterial dilation reduces the resistance against which the heart must pump (afterload). By lowering the workload on the heart, NTG decreases the oxygen demand, with relief or reduction of angina pain. Tolerance to these effects occurs, unless a nitrate-free period is observed daily.
Sublingual (SL) NTG is used to treat acute anginal attacks. It has a rapid onset (a few minutes) by this route, and its effect can last up to 30 minutes. It is available as an SL tablet (Nitrostat) or a spray used sublingually (Nitrolingual). SL isosorbide dinitrate is also effective for an acute anginal attack. The dental office emergency kit should contain one of these products to manage acute anginal attacks. Dental patients with a history of angina should be asked to bring their NTG to each dental appointment.
Adverse Reactions
Most adverse reactions associated with NTG occur because of its effect on vascular smooth muscle. Severe headaches are often reported (vasodilation) after the use of NTG. Flushing, hypotension, lightheadedness, and syncope (fainting) can also result. Hypotension is enhanced by alcohol and hot weather. SL NTG can cause a localized burning or tingling at the site of administration. The presence of stinging is not indicative of the potency of the NTG.
Significant Drug Interactions and Contraindications
Phosphodiesterase 5 (PDE5) inhibitors are a class of drug used to treat erectile dysfunction. These drugs include sildenafil (Viagra), vardenafil (Levitra), and tadalafil (Cialis). The administration of any of these drugs with either daily or intermittent doses of any nitrate is contraindicated. The combination of a PDE5 inhibitor with any type of nitrate can cause dangerously low blood pressure.
Storage
NTG is degraded by heat and moisture but not by light. NTG should be stored in its original brown glass container and tightly closed because it can be adsorbed by plastic. It should not be refrigerated because condensation of the moisture in the air produces moisture that can reduce the drug’s effectiveness.
If the original bottle is unopened, NTG is active until the expiration date printed on the bottle (assume average storage conditions). When the bottle is opened, the date opened should be written on the outside of the bottle. It should be discarded after 3 months or in accordance with the expiration date printed on the bottle (whichever date is earlier). The NTG spray is effective until its expiration date is reached because air does not enter the container with use.
Various long-acting NTG-like products (see Table 14-3), such as isosorbide dinitrate (eye-soe-SOR-bide dye-NYE-trate) and isosorbide mononitrate, are available for the long-term prophylaxis of anginal attacks. The dose forms available include tablets (swallowed) and topical (ointment and patch) products. With long-term, regular use of such products, tolerance to this effect develops. In fact, no difference can be detected between a long-acting nitrate and placebo when taken without a daily “vacation.” To prevent tolerance, prophylactic nitrates should be given with at least an 8-12-hour “vacation” every day (often during sleep, depending on symptom pattern). The mononitrate dose form requires a 7-hour “vacation” daily; the first dose is given in the morning, and the second dose is given 7 hours later.
β-Adrenergic Blocking Agents
β-Adrenergic blocking drugs (β-blockers) such as propranolol (proe-PRAN-oh-lole) (Inderal), metoprolol (me-TOE-proe-lole) (Lopressor), and atenolol (a-TEN-oh-lole) (Tenormin), are used in the treatment of angina pectoris as initial therapy, if not contraindicated, in patients with or without a prior MI. These drugs block the β-adrenergic receptor response to catecholamine stimulation, thereby reducing both the chronotropic and inotropic effects. The net result is a reduced myocardial oxygen demand. β-Blockers are effective in reducing both exercise- and stress-induced anginal episodes. They are also recommended because they can help prevent MI and death in patients with documented coronary artery disease. Adverse effects include bradycardia, HF, headache, dry mouth, blurred vision, and unpleasant dreams. β-Adrenergic blocking drugs are discussed in the section on hypertension and in Chapter 4 in the section on sympathetic blockers.
Calcium Channel Blocking Agents
Another group of drugs approved for use in angina pectoris is the calcium channel blockers (CCBs) (see discussion in the section on hypertension). Calcium channel blockers can be used as initial therapy when β-blockers are contraindicated or their side effects are intolerable or in combination with β-blockers when the initial treatment with β-blockers is unsuccessful or side effects are not acceptable. A few examples are verapamil (ver-AP-a-mil) (Calan, Isoptin), diltiazem (dil-TYE-a-zem) (Cardizem), and nifedipine (nye-FED-i-peen) (Procardia, Adalat) (Table 14-4).
The mechanism of action of CCBs for the treatment of angina pectoris is related to the inhibition of the movement of calcium during the contraction of cardiac and vascular smooth muscle. Vasodilation and a decrease in peripheral resistance result, thereby reducing the work of the heart. Some CCBs decrease myocardial contractility (negative inotropic effect), resulting in reduced cardiac output. Others increase coronary vasodilation. CCBs reduce ischemia and relieve the symptoms of chronic stable angina. The choice of the specific CCB depends on the patient’s cardiac disease. Short-acting dihydropyridine calcium channel blockers should be avoided.
Ranolazine
Ranolazine is indicated for the treatment of chronic angina alone or in combination with nitrates, β-blockers, CCBs, antiplatelet therapy, lipid-lowering therapy, ACEIs, or ARBs. It can be used alone in patients with contraindications to β-blockers and CCBs. Although it has several pharmacologic activities, its exact mechanism of action is unknown. It does not significantly alter heart rate or blood pressure. It does prolong the QT interval, and caution should be used when it is used in combination with other drugs that increase the QT interval. Ranolazine is generally well tolerated. Adverse effects include dizziness, headache, constipation, and nausea.
Angiotensin-Converting Enzyme Inhibitors
ACEIs are recommended for all people with chronic stable angina who also have hypertension, diabetes mellitus, an LVEF less than 40%, chronic kidney disease, or other vascular disease. Evidence supports the concept that ACEIs have cardioprotective effects that can reduce the incidence of ischemia. ACEIs lower angiotensin II and raise bradykinin levels, possibly leading to reductions in LV and vascular hypertrophy, atherosclerotic progression, plaque rupture, and thrombosis. These hemodynamic changes result in improved myocardial oxygen supply/demand balance.
Angiotensin Receptor Blockers
ARBs are indicated for those patients with chronic stable angina who also have hypertension, diabetes mellitus, an LVEF less than 40%, or chronic kidney disease and who cannot tolerate ACEIs. These agents work much like ACEIs.
Dental Implications
Treatment of an Acute Anginal Attack
Before treating a patient with a history of angina, the dental team should be prepared to treat an acute anginal attack. Before administering NTG for such an attack, however, the dental team should make sure that the patient has not used a PDE5 inhibitor within the past 24 hours. If the patient has used one of these drugs, NTG cannot be given. The best course of action is to immediately contact 911. The patient’s personal NTG tablets or spray should be available and placed on the bracket table in case of an acute attack. Long-acting nitrates and topical products are not useful for the treatment of an acute anginal attack. For acute emergencies, the dental office should have a supply of SL NTG (see previous discussion of storage). The patient should be in the seated position before ingesting the NTG. One tablet can be administered at once, followed in 5 minutes by another, and in another 5 minutes by a third tablet. If these tablets do not stop the anginal attack, the patient should be taken to the emergency room. If using the spray, one should make sure that the patient does not inhale while spraying.
Prevention of Anginal Attack
An acute attack of angina may be prevented through pretreatment with either an anxiolytic agent (e.g., benzodiazepine or nitrous oxide [N2O]) or SL NTG. One should make sure that the patient has not used a PDE5 inhibitor within the past 24 hours. If he or she has, then SL NTG cannot be used as prophylaxis against an angina attack.
Anxiolytics
Because anxiety produces stress and causes the heart to work harder, an antianxiety agent, or anxiolytic (benzodiazepine), may be prescribed to allay anxiety and prevent an acute anginal attack. N2O-oxygen (N2O-O2) can also relax an anxious dental patient, and N2O itself produces vasodilation.
Nitroglycerin
Premedicating an anxious dental patient with SL NTG before an anxiety-provoking procedure can reduce the chance of an attack. For example, the patient can be given SL NTG a few minutes before a local anesthetic injection.
Because of NTG’s instability, it must be properly stored in the dental office, as previously described, and the expiration date should be checked regularly.
Myocardial Infarction
A patient with symptoms of an anginal attack that is not relieved by SL NTG (1 SL tablet placed under the tongue every 5 minutes for a total of 3 doses) may be experiencing an MI. If the patient who has not been previously diagnosed as having angina experiences chest pain, he or she should be taken to an emergency room for diagnosis. Occasionally, an anginal attack can proceed to an acute MI. For this reason, the dental team should make sure any patient with an attack that is not relieved by NTG is accompanied by an employee to the hospital emergency room.
Antihypertensive agents
Hypertension is the most common cardiovascular disease, affecting some 70 million Americans (33%) and more than 1 billion individuals worldwide. The most recent National Health and Nutrition Examinations Survey (NHANES), for 1999-2006, reported that the prevalence of hypertension increases with age and is higher among women than men (30% versus 28%). The age-adjusted prevalence of hypertension was 41% in non-Hispanic blacks, 28% in non-Hispanics whites, and 22% in Mexican Americans. Data from the Framingham Heart Study suggested that individuals with normal blood pressure at age 55 years have a 90% lifetime risk for development of hypertension. Statistically, it is likely that many dental patients have hypertension because only 68% of patients with diagnosed hypertension are being treated.
In 2013 the Eight Report of the Joint National Committee on the Prevention, Detection, Evaluation and Treatment of High Blood Pressure (JNC 8) presented its most up-to-date guidelines for treating hypertension that were based on many new hypertension observational studies and clinical trials. Normal blood pressure is defined as a systolic pressure less than 120 mm Hg and a diastolic pressure less than 80 mm Hg (120/80 mm Hg). JNC 8 guidelines now consider hypertension for individuals older than 60 years without diabetes or chronic kidney disease to be 150/90 mm Hg or more, higher than the limit established by JNC 7. Hypertension is still a blood pressure of 140/90 mm Hg in persons younger than 60 and all persons with either concomitant diabetes or chronic kidney disease in JNC 8. According to ACC and AHA guidelines, hypertension is a blood pressure 140/90 mm Hg or more for persons younger than 80 years and 150/90 mm Hg or more for persons older than 80 years. When to begin treatment will be dependent on the medical practitioner treating the patient with suspected hypertension. Most commonly, no symptoms are associated with hypertension, which is therefore called the “silent killer.” Complications of hypertension affect organs such as the heart, kidney, and brain as well as the retina. After some damage has occurred, symptoms of malfunction become noticeable.
Eventually, a sustained elevated blood pressure damages the body’s organs, so untreated hypertensive patients are more likely to have kidney and heart disease and cardiovascular problems (MI, cerebrovascular accident). Likelihood of these complications is greatly increased with concomitant smoking.
Fortunately, early detection and treatment with drug therapy (Box 14-4) reduces the possibility of damage to vital organs (reduced morbidity) and extends the patient’s lifetime (reduced mortality). Only about 50% of those with known hypertension are properly treated. If hypertensive patients are properly treated (blood pressure is normalized), their risk of complications is equal to that of patients without hypertension.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses