(1)
Dept. of Oral and Maxillofacial Surgery/Oral Pathology of the VU University Medical Center/ACTA, Amsterdam, The Netherlands
6.1 Introduction
The palate may be the site of various diseases of the oral mucosa and the underlying minor salivary glands. With regard to palatal lesions, it is somewhat artificial to make a distinction between hard and soft palate. Nevertheless, in this chapter, the focus is on lesions of the hard palate.
A limited number of lesions are more or less limited to the palate such as nicotinic stomatitis and angina bullosa hemorrhagica. Also non-Hodgkin lymphoma is one of the diseases that has a predilection for occurrence on the palate.
6.2 Angina Hemorrhagica Bullosa (Blood Blister)
Definition
Angina bullosa hemorrhagica is the Latin term for a blood blister. Some authors refer to this lesion as epidermolysis bullosa acquisita (see also Chap. 2).
Etiology
The etiology is unknown, although trauma is suggested to be the most likely cause.
Epidemiology
Rather rare phenomenon. Occurs more often in women than in men, usually at an older age.
Clinical Aspects
Sudden development of a solitary blood blister accompanied by a painful sensation.
The palate is the site of predilection (Fig. 6.1); other affected sites may be the buccal mucosa and the lateral borders of the tongue. The blister ruptures in a matter of hours, leaving a superficial ulcer behind.


Fig. 6.1
Suddenly arising blood blister (“angina hemorrhagica bullosa”) on the palate
Treatment
Because of the spontaneous rupture of the blister, there is no need for treatment. Some patients will experience recurrences; there are no means to prevent such events.
6.3 Midline Granuloma
Definition
Descriptive, somewhat obsolete, term for an ulcerative lesion in the midline of the hard palate after having excluded any etiologic factor.
Etiology
A midline granuloma is often caused by a natural killer T-cell lymphoma. There are several lesions and conditions that may cause palatal ulceration or even perforation, including malignancies other than lymphomas, Wegener’s granulomatosis, traumatic ulcers due to an ill-fitting denture, third stage of syphilis, and cocaine abuse.
Epidemiology
Rare event.
Clinical Aspects
Ulcerative, destructive changes of the palatal mucosa sometimes resulting in palatal perforation (Fig. 6.2). The differential diagnoses includes Wegener’s granulomatosis (Fig. 6.3), squamous cell carcinoma, non-Hodgkin lymphoma, and a defect due to the use of cocaine.



Fig. 6.2
Midline granuloma after having excluded all other diagnoses, including non-Hodgkin lymphoma

Fig. 6.3
Granulomatous aspect of the palatal mucosa, compatible with a diagnosis of Wegener’s granulomatosis
Treatment
Depends on the final diagnosis.
6.4 Mucormycosis
Definition
Opportunistic mycotic infection.
Etiology
Predisposing factors are dysregulated diabetes mellitus, chronic renal failure, and immunodeficiency.
Clinical Aspects
The typical oral presentation is a dehiscence of the palatal bone that becomes necrotic, acquiring a brown-black appearance (Fig. 6.4).


Fig. 6.4
Rather typical presentation of mucormycosis of the palate
Laboratory Examination
Cytologic smears may be used for the demonstration of the fungus (Fig. 6.5).
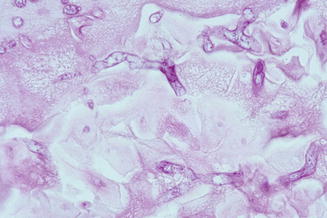
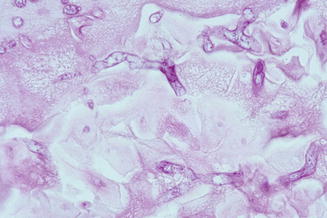
Fig. 6.5
Cytologic aspect of mucormycosis; notice the branching of the fungi
Treatment
Treatment of the underlying cause, if possible. Removal of the necrotic bone. Antifungal treatment, e.g., with high-dose amphotericin B.
6.5 Nasopalatine Duct Cyst
Definition
Developmental non-odontogenic cyst derived from epithelial rests of the nasopalatine duct.
Epidemiology
Rather uncommon cyst that usually does not appear before the age of 30–40 years.
Clinical Aspects
A nasopalatine duct cyst occasionally causes a swelling at the palatal aspect of the upper front teeth, typically located in the midline (Fig. 6.6); the teeth remain vital. In the rare event of occurrence in a child, the typical presentation is just a small, slightly elevated bluish lesion behind the upper incisors (Fig. 6.7). In rare instances, the cyst formation occurs in the papilla incisiva, outside the bone. A nasopalatine duct cyst may also arise in an edentulous part of the alveolar ridge.



Fig. 6.6
Palatal swelling caused by a nasopalatine duct cyst

Fig. 6.7
Typical presentation of a nasopalatine duct cyst in a child
Radiographic Aspects
A nasopalatine duct cyst presents as a round or oval, well-defined radiolucency in or close to the midline, sometimes mimicking a periapical radiolucency (Fig. 6.8). When the teeth are vital, the diagnosis of nasopalatine duct cyst may be made based on the radiograph only, although the differential diagnosis theoretically includes a variety of odontogenic and non-odontogenic cysts and tumors.


Fig. 6.8
The radiograph shows a well-defined radiolucency in the midline; almost diagnostic of nasopalatine duct cyst
Histopathology
The cyst lining consists of stratified squamous epithelium and sometimes cuboidal or ciliated epithelium. In contrast to odontogenic cysts, the cyst wall may contain nerves.
Treatment
An asymptomatic well-defined radiolucency in the midline of the upper front is a rather common incidental finding on a radiograph and does not necessarily require treatment. In the absence of a swelling or symptoms, there is no need for treatment or follow-up. In case of symptoms, enucleation or marsupialization is indicated. Recurrences are rare.
6.6 Palatal Ulcer Due to the Use of Local Anesthetics
Definition
Ulcer of the palatal mucosa due to local injection of an anesthetic solution (see also Chap. 2).
Etiology
A palatal ulcer may be caused by infiltration with a local anesthetic containing epinephrine. This may result a few days later in an ischemic ulcer.
Clinical Aspects
Clinically, a nonspecific, usually painful ulcer near the midline of the palate will be observed (Fig. 6.9a, b). The underlying bone will remain intact. When in doubt about the nature of the ulcer, a biopsy should be taken.
Fig. 6.9
(a) Ulcer caused by an injection with local anesthetics for the removal of 26 a few days before. (b) Spontaneous healing within a month
Histopathology
A biopsy will show necrotic changes of the parenchyma of the palatal salivary glands. The salivary ducts usually persist and may show squamous metaplasia (“necrotizing sialometaplasia”). These changes may mimic a squamous cell carcinoma or a mucoepidermoid carcinoma (Fig. 6.10).
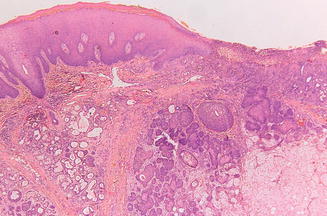
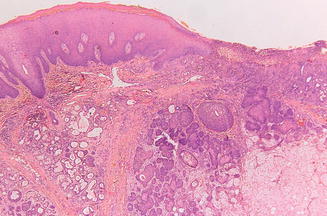
Fig. 6.10
Low-power view of ulcer shown in Fig. 6.9, showing necrotizing sialometaplasia
Treatment
Treatment is not required. Healing takes place in several weeks.
6.7 Papillomatosis of the Palate
Definition
Papillary hyperplasia of the palatal mucosa.
Etiology
Papillomatosis of the palate is mainly observed in denture wearers and is probably caused by wearing the denture day and night. Probably, C. albicans plays a role in the etiology.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


