(1)
Dept. of Oral and Maxillofacial Surgery/Oral Pathology of the VU University Medical Center/ACTA, Amsterdam, The Netherlands
2.1 Introduction
In this chapter, diseases arising from the oral mucosa and soft tissues, such as connective tissue, fat tissue, blood vessels, nerves, and also minor salivary glands, will be discussed. The choice has been made to follow an alphabetical order. Some lesions are grouped together, e.g., fibroma and fibroma-like lesions. A number of the presently discussed lesions and disorders will also be briefly covered in the chapters of the various oral subsites.
2.2 Angioedema
Definition
Sudden vasodilatation caused by histamines and histamine-like substances, followed by plasmatic transudate.
Etiology
C1-esterase inhibitor deficiency in the serum (hereditary type). Allergic reaction, e.g., to drugs such as antibiotics or angiotensin converting enzyme inhibitors (acquired type).
Clinical Aspects
Mainly involvement of the face, lips, eyes, and tongue (Fig. 2.1); occasionally also involvement of the hand and feet. Glottic edema can lead to a life-threatening situation.
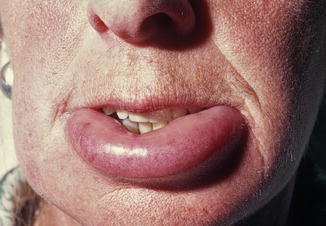
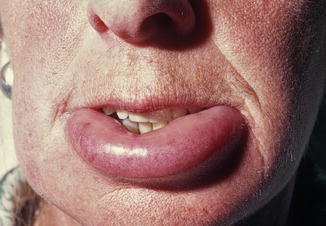
Fig. 2.1
Suddenly arising swelling of the lower lip due to angioedema
Treatment
In case of glottis involvement, it is important to secure a free airway; occasionally, a tracheostomy may be required. In the hereditary type administration of C1-esterase inhibitor concentrate is indicated. In the acquired type, antihistamines may be administered.
2.3 Cysts in the Soft Tissues
Cysts, in general, may be treated by enucleation or by marsupialization (Fig. 2.2a, b). Enucleation aims at removal of the entire cyst, followed by primary closure. In marsupialization just the roof of the cyst is removed, thereby connecting the epithelial cyst lining with the mucosal epithelium.
Fig. 2.2
(a) Schematic drawing of enucleation of a cyst followed by primary closure. (b) Schematic drawing of marsupialization of a cyst
Enucleation is usually performed in small cysts in which complete removal does not interfere with vital structures, e.g., nerves or large blood vessels. Marsupialization is performed in large cysts in which enucleation would carry a risk to damage nerves, e.g., the mandibular nerve, or teeth. The challenge in marsupialization is to prevent the mucosal margins to close again during the postoperative period since that event would result in a “new” cyst. For this purpose, a temporary gauze or an acrylic device can be inserted temporarily into the cavity.
2.3.1 (Epi)dermoid Cyst
Definition
Developmental cyst arising from gastrointestinal epithelium.
Epidemiology
Rather rare cyst.
Clinical Aspects
May become manifest already during infancy or childhood. The most common location is the midline of the floor of the mouth (Fig. 2.3).


Fig. 2.3
Dermoid cyst of the floor of the mouth
Histopathology
Histopathologic examination will show a cyst lined by stratified squamous epithelium (epidermoid cyst); in the presence of adnexal structures (e.g., sebaceous glands or hair follicles), one is dealing with a dermoid cyst (Fig. 2.4b, c).
Fig. 2.4
(a) Gross specimen of well-encapsulated dermoid cyst. (b) Wall of a dermoid cyst containing sebaceous glands
Treatment
Enucleation; recurrences are rare.
2.3.2 Heterotopic Gastrointestinal Cyst
Definition
Developmental cyst characterized by presence of a gastrointestinal epithelial lining of the cyst wall.
Epidemiology
Rare cyst with less than 100 cases published in the literature.
Clinical Aspects
Usually already present at birth or shortly thereafter. Presents itself as a cystic swelling in the anterior part of the floor of the mouth (Fig. 2.5).


Fig. 2.5
Heterotopic gastrointestinal cyst in a young child
Histopathology
The cyst wall is lined by gastrointestinal epithelium (Fig. 2.6). Sometimes it is difficult to really demonstrate the gastrointestinal origin of the epithelial lining.
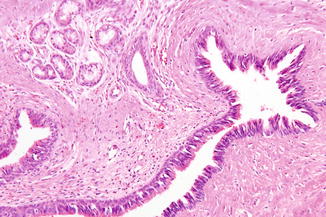
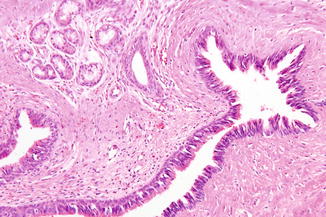
Fig. 2.6
Low-power view of a heterotopic gastrointestinal cyst
Treatment
Enucleation; recurrences are rare.
2.3.3 Lymphoepithelial Cyst (“Oral Tonsil”)
Definition
Developmental cystic lesion, sometimes forming a crypt like in the tonsils, arising from epithelium that has been entrapped in lymphoid tissue; is also referred to as “oral tonsil.”
Epidemiology
Rather rare cyst; may occur at all ages.
Clinical Aspects
Yellowish, circumscribed swelling, asymptomatic otherwise (Fig. 2.7). Usually solitary or multiple presentation. The floor of the mouth and ventral aspect of the tongue are the most common locations. The differential diagnosis includes mainly ranula and lipoma.


Fig. 2.7
Lymphoepithelial cyst (“oral tonsil”) at the ventral aspect of the tongue
Histopathology
The cyst is lined by stratified squamous epithelium and surrounded by lymphoid tissue (Fig. 2.8).
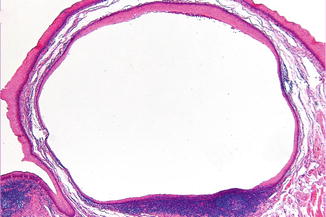
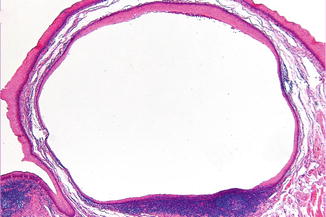
Fig. 2.8
Low-power view of a lymphoepithelial cyst
Treatment
In general removal is recommended, mainly for histopathologic verification. Recurrences have not been reported.
2.3.4 Nasolabial Cyst
Definition
Developmental cyst arising from epithelium enclosed in the lower part of the nasolacrimal duct.
Epidemiology
Rare cyst; mainly diagnosed during adulthood.
Clinical Aspects
Paramedian swelling in the upper mucobuccal fold and, extraorally, of the nasolabial fold (Fig. 2.9). Radiographically, some erosion of the underlying maxillary bone may be observed.


Fig. 2.9
Nasolabial cyst; notice swelling of left nasolabial fold and the bluish swelling in the left nostril
Histopathology
The cyst is lined by cylindrical epithelium (Fig. 2.10). Occasionally, the lining consists of squamous epithelium.
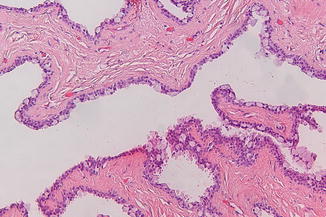
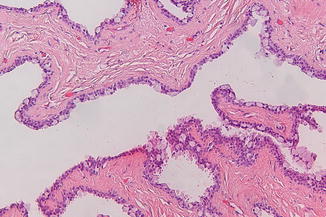
Fig. 2.10
Rather typical histology of nasolabial cyst
Treatment
Enucleation through an intraoral approach; recurrences are rare.
2.3.5 Mucous Retention Phenomenon or Mucous Cyst (Mucocele, Ranula)
Definition
Retention of mucous material in the excretory duct of minor salivary gland or the sublingual gland in case of involvement of the floor of the mouth; occasionally, extravasation in the surrounding connective tissue.
Etiology
Most likely caused by traumatic obstruction of the orificium of the duct.
Epidemiology
Rather common cyst; may occur at all ages.
Clinical aspects
Bluish, non-painful, recurrent cystic swelling. Occurs mainly in the lower lip (mucocele) and in the floor of the mouth (ranula) (Fig. 2.11a, b). Rarely occurs at the ventral aspect of the tip of the tongue (see also Chap. 4) or the palate.
Fig. 2.11
(a) Typical presentation of a mucocele. (b) Typical presentation of a ranula in the floor of the mouth
A special variant of the ranula is the “plunging” ranula, in which the cyst herniates through the mylohyoid muscle, presenting itself as a submental or submandibular swelling. The differential diagnosis of a mucous cyst includes a cystic salivary gland neoplasm, (arterio)venous malformation, and phlebectasia, particularly when located on the lower lip.
Histopathology
Histopathologically, a lumen is seen filled with mucous and cell debris. The lumen may be lined by ductal epithelium (“retention type”); in case of absence of an epithelial lining, one is dealing with the “extravasation type.”
Treatment
A mucocele of the lower lip can usually easily be removed in toto; recurrences are rare. In case of a mucocele at the ventral aspect of the tip of the tongue, the removal of the associated, surrounding minor salivary glands is indicated in order to prevent recurrences.
A ranula is usually primarily treated by marsupialization. In case of recurrence, the removal of the underlying sublingual gland may be required. In case of a “plunging ranula” intraoral removal of the associated sublingual gland usually suffices.
2.3.6 Thyroglossal Duct Cyst
The thyroglossal duct cyst is discussed in the chapter of diseases of the tongue see (Chap. 4).
2.4 Erythroplakia
Definition
Flat erythematous lesion of the oral mucosa that cannot be recognized as any other known erythematous lesion. In fact, it is a definition by exclusion, similarly as applies for the definition of leukoplakia.
Erythroplakia is a premalignant or potentially malignant condition that carries a much higher risk of malignant transformation than leukoplakia. No exact annual malignant transformation figures are available from the literature.
Etiology
Almost exclusively seen in heavy smokers and drinkers.
Epidemiology
Rather rare condition; the estimated prevalence is less than 0.01 %. Rarely occurs below the age of 40 years.
Clinical Aspects
Usually smooth, but sometimes granular, reddish aspect of the mucosa (Fig. 2.12). Often causes symptoms, such as burning or itching. May occur at all sites of the oral cavity.


Fig. 2.12
Erythroplakia of the palate
Clinical Differential Diagnosis
Erythematous candidiasis (usually bilateral and symmetrical), particularly on the dorsal surface of the tongue and on the hard palate.
Erythematous lichen planus (almost always bilateral and symmetrical distribution).
A patient with erythroplakia should always be referred to a specialist for further evaluation.
Histopathology
Histopathologic examination will usually show severe dysplasia, carcinoma in situ, or even squamous cell carcinoma (Fig. 2.13).
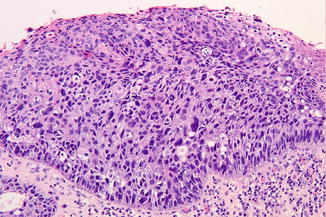
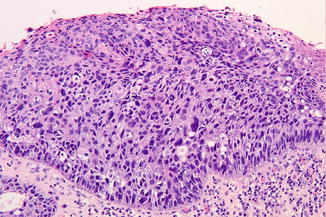
Fig. 2.13
Severe dysplasia or carcinoma in situ
Treatment
Treatment usually consists of surgical removal. CO2-laser vaporation may be considered but has the disadvantage of not providing a surgical specimen for additional histopathologic examination. Photodynamic therapy may be considered in widespread erythroplakia but carries the same disadvantage as being mentioned for laser vaporation.
Long-term (lifelong?) follow-up after treatment is recommended with intervals of not more than 4–6 months.
2.5 Fibroma and Fibroma-Like Lesions
2.5.1 Fibroma
Definition
A fibroma of the oral mucosa represents a hyperplastic lesion rather than a neoplastic one; sometimes the term “fibroepithelial polyp” is used.
The rare “solitary fibrous tumor” of the oral mucosa will not be discussed here; this tumor does not have a characteristic clinical presentation, and the diagnosis is solely based on histologic criteria, resembling the somewhat questionable entity of hemangiopericytoma.
Etiology
Chronic, mechanical irritation caused by habitual biting on the mucosa, by a broken-down dental restoration, or by an ill-fitting partial or full denture. The etiology of “symmetrical fibromas” of the palate or the lingual aspect of the mandible near the trigonum region is unknown.
Clinical Aspects
Often pedunculated, usually solitary lesion, occurring particularly at sites of mechanical irritation such as the buccal mucosa, the tip of the tongue, and along the borders of a denture. In the latter event, the term “denture hyperplasia” or “epulis fissuratum” is used (Figs. 2.14 and 2.15a, b). The consistency of a fibroma may vary from soft to firm elastic. Fibromas are asymptomatic otherwise.


Fig. 2.14
Pedunculated fibroma of the buccal mucosa
Fig. 2.15
(a) Fibrous hyperplasia along the border of an ill-fitting denture (Epulis fissuratum). (b) Clinical aspect after removal of the denture
Symmetrical fibromas may occur on the hard palate and on the lingual aspect of the trigonum region of the mandible (Fig. 2.16).


Fig. 2.16
Symmetrical fibromas of the palate; unknown etiology
Clinical Differential Diagnosis
The differential diagnosis includes lipoma, pyogenic granuloma, and other neoplasms either benign or malignant such as a non-Hodgkin lymphoma or a metastasis. A unilateral fibroma-like lesion on the palate may also be caused by a salivary gland neoplasm.
Multiple fibroma-like swellings may be part of the multiple hamartoma syndrome (Cowden syndrome; a rare hereditary syndrome in which the patient is prone to develop a variety of benign or malignant tumors; see also Chap. 4).
In tuberous sclerosis, a (sometimes hereditary) syndrome in which a variety of abnormalities may occur, oral involvement consists a.o. of fibrous hyperplasia of the oral mucosa and the gingiva (Figs. 2.17 and 2.18), enamel pitting, and radiolucencies in the jaws based on fibrous connective tissue that may cause eruption disturbancies.



Fig. 2.17
Fibrous hyperplasia in left part of the mandible in a patient suffering from tuberous sclerosis

Fig. 2.18
Fibrous hyperplasia of buccal mucosa in a patient suffering from tuberous sclerosis
In Crohn’s disease, fibroma-like swellings of the buccal mucosa may occur. These swellings may have a cobble stone appearance (Fig. 2.19a, b).
Fig. 2.19
(a) Fibrous swellings in a patient suffering from Crohn’s disease. (b) Notice the cobble stone appearance of the buccal mucosa
Histopathology
On histopathologic examination of a fibroma fibrous tissue is seen with or without the presence of an inflammatory infiltrate. Occasionally, stellate-like, large fibroblasts are observed, referred to as “giant cell fibroma”; this histopathologic subtype does not have any clinical relevance (Fig. 2.20a, b).
Fig. 2.20
(a) Low-power view of a fibroma. (b) Stellate-like, large fibroblasts in giant cell fibroma
Treatment
Elimination of the etiologic factor, if identified, is sometimes effective. If not, excision and histopathologic verification may be considered. Recurrences are rare.
2.5.2 Lipoma
Definition
Benign neoplasm of fat cells.
Clinical Aspects
Fibroma-like appearance, sometimes showing a somewhat yellowish color, having a soft consistency (Fig. 2.21), being otherwise asymptomatic. Bilateral, symmetrical occurrence is extremely rare.
Fig. 2.21
Lipoma in the mucobuccal fold of the mandible
Histopathology
Histopathologically, mature, well-encapsulated fat cells are seen (Fig. 2.22). There are a few histologic subtypes such as fibrolipoma and angiolipoma; these subtypes are not of clinical significance. The malignant variant of a lipoma, referred to as liposarcoma, rarely occurs in the mouth.
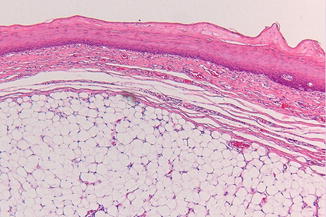
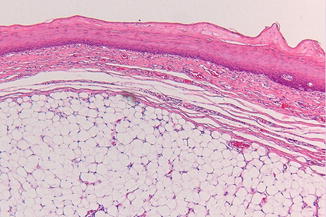
Fig. 2.22
Low-power view of a lipoma
Treatment
Surgical removal. Lipomas rarely, if ever, recur.
2.5.3 Mucinosis, Focal
Definition
Rare, somewhat questionable entity of unknown etiology, possibly representing the counterpart of cutaneous focal mucinosis; may be just a fibroma with myxoid changes of the connective tissue.
Clinical Aspects
Pedunculated, fibroma-like swelling that may occur on the gingiva, palate, and buccal mucosa, being asymptomatic otherwise (Fig. 2.23).
Fig. 2.23
Fibroma-like swelling of focal mucinosis
Histopathology
Histopathologically, a somewhat circumscribed myxoid fibromatous lesion can be observed without the presence of an inflammatory infiltrate (Fig. 2.24).
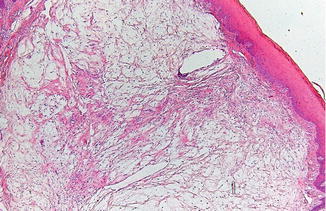
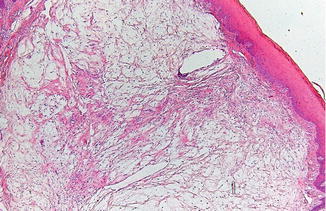
Fig. 2.24
Low-power view of focal mucinosis
Treatment
Surgical removal.
2.5.4 Neurofibroma
Definition
Benign neoplasm derived from perineural fibroblasts and Schwann cells; can be part of hereditary neurofibromatosis type I.
Epidemiology
Rather uncommon tumor of the oral soft tissues.
Clinical Aspects
Solitary or multiple firm-elastic swelling of the oral mucosa, usually asymptomatic otherwise. The tongue and the buccal mucosa are the sites of predilection. Occasionally, the palate is involved (Fig. 2.25).
Fig. 2.25
Neurofibroma of the palate in patient suffering from neurofibromatosis
Histopathology
Histopathologically, the lesion is usually well circumscribed. Proliferation of spindle cells in a collagen-rich matrix can be observed (Fig. 2.26).
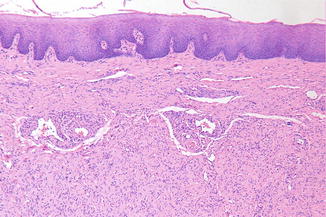
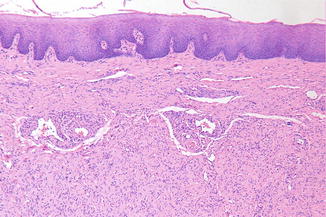
Fig. 2.26
Low-power view of neurofibroma
Treatment
A solitary neurofibroma can be removed by surgical excision. In patients suffering from neurofibromatosis type I, malignant transformation may occur. Because of the often widespread occurrence throughout the body, prophylactic removal of these neurofibromas is not feasible. Instead, regular, lifelong follow-up is recommended.
2.5.5 Neurilemmoma (Schwannoma)
Definition
Benign neoplasm derived from Schwann cells.
Epidemiology
Rare intraoral neoplasm.
Clinical Aspects
Circumscribed firm-elastic swelling, usually asymptomatic otherwise (Fig. 2.27).
Fig. 2.27
Neurilemmoma at the border of the tongue
Histopathology
Histopathologically characterized by two cell types, being “ Antoni-A cells” (with elongated nuclei and arranged in a palisade pattern around acellular collagen-like structures, so-called Verocay bodies) and Antoni-B cells (Fig. 2.28).
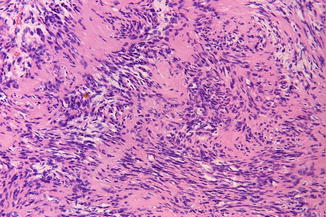
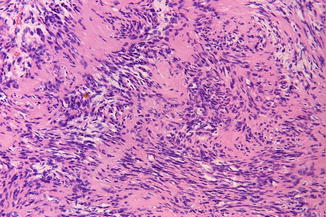
Fig. 2.28
Neurilemmoma; the pinkish material represents the Verocay bodies
Treatment
Surgical removal.
2.5.6 Neuroma
Definition
Proliferation of neural structures caused by trauma (“traumatic neuroma”). Multiple mucosal neuromas are indicative of the hereditary multiple endocrine neoplasia (MEN) type 2B syndrome, also referred to as Sipple syndrome (Fig. 2.29).
Fig. 2.29
Multiple neuromas in MEN type 2B (a and b)
Clinical Aspects
Circumscribed solitary or multiple swellings of the lower lip or the tongue, sometimes painful. In case of multiple neuromas, the lips, tongue buccal mucosa, gingiva, and palate may be involved.
Histopathology
The histopathology is characterized by a haphazard proliferation of nerve bundles. In MEN type 2B syndrome, distinct hyperplasia of nerve bundles can be seen.
Treatment
A traumatic neuroma can be excised, together with a part of the associated nerve bundle.
In MEN type 2B, the emphasis is on early detection of the possible development of thyroid cancer.
2.5.7 Pyogenic Granuloma (“Lobular Capillary Hemangioma”)
Definition
Excessive tissue reaction to nonspecific local irritation. In the past believed to be caused by pus-producing microorganisms, hence the adjective “pyogenic.” Is by some regarded as a vascular lesion (“lobular capillary hemangioma”).
Clinical Aspects
Soft, pedunculated, and usually partly ulcerative swelling, usually asymptomatic otherwise (Fig. 2.30). May occur at any site in the oral cavity, except for the floor of the mouth.
Fig. 2.30
Pyogenic granuloma of the buccal mucosa
Histopathology
Vascular spaces surrounded by clusters of endothelial cells (“lobular capillary hemangioma”); there may be secondary signs of inflammation (Fig. 2.31).
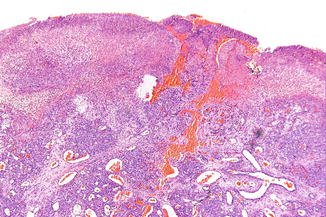
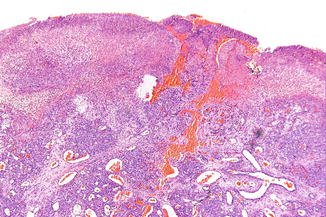
Fig. 2.31
Low-power view of pyogenic granuloma
Treatment
Conservative surgical excision; recurrences are rare.
2.5.8 Mucosal Nodules in Sarcoidosis
Definition
Generalized granulomatous disease.
Etiology
Unknown.
Epidemiology
Rather uncommon disease; may become manifest during adolescence.
Clinical Aspects
In 90 % of patients suffering from sarcoidosis, the lungs are involved. Oral involvement is rare and consists of solitary or multiple nodules of the oral mucosa (Fig. 2.32).


Fig. 2.32
Nodular swelling caused by sarcoidosis
Histopathology
Histopathologically, noncaseating granulomas are observed (“sarcoid granulomas”); these do not allow to make a firm diagnosis of sarcoidosis and require additional medical examination (Fig. 2.33).
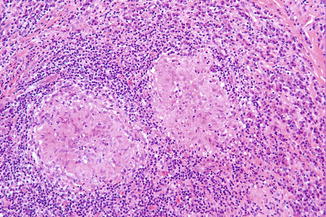
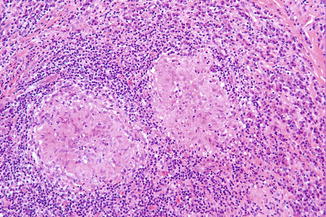
Fig. 2.33
Sarcoid granulomas, suggestive but not diagnostic of sarcoidosis
Treatment
Treatment is only indicated in active disease and usually consists of systemic administration of corticosteroids.
2.5.9 Nodular Presentation of Sialoadenitis of Minor Salivary Glands
Definition
Inflammation of minor salivary glands. Subacute necrotizing sialadenitis (SANS) of the palate is a separate entity that will be discussed in Chap. 6.
Epidemiology
Usually in adults and elderly patients.
Etiology
Probably the result of an ascending infection from the oral flora through the excretory ducts of the minor salivary glands (“retrograde” infection).
Clinical Aspects
Occurs mainly in the upper and lower lip (cheilitis glandularis; see also Chap. 3) and the buccal mucosa. Presents as recurrent, solitary, or multiple firm-elastic swellings of the mucosa (Fig. 2.34). Sometimes painful and occasionally resulting on abscess formation. On careful massage of the nodule(s), some mucopurulent discharge may be observed.


Fig. 2.34
Sialoadenitis of minor salivary glands; notice the mucous discharge
In case of a solitary swelling of the oral mucosa, the possibility of a salivary gland neoplasm should be considered as well as the rare event of a sialolith. The final diagnosis can only be established by histopathologic examination.
Nodular lesions of the lips and the cheek may also be the result of a foreign body reaction to fillers.
Histopathology
Histopathologic examination shows a nonspecific inflammatory reaction in the salivary gland tissue (Fig. 2.35).
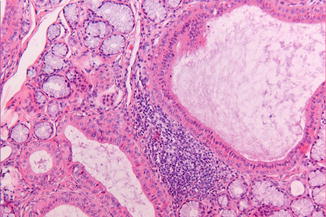
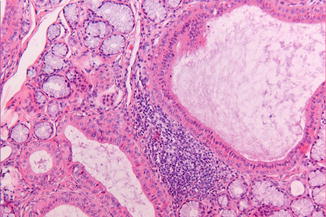
Fig. 2.35
Dilated excretory ducts surrounded by an inflammatory infiltrate in sialoadenitis
Treatment
In case of a solitary lesion, a biopsy is usually sufficient; in case of multiple lesions, the treatment policy is mainly guided by the presence of symptoms.
2.5.10 Fibroma-like Lesions or Nodules Caused by Salivary Gland Tumors of the Intraoral Glands
Definition
Tumor usually arising from the parenchymal epithelial salivary gland tissue and rarely from the stromal part of the salivary glands.
Etiology
Unknown; in an occasional patient, there is a history of previous irradiation in the head and neck region that may have caused the tumor.
Epidemiology
The incidence of salivary gland tumors, including the ones that occur in the major salivary glands, is approximately 3 per 100,000 population per year, for benign and malignant tumors together. May occur at all ages, although occurrence in children is rather rare.
Clinical Aspects
Usually a slowly growing, firm-elastic fibroma-like swelling, sometimes of cystic consistency, of the oral mucosa, being asymptomatic otherwise. Sites of preference are the palate, particularly at the junction of the hard and soft palate (see also Chap. 6), the upper lip and, rarely, the buccal mucosa and the floor of the mouth (see also Chap. 3) (Fig. 2.36).
Fig. 2.36
Salivary gland tumor; the biopsy showed a mucoepidermoid carcinoma
The percentage of occurrence in all salivary glands is as follows:
-
Parotid gl. : submandibular gl. : sublingual gl.: intraoral (accessory gl.) = 100: 10: 1: 10. In the parotid gland, the majority of the neoplasms is benign, while in the intraoral glands some 50 % are malignant.
Based on the clinical signs and symptoms, no reliable distinction can be made between a benign or a malignant salivary gland tumor, and in all instances, a biopsy is required, preferably taken in the center of the swelling and deep enough to obtain representative tissue.
Histopathology
Histopathologically, there is a wide range of benign and malignant salivary gland tumors (Table 2.1). It may be difficult for the pathologist to provide a firm histopathologic subtype of a salivary gland tumor based on a biopsy.
Table 2.1
Classification of salivary gland tumors
|
Benign
|
|
Pleomorphic adenoma
|
|
Basal cell adenoma
|
|
Warthin tumor
|
|
Canalicular adenoma
|
|
Ductal papilloma
|
|
And several other, rare subtypes
|
|
Malignant
|
|
Acinic cell carcinoma
|
|
Mucoepidermoid carcinoma
|
|
Adenoid cystic carcinoma
|
|
Salivary duct carcinoma
|
|
Adenocarcinoma, not otherwise specified
|
|
Carcinoma ex pleomorphic adenoma
|
|
And several other, rare subtypes
|
The adenoid cystic carcinoma is a rare intraoral salivary gland tumor known for its perineural spread (Fig. 2.37) and rather poor prognosis.
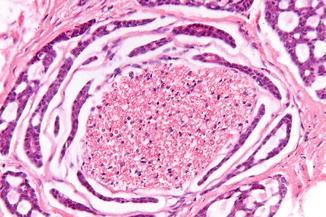
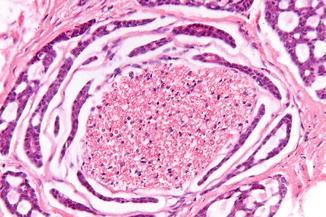
Fig. 2.37
Perineural spread of adenoid cystic carcinoma
Treatment
Surgical removal; postoperative irradiation on indication. Malignant salivary gland tumors may metastasize to the cervical lymph nodes. The adenoid cystic carcinoma often produces distant metastases, skipping the regional lymph nodes in the neck.
2.5.11 Fibroma-Like Swelling Caused by a Sialolith
Definition
A sialolith (calculus formation) in the duct of a minor or major salivary gland; occasionally in the gland itself, e.g., in the submandibular or the parotid gland.
Etiology
Deposition of debris possibly caused by infection and followed by calcification. There is no association between calculus formation in the salivary glands and other organs, e.g., kidney and gall bladder.
Epidemiology
Rather rare event; usually at middle age but may occur in children as well.
Clinical Aspects
Sialoliths mainly occur in the submandibular glands or their excretory ducts and are usually associated with symptoms of a painful, recurrent submandibular swelling, particularly during meals. Occasionally presents as a swelling in the floor of the mouth (Fig. 2.38a). The diagnosis is confirmed by the findings on an occlusal radiograph (Fig. 2.38b) or a (cone beam) CT (Fig. 2.38c, d).
Fig. 2.38
(a) Swelling in the floor of the mouth caused by an underlying sialolith. (b) Occlusal radiograph shows a sialolith. (c) CT scan of another patient shows a small sialolith. (d) 3D image of c.
Occurrence of a sialolith in a minor salivary gland is quite rare; the usual presentation is a small nodule in the upper lip.
Treatment
Treatment consists usually of surgical removal. In most cases of involvement of the submandibular ductal system, there is no need to also remove the associated submandibular gland. Some clinicians prefer to apply lithotripsy. Removal of a sialolith in the parotid gland is more cumbersome; sometimes sialoendoscopic removal is possible. An intraoral sialolith can be simply enucleated (Fig. 2.39).
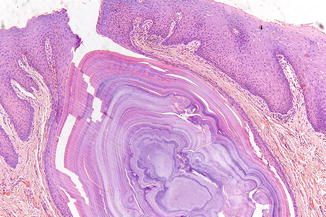
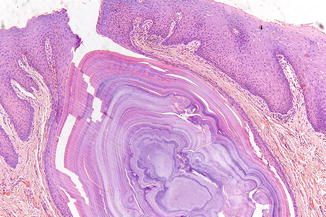
Fig. 2.39
Sialolith removed from the upper lip
2.6 Fordyce’s Spots
Definition
Ectopic sebaceous glands in the oral mucosa.
Etiology
Developmental anomaly.
Epidemiology
Is present in various amounts in almost all people. Fordyce’s spots become manifest during adulthood.
Clinical Aspects
Usually multiple pinpoint-sized yellowish granules; may occur everywhere in the oral cavity but sites of preference are the buccal mucosa and the upper lip (Fig. 2.40). Fordyce’s spots do not cause any symptoms. In rare cases, Fordyce’s spots become hyperplastic or even cystic. There is rarely a need for histopathologic confirmation.


Fig. 2.40
Fordyce’s spots in the buccal mucosa
Histopathology
Normal sebaceous glands without hair follicles (Fig. 2.41).
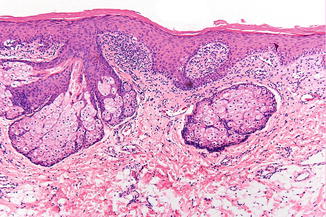
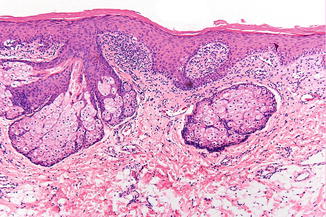
Fig. 2.41
Low-power view of Fordyce’s spots
Treatment
No treatment required.
2.7 Fungal Diseases
2.7.1 Actinomycosis
Definition
Acute or chronic infection of the cervicofacial region caused by actinomycetes. Actinomycetes are actually no fungi but normal, saprophytic bacteria of the oral flora. There are several subclasses of actinomycetes such as A.israelii and A. viscosus.
Etiology
Trauma, e.g., a tooth extraction, may be the “port d’entrée” of the infection, resulting in abscess formation that ultimately may cause a cutaneous fistula. In most cases, there is an interval of some months between the extraction and the clinical presentation of the disease.
Epidemiology
Rather rare disease in the head and neck region.
Clinical Aspects
Usually presenting as a firm infiltrate or abscess, showing a bluish-reddish discoloration of the overlying skin (Fig. 2.42).


Fig. 2.42
Cervicofacial actinomycosis 2 months after a tooth extraction
Laboratory Examination
Culturing of pus or infected tissue does not always demonstrate the presence of actinomycetes; in a number of such cases, histopathologic examination is helpful (Fig. 2.43).
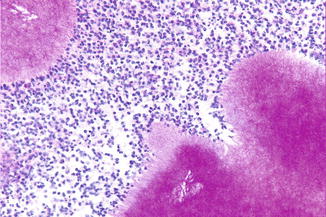
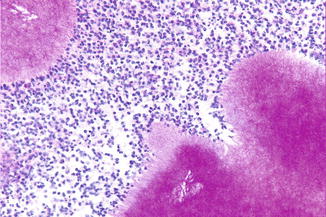
Fig. 2.43
Actinomyces colonies (PAS stain)
Treatment
Surgical drainage and debridement followed by a 6–12-week course of penicillin.
2.7.2 Candidiasis
Definition
Fungal infection caused by one of the Candida species, most often being C. albicans.
Etiology
C. albicans occurs in the oropharyngeal cavity in approximately 40 % of the population without causing signs or symptoms. Local and systemic factors may lead to a disease state, referred to as candidiasis. Local predisposing factors may be poor oral hygiene, dry mouth, topical use of corticosteroids, e.g., in the form of inhalers, smoking, and irradiation of the head and neck.
Systemic predisposing factors consist of immunodeficiencies (e.g., HIV infection), diabetes mellitus, malnutrition, hematologic disorders such as leukemia, and prolonged use of antibiotics.
Clinical Aspects
There are several clinical manifestations; these may occur simultaneously in an individual patient. There is almost always a bilateral, more or less symmetrical pattern.
The pseudomembranous type (“thrush”) is characterized by white plaques that can be easily wiped off from the mucosal surface (Fig. 2.44); this type mainly occurs on the buccal mucosa and the tongue. Symptoms may consist of a burning sensation and an abnormal taste.
Fig. 2.44
Pseudomembranous candidiasis; notice the bilateral distribution
The erythematous type is characterized by sometimes painful, fiery red changes of the mucosa, particularly occurring on the palate and the dorsum of the tongue (Fig. 2.45). Median rhomboid glossitis is regarded as a variant of erythematous candidiasis (see Chap. 4), being sometimes associated with erythematous candidiasis of the palate (“kissing lesion”); C. albicans may also play a role in angular cheilitis (“perlèches”); furthermore, denture stomatitis may be a variant of erythematous candidiasis, although the etiologic role of C. albicans in this condition is less convincing than has been thought in the past. In the absence of a bilateral distribution, the clinician should consider a diagnosis of erythroplakia, being a rare but serious premalignant disorder.
Fig. 2.45
Erythematous candidiasis of the palate; bilateral distribution
The hyperplastic type is characterized by a white patch that cannot be scraped off, occurring particularly in the corners of the mouth and on the dorsal surface of the tongue; some clinicians regard these lesions as Candida-associated leukoplakias.
The mucocutaneous type is caused by an underlying immune disorder and affects the oral mucosa, the skin, and nails. This rare entity will not be discussed here any further.
In most instances, the diagnosis “candidiasis” is a clinical one, either based on the clinical presentation or on a positive response to antifungal treatment.
Laboratory Studies
Exfoliative examination applying KOH may be considered but can in most cases be omitted. Culturing C. albicans is not very common as a routine procedure either.
In the hyperplastic type, one may consider to perform a biopsy. In such event hyperplastic, parakeratotic epithelium can be observed with hyphae penetrating the epithelium (Fig. 2.46); in the superficial epithelium, microabscesses may be encountered. There may be varying degrees of chronic inflammation in the subepithelial connective tissue and sometimes also presence of neutrophils in the epithelium.
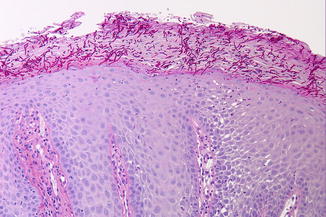
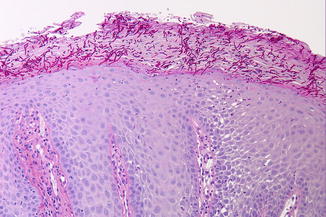
Fig. 2.46
Hyphae of C. albicans penetrating the superficial layer of the epithelium (PAS stain)
Treatment
Treatment is mainly indicated in symptomatic cases and should primarily be directed at elimination of predisposing factors, if any. In many cases, topical antifungal treatment for a few weeks is sufficient; only in persistent cases, systemic antifungal treatment is indicated.
2.8 Hemangioma and Hemangioma-Like Lesions
2.8.1 Angina Hemorrhagica Bullosa
Definition
Angina hemorrhagica bullosa is the Latin term for a painful blood blister.
Etiology
Unknown; some patients report that the lesion arose after eating hard food substances.
Epidemiology
Rather rare event; mainly in adults and probably more often in women.
Clinical Aspects
The blister suddenly appears and is often associated with pain. The palate, buccal mucosa, and the borders of the tongue are the sites of preference (Fig. 2.47). The blister ruptures soon after its development, leaving a superficial erosion of the mucosa behind (Fig. 2.48a, b).


Fig. 2.47
Angina hemorrhagica bullosa in the cheek
Fig. 2.48
(a) Angina hemorrhagica bullosa on the palate. (b) Clinical aspect after rupture of the blister
Treatment
Treatment is rarely required since the blister ruptures soon after its development. Further healing takes place without scar formation.
Recurrence
Some patients will experience repeated recurrences. Unfortunately, no preventive measures can be taken.
2.8.2 Phlebectasia (“Varicosity”)
Definition
Local dilatation of a small vein.
Etiology
Is most likely an aging phenomenon and is the result of local weakness of the vascular wall. Is not a sign of cardiopulmonal disease.
Epidemiology
Common phenomenon in middle-aged and elderly people.
Clinical Aspects
Solitary or multiple bluish swellings ranging from a few millimeters up to a centimeter (Fig. 2.49). The borders and the ventral aspect of the tongue and also the lips are the sites of preference. Phlebectasias are asymptomatic otherwise. There is rarely a need for histopathologic confirmation.


Fig. 2.49
Phlebectasia on the lower lip
Histopathology
Vascular spaces filled with erythrocytes (Fig. 2.50a). Thrombus formation may occur, sometimes accompanied by intravascular papillary endothelial hyperplasia. In such instance, the term “Masson tumor” has been used in the past; this benign lesion can be misdiagnosed as an angiosarcoma (Fig. 2.50b).
Fig. 2.50
(a) Low-power view of phlebectasia. (b) Intravascular papillary endothelial hyperplasia of the lower lip
Treatment
Not required, although patients occasionally ask for removal because of esthetic reasons.
2.8.3 Hemangioma and Arteriovenous Malformations
Definition
The majority of the so-called hemangiomas of the oral mucosa and soft tissues are present already at birth or shortly thereafter and represent a malformation of blood vessels or lymphatic vessels (lymphangioma) rather than a neoplasm. There is, however, a rare “true” hemangioma that arises shortly after birth, showing rapid proliferation followed by spontaneous involution during childhood (Fig. 2.51). The present text focusses on the arteriovenous malformations.


Fig. 2.51
True, fast-growing hemangioma in a 1-year-old
Clinical Aspects
Red or bluish swelling of the oral mucosa, with or without pulsations, being usually asymptomatic otherwise. Only in arterial malformations repeated and severe spontaneous bleeding may occur. The lips, the tongue, and the buccal mucosa are the sites of preference (Fig. 2.52). Occasionally, calcified structures may be observed on a plain radiograph due to calcifications of thrombosed tissue; these are referred to as phleboliths (Fig. 2.53).

Fig. 2.52
Venous malformation in an adult, present from early childhood

Fig. 2.53
Multiple phleboliths in a venous malformation of the left side of the neck
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


