(1)
Dept. of Oral and Maxillofacial Surgery/Oral Pathology of the VU University Medical Center/ACTA, Amsterdam, The Netherlands
5.1 Introduction
The majority of diseases of the oral mucosa may also affect the gingiva and the mucosa of the alveolar ridges in edentulous part of the jaws. Some mucosal diseases rarely involve the gingiva, e.g., aphthous ulcers. On the other hand, there are diseases that only occur on the gingiva. In this chapter, examples of both categories of diseases will be discussed.
5.2 Cysts
5.2.1 Eruption Cyst
Definition
Odontogenic developmental cyst that can be regarded as a dentigerous or follicular cyst of an erupting tooth, usually a deciduous tooth. Some prefer to call this cyst an “eruption hematoma,” suggesting that the lesion is caused by trauma during eruption resulting in a hematoma.
Epidemiology
Not very common phenomenon; no gender preference.
Clinical Aspects
Bluish, cystic lesion on the alveolar ridge at the site of an erupting tooth, usually a deciduous molar in the upper jaw (Fig. 5.1). It is questionable whether an eruption cyst is painful. The general belief is that it is not. The diagnosis can usually be made on clinical grounds alone without the need for a radiograph to demonstrate the presence of an underlying erupting tooth. A biopsy is only indicated in case of doubt.


Fig. 5.1
Eruption cyst of 54
Treatment
Treatment is not required. The underlying tooth will erupt in a normal way. Sometimes the parents insist on having the overlying operculum excised.
5.2.2 Gingival Cyst of the Adult
Definition
Odontogenic developmental cyst in the gingiva of an adult is to be regarded as the extraosseous counterpart of the intraosseous lateral periodontal cyst.
Epidemiology
Rather rare cyst; no gender preference.
Clinical Aspects
Cystic, often bluish lesion of the alveolar mucosa on the buccal aspect of a tooth, usually in the anterior region of the mandible or maxilla (Fig. 5.2). The gingival cyst is asymptomatic otherwise. Usually, a radiograph (periapical film) is taken to exclude the presence on an underlying intraosseous lesion.


Fig. 5.2
Gingival cyst in an adult
Histopathology
Thin epithelial lining that may show features of a lateral periodontal cyst, such as formation of epithelial “plaques.”
Treatment
Treatment consists of conservative excision; the cyst rarely recurs.
5.2.3 Gingival Cyst of the Newborn (“Dental Lamina Cyst of the Newborn”)
Definition
Odontogenic developmental cyst on the alveolar ridge of a newborn.
Epidemiology
Probably quite common cyst.
Clinical Aspects
Solitary or multiple whitish-grayish nodules on the upper or lower alveolar ridge (Fig. 5.3). The diagnosis is a clinical one; only in rare instances, the taking of a biopsy may be considered.


Fig. 5.3
Multiple gingival cysts in a newborn (“dental lamina cyst”); no treatment indicated
Treatment
The cyst(s) will disappear spontaneously in a matter of weeks or a few months.
5.3 Epulis
Definition
Epulis is a clinical term for a localized swelling of the gingiva. It is, therefore, not a final diagnosis. Various diseases may present as a localized swelling of the gingiva. The “epulis of the newborn,” consisting of granular cells resembling somewhat a granular cell tumor, will be discussed separately.
Epulis fissuratum, also referred to as “denture fibrous hyperplasia,” has been dealt with in the paragraph on fibroma (see Chap. 2).
Etiology
The majority of epulides are caused by local irritation, e.g., by the presence of calculus, and consist of fibrous tissue such as is observed in fibrous hyperplasia. A fibrous epulis may occur during pregnancy, being referred to as pregnancy tumor. Epulis-like swellings of the gingiva may also be a side effect of some drugs, e.g., amlodipine.
Epidemiology
Rather common gingival swelling that may occur at all ages.
Clinical Aspects
Usually somewhat pedunculated swelling between two or more teeth, often only at the buccal side but sometimes also extending to the palatal side (Figs. 5.4a, b and 5.5a, b). The size may vary from a few millimeters to a few centimeters. The color may vary from that of the normal gingiva to a more bluish color in case of a peripheral giant cell lesion. There are usually no symptoms. The taking of a periapical film is recommended to exclude the presence of an underlying expanding intraosseous lesion. The differential diagnosis of an epulis includes:
Fig. 5.4
(a) Local swelling of the gingiva (“epulis”). (b) Clinical aspect 3 months after excision
Fig. 5.5
(a) Pregnancy tumor in the mandible. (b) Spontaneous regression within a few months after the delivery
-
Metastasis of a malignancy located elsewhere in the body (Fig. 5.6)
 Fig. 5.6Epulis caused by a metastasis of a cancer of the kidney
Fig. 5.6Epulis caused by a metastasis of a cancer of the kidney -
Peripheral giant cell lesion (Fig. 5.9a, b)
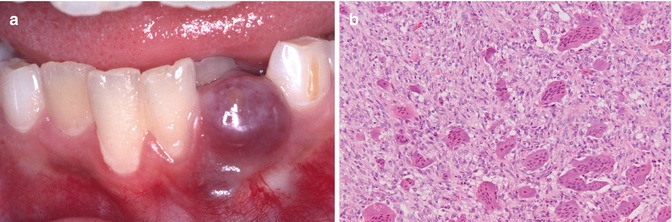 Fig. 5.9(a) Peripheral giant cell lesion. (b) Low-power view of peripheral giant cell lesion
Fig. 5.9(a) Peripheral giant cell lesion. (b) Low-power view of peripheral giant cell lesion -
Squamous cell carcinoma (Fig. 5.10)
 Fig. 5.10Squamous cell carcinoma of the gingiva and alveolar mucosa
Fig. 5.10Squamous cell carcinoma of the gingiva and alveolar mucosa -
Sarcoma (Fig. 5.11)
 Fig. 5.11Fibrosarcoma of the gingiva and alveolar mucosa
Fig. 5.11Fibrosarcoma of the gingiva and alveolar mucosa
Histopathology
The majority of epulides will show fibrous hyperplastic tissue with or without signs of inflammation. In case of the presence of bone formation, the term “peripheral ossifying fibroma” is applied (Fig. 5.12). This lesion is not considered to be the extraosseus counterpart of the central ossifying fibroma. In the presence of odontogenic epithelium, the term “peripheral odontogenic fibroma” is applied, being the extraosseous counterpart of the rare intraosseous odontogenic fibroma. In the presence of multinucleated giant cell, the term peripheral giant cell lesion is applied.
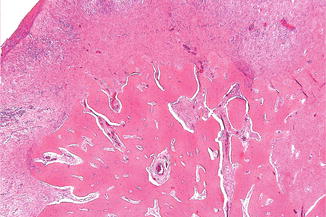
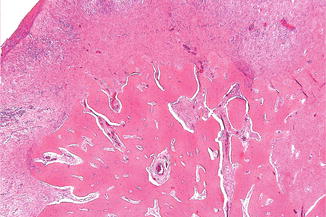
Fig. 5.12
Low-power view of peripheral ossifying fibroma
Treatment
Treatment of an epulis consists of excision. The underlying periosteum should be thoroughly curetted in order to minimize the risk of recurrence. Possible present calculus should be removed as well. Sometimes, an epulis behaves in a rather aggressive way by repeated recurrences after removal.
5.4 Exostoses
Definition
Exostoses are bony excrescencies that may occur on the buccal aspect of the maxillary or mandibular gingiva.
Etiology
Multiple exostoses of the gingiva are supposedly caused by chronic periodontal irritation.
However, when this hypothesis is true, one would expect to see these exostoses much more often.
Epidemiology
Occur exclusively in elderly people.
Clinical Aspects
Multiple bony, hard, localized swellings at the buccal aspect of the gingiva in the maxilla or mandible, being asymptomatic otherwise (Fig. 5.13).


Fig. 5.13
Multiple exostoses at the buccal aspect of the maxilla
Treatment
Surgical correction is only indicated in case of interference with the wearing of a denture.
5.5 Fibromatosis of the Gingiva
Definition
Generalized fibrous swelling of the gingiva.
Etiology
May be a side effect of certain drugs, e.g., phenytoine and cyclosporine. In the absence of a causative factor, the term idiopathic fibromatosis is used.
Clinical Aspects
Multiple fibrous swellings of the gingiva in the mandible and maxilla, being asymptomatic otherwise (Fig. 5.14). May cause eruption disturbances when occurring in children (Fig. 5.15a, b). In rare instances, a fibroma-like swelling of the gingiva or alveolar mucosa is based on a leukemic infiltrate (Fig. 5.16). Furthermore, there is a rare autosomal dominant syndrome consisting of fibromatosis of the gingiva and hypertrichosis on the face, the midback, and the extremities (“gingival fibromatosis-hypertrichosis syndrome”).


Fig. 5.14
Drug-induced fibromatosis of the gingiva
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses