Fig. 2.1
Measurement of the unstimulated whole saliva flow rate using the drooling method
Autoimmune Diseases
Autoimmune diseases include a large number of chronic inflammatory connective tissue diseases like Sjögren’s syndrome, rheumatoid arthritis, systemic lupus erythematosus and scleroderma, but also sarcoidosis, inflammatory bowel diseases and endocrine diseases. Overlap between the various autoimmune diseases is common.
Chronic Inflammatory Connective Tissue Diseases
Sjögren’s Syndrome
Sjögren’s syndrome (SS) is a chronic, systemic autoimmune inflammatory disorder that affects the exocrine glands and particularly the salivary and lacrimal glands [11]. The most prominent disease manifestations include hyposalivation and keratoconjunctivitis sicca, which result in symptoms of oral and ocular dryness. Although characterised as an exocrinopathy, non-exocrine organs may also be affected [11, 12]. The aetiology remains unknown, but most likely includes an interaction between immunological, genetic, hormonal and environmental factors. SS can occur at all ages, but the median age of presentation is around 50 years. A female preponderance is seen with a female to male ratio of 9:1 [11, 12]. Diagnosis is often delayed which reflects the fact that the onset of disease is often insidious, and patients often present various and non-specific symptoms like fatigue, myalgia, arthralgia and intermittent fever [11–13]. SS can occur alone as primary SS or in conjunction with another chronic inflammatory connective tissue disease such as rheumatoid arthritis, systemic lupus erythematosus, scleroderma or mixed connective tissue disease, designated as secondary SS [14]. The prevalence of primary SS is about 0.6 %, but the prevalence varies depending on the population sampled and the diagnostic criteria used [15]. At present, there are no specific diagnostic tests for SS. The diagnosis is based on a combination of questions regarding oral and ocular symptoms and clinical tests for evaluation of the salivary and lacrimal gland function as well as labial salivary gland biopsy and serological analysis for presence of serum autoantibodies (anti-Ro/SSA and anti-La/SSB) [16]. The classification criteria for SS currently used by clinicians and researchers around the world are the American-European Consensus Classification Criteria [16] (Table 2.1). The diagnosis of SS requires presence of focal lymphocytic infiltrates in the labial salivary glands and/or presence of serum autoantibodies as indicators of autoimmune activity [16]. Recently, a new set of classification criteria was proposed that are based entirely on objective measures [17]. At present, there is no curative therapy for SS, and current management is mainly symptomatic. Patients with SS are at risk of developing diseases of the oral hard and soft tissues due to hyposalivation and therefore require special attention by the dentist.
Table 2.1
American-European classification criteria for Sjögren’s syndrome [16]
|
I. Ocular symptoms, positive response for at least one of the following questions
|
|
1. Have you felt your eyes dry for the past 3 months?
|
|
2. Do you have a recurrent feeling of sand in your eyes?
|
|
3. Do you use tear substitutes more than 3 times a day?
|
|
II. Oral symptoms, positive response for at least one of the following questions
|
|
1. Have you felt your mouth dry for the past 3 months?
|
|
2. Have you had persistent or recurrent swollen salivary glands in your adult life?
|
|
3. Do you normally drink liquids to help you swallow dry foods?
|
|
III. Ocular impairment signs, positive results in one of the two following tests
|
|
1. Schirmer I test (≤5 mm/5 min)
|
|
2. Rose bengal staining (≥4 according to van Bijsterveld’s scoring system)
|
|
IV. Histopathology: presence of focal lymphocytic infiltration with focus score ≥1 in minor salivary gland biopsy
|
|
V. Salivary gland involvement, positive results in one of the two following tests
|
|
1. Whole saliva sialometry ≤1.5 ml/15 min
|
|
2. Parotid sialography (presence of diffuse punctate sialectasia)
|
|
3. Salivary scintigraphy (delayed uptake, reduced concentration and/or decreased excretion of tracer)
|
|
VI. Presence of serum autoantibodies
|
|
1. Antibodies to Ro(SSA) or La(SSB) antigens or both
|
The histological findings of the labial salivary glands that have been given diagnostic significance are characterised by focal, periductal infiltration of lymphocytes, comprising about 80 % T lymphocytes and 20 % B lymphocytes [18, 19] (Fig. 2.2). The lymphocytic infiltrates may in severe cases replace the acinar tissue. The degree of lymphocytic infiltration is evaluated semi-quantitatively by means of a focus scoring system in which a focus is defined as an aggregate of more than 50 lymphocytes per 4 mm2 of glandular tissue [18]. A focus score is derived by calculating the number of foci per 4 mm2 of the total salivary gland tissue in the specimen [18]. A focus score ≥1 is considered consistent with the diagnosis of SS, provided that other criteria are fulfilled [16, 17].
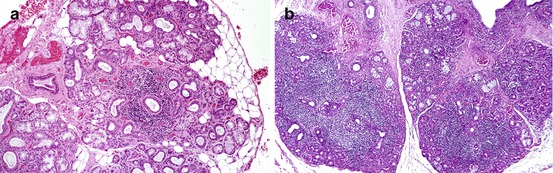
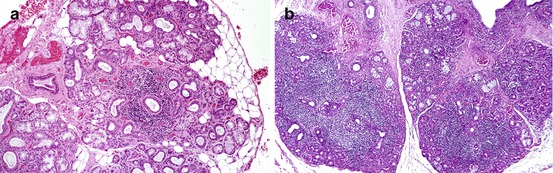
Fig. 2.2
Labial salivary gland specimens from patients with Sjögren’s syndrome. (a) Presence of focal periductal lymphocytic infiltrates. Note the normal-appearing acinar cells adjacent to the infiltrate. (b) Confluent foci of lymphocytes in labial salivary gland tissue
However, focal lymphocytic infiltrates in labial salivary glands are not specific for SS, but may be seen in other disorders such as type 1 diabetes mellitus [20, 21], myasthenia gravis [22], primary biliary cirrhosis [23] and SOX syndrome [24]. Acute and chronic graft-versus-host disease [25], HIV infection [26], leukaemia or lymphoid malignancies [27] and sarcoidosis [28] display symptoms and salivary gland histopathology that resembles SS, and they are also among the exclusion criteria in the American-European Consensus Classification Criteria for SS [16].
The impaired salivary gland function and xerostomia are considered to be consequences of progressive lymphocyte-mediated destruction of the gland tissue [29, 30]. However, the extent of focal lymphocytic infiltration in labial salivary glands is not always associated with the functional capacity of the salivary glands [31, 32]. Thus, some patients with markedly diminished salivary secretion may lack significant focal lymphocytic infiltration in their labial salivary glands indicating an earlier involvement of the major salivary glands than of the minor ones. On the other hand, a recent study indicates that the diagnostic value of labial and parotid biopsies is comparable, and the advantage of taking a parotid biopsy is that it allows comparison of flow rate with histopathological findings from the same gland [33].
It has been suggested that the exocrine gland hypofunction is not merely a result of immune-mediated inflammation, but could be the result of a neurogenic, autonomic dysfunction. It has been shown that stimulation of labial salivary gland cells of isolated patients with primary SS produces an almost identical rise in the intracellular calcium concentration as that of healthy controls, which indicate that patients with SS possess functional receptor systems on their salivary gland cells, despite severely impaired salivary flow [34]. Along this it has been reported that the M3 muscarinic receptors are up-regulated in labial salivary gland acinar cells of patients with primary SS [35] and that these cells have a lowered sensitivity to acetylcholine [36]. These findings suggest that the receptors on the salivary gland cell membranes are not activated either due to inactivation or increased breakdown of the neurotransmitters (most likely acetylcholine) in the synaptic cleft or inhibition of the receptor systems by autoantibodies or cytokines or defect in the intracellular second messenger systems required for stimulus-secretion coupling in acinar cells [12, 34]. Experimental studies in animals suggest that SS-autoantibodies and cytokines play a role in the pathogenesis of exocrine hypofunction by interacting with the muscarinic receptors [37, 38] and that antibodies inhibit the function of the salivary and lacrimal glands [39, 40]. The potential involvement of autoantibodies in SS is further substantiated by the demonstration of Ro/SSA and La/SSB autoantibody-producing cells in labial salivary glands of patients with SS having circulating serum autoantibodies [41]. In addition, interaction of the salivary gland cells with infiltrating lymphocytes seems to lead to increased secretion of cytokines such as IL-6 and TNF-α than can interfere with the binding of neurotransmitters to the receptor system and thereby contribute to salivary gland dysfunction in SS. Moreover, it has recently been shown that autonomic symptoms are common in SS and are associated with the disease activity and symptom burden [42].
Other salivary measures that have been used diagnostically include sialometry with measurement of unstimulated whole saliva flow rate. It has been reported that in primary SS patients with the lowest unstimulated whole salivary flow rates, i.e. <0.05 ml/min, the sensation of oral dryness had the most significant negative impact on general health. These patients were also more severely affected by non-exocrine disease involvement and serological hyperactivity and had more extensive focal lymphocytic infiltrates than patients with flow rates >0.05 ml/min [43]. Measurement of the paraffin chewing-stimulated whole saliva flow rate with a pathological cut-off value of ≤3.5 ml/5 min has a relatively low diagnostic sensitivity (66 %) and specificity (56 %) and is not included in the classification criteria [16]. On the other hand, it provides information regarding the residual secretory capacity of the salivary glands and is useful in monitoring disease progression and efficacy of therapeutic intervention. Selective measurement of the parotid, submandibular and sublingual and the minor salivary gland flow provides important information concerning the function of each of these glands and the composition of the saliva that is produced in these glands, but are not included in the classification criteria. Nevertheless, measurements from these glands indicate that mucous glands/acini are affected earlier than the serous ones [44].
Sialochemical analyses have demonstrated elevated concentrations of sodium and chloride in whole saliva and parotid and submandibular/sublingual saliva despite markedly diminished flow rates, which indicate an impairment of ductal reabsorption of sodium and chloride [44, 45].
Cytokines are assumed to play an essential role in the pathogenesis and B-cell development in SS. It has been reported that serum levels of members of the tumour necrosis factor (TNF) superfamily and levels of the B-cell-activating factor (BAFF) are increased in SS compared to controls and are found correlated with the focal lymphocytic infiltrates in the labial salivary glands [46, 47]. More recent analyses of salivary changes in SS using proteomics, genomics and systems biology assays have opened new possibilities for easier and earlier detection of SS as well as for monitoring the effects occurring in salivary gland physiology induced by treatment with biological agents [48, 49].
Intermittent or persistent enlargement of the salivary glands, particularly the parotid glands, occurs in 20–30 % of patients with SS [50]. It may be unilateral or bilateral. The swelling is usually related to benign lymphoepithelial lesions in the gland tissue. A persistent, unilateral salivary gland enlargement should give suspicion of lymphoma development, since patients with SS have an increased risk of developing non-Hodgkin’s lymphomas, typically the mucosa-associated lymphoid tissue (MALT) type that is about 18 times greater than in the general population [51]. Risk factors for the development of lymphoma include low complement C4 levels, presence of cryoglobulins and palpable purpura [52].
Rheumatoid Arthritis
Rheumatoid arthritis (RA) is a chronic systemic inflammatory disease which affects multiple joints of the body. The inflammatory process primarily affects the lining of the joints (synovial membrane), but can also affect other organs. The inflamed synovium leads to erosions of the cartilage and bone, which may result in joint deformity and disability. It affects 0.5–1.0 % of the population with a female to male ratio of 3:1 [53]. The onset of RA is usually 25–45 years of age, but it may occur in all age groups. The aetiology is unknown, but probably involves interplay between genetic and environmental factors (smoking, viral infections, vitamin D deficiency) that triggers a specific autoimmune response. RA primarily affects the small joints in the hands, wrists and feet. It may also in rare cases affect the temporomandibular joint. The symptoms include malaise, fatigue, weakness, muscle soreness, fever and weight loss which often precede the symptoms of the joints (pain, stiffness, redness and swelling). RA is classified according to the 2010 American College of Rheumatology (ACR) and European League Against Rheumatism (EULAR) classification criteria for rheumatoid arthritis.
A study of 636 patients with RA found that 50 % had symptoms of dry mouth and 17 % diminished unstimulated whole saliva flow rates [54]. It has also been shown that patients with RA have significantly lower saliva secretion from the submandibular gland compared to healthy controls, while the parotid saliva flow rate was in the normal range [55]. The concentrations of acidic proline-rich proteins and statherin in saliva from the submandibular gland were lower in the RA patients with xerostomia than in RA patients without xerostomia and healthy controls [55]. Other studies have also reported an increased frequency of xerostomia and hyposalivation in RA [56–58]. Enlargement of the major salivary glands is relatively seldom, and the risk of lymphoma is low. On the other hand, the labial salivary glands may display inflammatory changes like those seen in patients with SS [59, 60]. About 30 % of patients with RA also have SS (secondary SS), but xerostomia and the salivary hypofunction and histopathology may be present, independent of SS [61, 62].
Systemic Lupus Erythematosus
Systemic lupus erythematosus (SLE) is a chronic, autoimmune, inflammatory disease which affects the joints, skin, kidneys, membranes such as the pleura and pericardium, central nervous system and blood-forming system. The overall prevalence is approx. 50 per 100,000. The onset of SLE is usually in the age of 20–30 years, and the female to male ratio is 10:1. Apart from symptoms like fatigue, weight loss and intermittent fever, SLE is characterised by a facial exanthema (butterfly-like rash), photophobia, vasculitis, hair loss, arthritis, Raynaud’s phenomenon, pleuritis, pericarditis, glomerulonephritis, seizure and psychosis. It has been reported that 75 % of patients with SLE have oral symptoms including mucosal soreness and xerostomia [63]. It has also been shown that the unstimulated whole saliva flow rate in some cases is decreased and that the concentration of statherin in saliva from the parotid gland is lower, whereas the concentration of acidic proline-rich proteins from parotid and submandibular gland saliva is higher than in controls [64]. The stimulated whole saliva flow rate has also been found decreased in SLE in addition to increased salivary concentrations of sodium, calcium, protein and carbohydrates and decreased concentration of phosphate [65]. About 30 % of patients with SLE also have SS [66]. Inflammatory changes have been demonstrated in labial salivary glands in 49 % of patients with SLE of whom 25 % had SS [67].
Scleroderma
Scleroderma is a chronic disease characterised by excessive deposits of collagen especially in the skin, but also in other organs. The generalised type of the disease is designated systemic sclerosis, which can be lethal due to damage to the heart, kidneys or lungs. It is four times more common in women than in men. Symptoms predominantly occur at the age of 40. The characteristic disease manifestations include fibrotic changes of the skin of the fingers, hands, arms and face, sclerodactyly (localised thickening and tightness of the skin of the fingers or toes), telangiectasia, Raynaud’s phenomenon, oesophageal changes, microstomia, arthralgia, myalgia, lung fibrosis, nephropathy and hypertension. SS presents in approx. 20 % of the patients. It has been found that up to 70 % of the patients with scleroderma complain of xerostomia, and about 50 % display diminished whole saliva flow rates. A large variety of inflammatory changes including glandular fibrosis may be seen in the labial salivary glands [68, 69].
Mixed Connective Tissue Disease
Mixed connective tissue disease (MCTD) is a chronic disease characterised by swollen fingers, Raynaud’s phenomenon and non-erosive polyarthritis. MCTD has overlapping features of SLE, scleroderma and polymyositis, and consequently the diagnosis is often delayed. MCTD mostly affects women (90 %), and the onset is often at the age of 30. Xerostomia and salivary hypofunction as well as histopathological changes in terms of focal lymphocytic infiltrates are common conditions in MCTD [70].
Sarcoidosis
Sarcoidosis is a chronic granulomatous disease of unknown aetiology. It is usually seen in the age of 20–40 years and affects women more often than men. The prevalence is about 10:100,000. The tissue of any organ may be affected by the progressive non-caseating granulomatous inflammation, but the lungs, lymph nodes, skin, eyes and salivary glands are most commonly affected. Sarcoidosis may be asymptomatic and may resolve spontaneously within 2 years [71]. However, the symptoms and clinical signs including enlargement of the major salivary glands, symptoms of oral and ocular dryness and salivary hypofunction may resemble those of SS [72]. Histopathologically, the salivary gland tissue is characterised by the presence of epithelioid cell granulomas and not focal lymphocytic infiltration. Sarcoidosis can lead to loss of acinar cell which may explain the reduction in salivary flow seen in some of the patients [73].
Chronic Inflammatory Bowel Diseases
Crohn’s Disease
Crohn’s disease (CD) is a chronic, inflammatory, granulomatous disease which mainly affects the lowest portion of the small intestine known as the terminal ileum, but it may affect any part of the gastrointestinal tract, from the mouth to the anus. The cause is unknown. The inflammation often leads to erosions, ulcers, intestinal obstruction and formation of fistulas and abscesses. The onset of CD most commonly occurs between ages of 15 and 30. Symptoms include chronic diarrhoea, abdominal pain, fever, weight loss, arthritis and ocular infections. More than 30 % of children with CD display mucosal tags, lip swelling, gingivitis, aphthous ulcerations and pyostomatitis vegetans. Also the salivary gland tissue may display non-caseating granulomatous inflammation [74]. About 30 % of patients with CD complain of xerostomia, but whole saliva flow rates and buffer capacity appear to be unaffected [75]. In addition there appear to be no changes in salivary levels of antimicrobial proteins [75].
Ulcerative Colitis
Ulcerative colitis (UC) is a chronic inflammation of the large intestine (colon). The inflammation affects the mucosa and submucosa, leading to ulcers. The symptoms include abdominal pain, diarrhoea, rectal bleeding, painful spasms, fever, fatigue, arthritis and inflammation of the eyes. The cause of UC remains elusive. The onset of UC usually occurs between the ages of 15 and 30. It has been shown that the levels of IgA and IgG in parotid and whole saliva are elevated compared to healthy controls [76]. Salivary levels of nitric oxide and transforming growth factor-beta are also elevated, although not found correlated to the severity of UC [77].
Coeliac Disease
Coeliac disease is an autoimmune disease with small intestine (duodenum and jejunum) inflammation caused by intolerance to gluten, which is found in wheat, oats, barley and rye. Ingestion of gluten is assumed to initiate an abnormal activation of the immune system leading to inflammation in genetically predisposed persons. Symptoms include diarrhoea, dyspepsia, abdominal pain, weight loss, fatigue, anaemia, infertility, depression, osteoporosis, muscle weakness and neuropathy. Oral symptoms include aphthous ulcers, sore tongue, glossitis and stomatitis. Coeliac disease is also related to an increased frequency of dental enamel defects. The mean age of diagnosis is 40 years, but it can occur at any age. It has been shown that patients following a strict gluten-free diet have lower levels of amylase, IgA and IgM in stimulated whole saliva than healthy controls [78]. The whole and parotid saliva flow rates appear to be unaffected. As expected, oral symptoms such as itching and burning mouth, dry mouth and altered taste sensations as well as history of RAS were more prevalent among the patients than the healthy controls, and these results support previous observations [79].
Autoimmune Liver Diseases
In chronic autoimmune inflammatory liver diseases, the hepatocytes, small bile ducts or the entire biliary system are target for an immune-mediated attack. The cause is unknown. The most prevalent of them include autoimmune hepatitis (AIH), primary biliary cirrhosis (PBC) and primary sclerosing cholangitis (PSC). AIH and PBC are most often seen in young women, while PSC mainly affects young men, of whom 75 % also have an inflammatory bowel disease. The symptoms include fatigue, fever, jaundice, polymyalgia, arthralgia and symptoms of progressive hepatic dysfunction. Autoimmune liver diseases often present in association with other autoimmune diseases like SS, RA, type 1 diabetes, autoimmune thyroiditis and ulcerative colitis. Both xerostomia and decreased salivary flow have been reported in autoimmune liver diseases [80]. About 90 % of PBC patients have focal lymphocytic infiltrates in their labial salivary glands [81]. Antimitochondrial autoantibodies to 2-oxo-acid dehydrogenase enzymes have been detected in saliva from patients with PBC suggesting that the salivary glands may participate in the pathogenesis [82, 83].
Amyloidosis
Amyloidosis covers various conditions in which amyloid, an abnormal protein polysaccharide substance with starchlike characteristics, is deposited in tissues and organs and thereby affects their function. Primary amyloidosis occurs independently of other diseases and often affects the skin, tongue, thyroid gland, intestines, liver, heart, lung, spleen and kidneys. Secondary amyloidosis is the most prevalent type, and it usually occurs with other chronic diseases such as rheumatoid arthritis, Crohn’s disease, multiple myeloma, osteomyelitis or tuberculosis, and it often affects the vascular system, lymph nodes, kidneys, liver and spleen. Disease manifestations include cardiomyopathy, nephropathy, purpura, neuropathy, carpal tunnel syndrome, arthritis, bursitis, macroglossia, diarrhoea, constipation and malabsorption. Amyloidosis is typically diagnosed at the age of 40–60 years. Most patients are men. Salivary hypofunction and changes in saliva composition have been demonstrated in patients with familial amyloidotic polyneuropathy [84]. Labial salivary gland biopsy is a highly sensitive method for the diagnosis of primary and secondary amyloidosis [85].
Endocrine Diseases
Diabetes Mellitus
The term diabetes mellitus (DM) refers to a group of metabolic diseases characterised by hyperglycaemia, which develops as a result of insufficient insulin secretion and/or reduced insulin sensitivity. The two most prominent forms are type 1 and type 2 diabetes. Type 1 diabetes is characterised by a progressive immune-mediated destruction of the insulin-producing β-cells in the pancreas. Exogenous supply of insulin is vitally necessary, and if left untreated, it will lead to diabetic coma and death. Type 1 diabetes mainly affects children and adolescents, but it may occur at any age. The initial classical symptoms include fatigue, weakness, weight loss, irritability, polydipsia, polyphagia, polyuria and pruritus. Type 2 diabetes is caused by a combination of insufficient insulin secretion in the pancreatic β-cells and insulin resistance in mainly the skeletal muscles and hepatic cells. Type 2 diabetes typically develops in middle-aged and older people. It is well known that both type 1 and type 2 diabetes are associated with an increased susceptibility to periodontitis and fungal infections. However, xerostomia and salivary hypofunction also appear to be prominent conditions, particularly in inadequately controlled diabetics. It has been shown that 16 % of patients with type 1 with a disease duration of 10 years have symptoms of dry mouth [86] and 54 % of type 2 diabetics with similar duration [87]. The difference in prevalence can be explained by the fact that type 2 diabetics often are older, display more late-diabetic complications, have other medical diseases and take more medications that may cause hyposalivation and xerostomia than type 1 diabetics [88]. In both type 1 and type 2 diabetes, xerostomia has been found related to diminished unstimulated and stimulated whole saliva flow [89–94]. However, other studies found no differences between diabetic patients and healthy controls [88, 95]. Saliva composition in terms of electrolytes, pH, buffer capacity, antimicrobial proteins and total protein has also been studied, but the results are conflicting [for review 96]. Dehydration, occurring as the result of prolonged hyperglycaemia and consequently polyuria, is considered an important cause of xerostomia and salivary gland hypofunction in diabetics [92]. However, structural changes have also been observed in the salivary glands. Thus, 10–25 % of type 1 or type 2 diabetics may develop sialosis, a bilateral asymptomatic enlargement of the major salivary glands, particularly the parotid glands [97–100]. The salivary gland tissue of these enlarged glands is characterised by enlargement of acinar cells, reduction in the acinar tissue, fatty infiltration, fibrosis and no signs of inflammation [99]. It is likely that the neuropathy and microangiopathy associated with diabetes affect the autonomic innervation and microcirculation of the glandular tissue and thereby contribute to salivary hypofunction. Lymphocytic infiltrates have been found in labial salivary glands of children with type 1 diabetes [20], indicating that the salivary gland tissue may be a target for the same autoimmune process as the pancreas.
Thyroiditis
Thyroiditis is a group of diseases that cause inflammation in the thyroid gland and destruction of the thyroid cells. Some of the most common types include Hashimoto’s thyroiditis, postpartum thyroiditis, acute and subacute thyroiditis, drug-induced thyroiditis and radiation-induced thyroiditis. Hashimoto’s thyroiditis, an autoimmune inflammatory disorder, is the most prevalent cause of hypothyroidism, i.e. reduced activity of the thyroid gland. Diseases causing thyroiditis occur three to five times more often in women than in men. The average age of onset is between 30 and 50 years of age. The symptoms are related to thyroid gland hypofunction and include fatigue, weight gain, dry skin, myalgia, constipation and depression. Thyroiditis is common in SS (30–60 %) [101], but autoimmune thyroiditis itself has been found associated with xerostomia (30 %) and inflammatory changes in the salivary glands [102]. Moreover, it has been shown that both unstimulated and stimulated salivary flow are decreased in patients with autoimmune thyroiditis and xerostomia [103].
Neurological Disorders
CNS Trauma
A number of head and brain trauma including, among others, craniofacial fractures, neural disruption by surgical trauma, cerebrovascular accidents including stroke, cerebral ischaemia or haemorrhage and brain stem injury may result in sequelae comprising xerostomia and salivary dysfunction.
Cerebral Palsy
Cerebral palsy syndromes occur in 0.1–0.2 % of children. The prevalence is higher in babies born prematurely. The term covers a group of conditions affecting body movement, balance and posture caused by abnormal development or damage of the part(s) of the brain that controls muscle tone and motor activity. Thus, this CNS damage is characterised by lack of muscle coordination when performing voluntary movements (ataxia), and also stiff muscles and exaggerated reflexes (spasticity) are common. It has been shown that patients with cerebral palsy have diminished whole saliva flow rates and changes in the composition of saliva including increased total protein concentration, decreased amylase and peroxidase activity, decreased sodium and increased potassium concentrations and impaired buffer capacity [104, 105]. Dysphagia and sialorrhoea are common conditions in cerebral palsy. Drooling is often related to swallowing difficulties rather than hypersialorrhoea.
Bell’s Palsy
Bell’s palsy is an idiopathic unilateral facial nerve paralysis. The condition usually has a rapid onset of partial or total facial paralysis. It is generally self-limiting, and in about 70 % of the patients, there is a spontaneous recovery within weeks or few months. However, in some cases it persists, and in rare cases (<1 %) it occurs bilaterally causing total facial paralysis. Several conditions are associated with facial paralysis including pregnancy, diabetes, autoimmune diseases like SS, ear infections and herpes simplex virus infection. The underlying mechanism is assumed to involve swelling and thereby pressure on the facial nerve in the narrow bone canal it passes through in the temporal bone. The facial nerve comprises parasympathetic nerve fibres that supply the salivary glands and travel with the facial nerve, and consequently, Bell’s palsy is characterised by salivary gland hypofunction due to compromised innervation of the gland. Impaired sensation of taste is also common.
Parkinson’s Disease
Parkinson’s disease (PD) is a progressive neurodegenerative cerebral disease of unknown aetiology. It is predominantly diagnosed in persons above 50 years of age.
Degeneration of dopamine neurons results in motor dysfunction, and the four cardinal features of PD are tremor, rigidity, bradykinesia and postural instability and gait disorder. It has been reported that unstimulated and stimulated whole saliva flow rates are reduced in untreated patients with PD indicating that salivary hypofunction is an early manifestation of PD and also a sign of autonomic dysfunction [106]. Furthermore, it has been shown that the salivary concentrations of amylase, sodium and chloride are increased [107]. Xerostomia is also a common symptom in PD, increasing with the progression of the disease. This can be ascribed to the adverse effects of the medication, especially anticholinergic agents, taken by PD patients. However, selective administration of levodopa has been shown to increase saliva flow rates [107]. Drooling and dysphagia are prevalent conditions in PD. Drooling is assumed to be related to reduced swallowing activity rather than hypersialorrhoea.
Alzheimer’s Disease
Alzheimer’s disease (AD) is a progressive neurodegenerative disorder and the most common cause of dementia among elderly people. It is mostly diagnosed in persons above the age of 60. Dementia is characterised by loss of cognitive functioning like memory, reasoning and judgement, as well as loss of behavioural abilities that affect the person’s daily life and activities. It has been shown that untreated patients with AD have salivary hypofunction [108] which may be related to an autonomic dysfunction. Patients with AD are often treated with “xerogenic” medication that can further aggravate salivary gland hypofunction leading to further impairment of the oral health.
Burning Mouth Syndrome
Burning mouth syndrome (BMS) is an orofacial pain condition of unknown aetiology, characterised by a persistent burning sensation in a clinically normal-appearing oral mucosa. There is increasing evidence supporting that BMS is a form of neuropathic pain condition. The average age of onset is usually 50 years. Xerostomia is a common complaint in patients with BMS (30–70 %), but overall both whole and parotid saliva flow rates are within the normal range [109, 110]. Results are conflicting with regard to changes in saliva composition [110]. It has been shown that the salivary concentrations of chloride, phosphate and potassium are elevated [111]. Total protein concentrations appear to be reduced in patients with BMS [111, 112] and also the expression of low molecular weight proteins [111]. A study, comparing the expression levels of MUC1 and Toll-like receptor-2 between patients with BMS, patients with oral lichen planus and healthy women, showed increases in MUC1 transcripts in BMS patients, indicating a role of salivary mucins in BMS [113].
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


