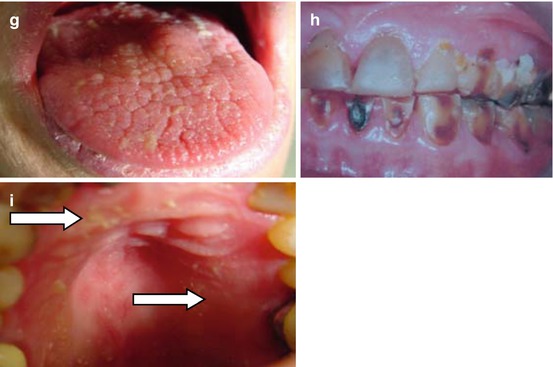
Fig. 8.1
Illustrations of some of the clinical features of dry mouth (a–i). (a) Mirror sticks to buccal mucosa, (b) mirror sticks to the tongue, (c) frothing of saliva (arrows), (d) no saliva pooling in the floor of the mouth, (e) loss of normal gingival architecture, (f) glassy appearance of mucosa, especially palate, (g) fissured or lobulated tongue, (h) active cervical caries due to oral dryness and (i) debris on the palate (arrows)
5.
Tongue shows loss of papillae
Although the scoring system reflects an approximate severity scale, each feature scores one point, and the total is determined. A high total score indicates increased severity of oral dryness. A specially designed form with illustrations of dry mouth features can be used for scoring oral dryness for each patient. The examiner scores the features he/she observes in the patient’s mouth and thus derived a COD score of between 0 and 10 (Fig. 8.2).
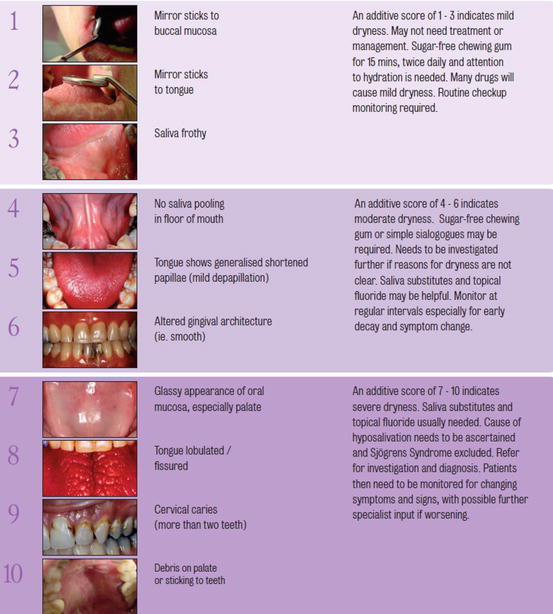
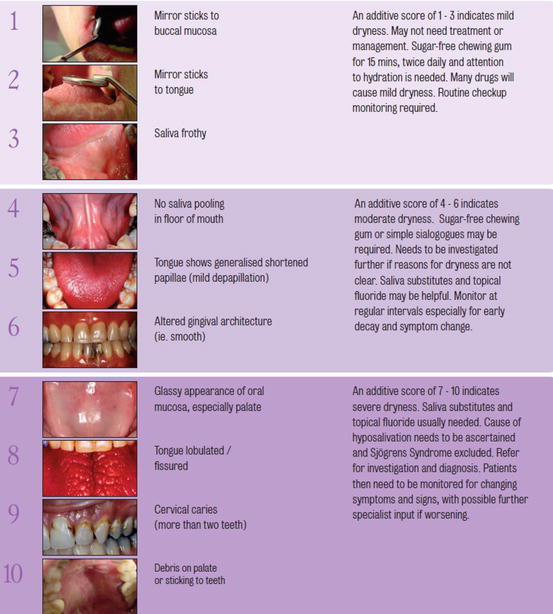
Fig. 8.2
Clinical oral dryness scale to derive CODS assessed as mild, moderate or severe (http://www.dentalhealth.org/uploads/download/resourcefiles/download_68_1_The%20Challacombe%20Scale.pdf)
Instructions for assessment of mucosal dryness and COD score:
1.
Place the mirror head against the buccal mucosa for 2 s and gently move it away. Observe whether the mucosa pulls away with the mirror.
2.
Place the mirror head against the anterior dorsum of the tongue for 2 s and gently move it away. Observe whether the tongue mucosa pulls away with the mirror.
3.
Look round the mouth and observe if saliva is frothy in any areas. This can occur in the sulci as well as the floor of the mouth.
4.
Saliva normally pools in the floor of the mouth. Observe if any saliva can be seen. Dryness of mucosa normally results in it being light reflective.
5.
The dorsum of the tongue is very sensitive to lubrication and desquamates very consistently. Hyposalivation results initially as generalised shortening of the filiform papillae and then of patchy marginal depapillation (scores 1).
6.
Without adequate lubrication, gingival mucosa shows altered desquamation which is normally reflected as shiny red mucosa and loss of normal architecture such as stippling.
7.
Palatal mucosa responds to lack of adequate lubrication by increased desquamation and loss of normal architecture, becoming smooth and translucent. Observe whether such changes are present.
8.
In severe hyposalivation, the dorsum of the tongue becomes depapillated and then fissured and lobulated (scores a further 1).
9.
Observe if there is any recent cervical caries. This scores only if two or more teeth are involved or have been filled in the last 6 months. Single cavities are not sufficiently related to hyposalivation to be discriminatory.
10.
Debris such as food or desquamated epithelial cells are normally removed from the oral cavity by saliva. Presence of debris on the palate or sticking to teeth indicates loss of such function and scores 1.
Interpretation of the COD Score (Fig. 8.2)
An additive score of 1–3 (Fig. 8.2) indicates mild dryness which may not need treatment. Sugar-free chewing gum chewed for 15–20 min twice a day may be adequate to maintain oral health and diminution of symptoms. Patients should also be advised with regard to the importance of maintaining hydration, especially the elderly.
An additive score of 4–6 (Fig. 8.2) indicates moderate dryness. Sugar-free chewing gum or mild sialogogues may be required. Saliva substitutes and topical fluorides or fluoride toothpaste may be appropriate. If the reason for the dryness is not apparent, then these patients should be further investigated. Monitor at regular intervals to ensure that the symptoms remain unchanged and that caries development is controlled.
An additive score of 7–10 (Fig. 8.2) indicates severe dryness. Saliva substitutes and topical fluorides are usually needed. The cause of the hyposalivation must be determined and Sjögren’s syndrome excluded [14]. This usually requires referral and investigation by a specialist in an oral medicine or rheumatology department. Patients then need to be monitored regularly to ensure maintenance of oral health, for changing symptoms and signs and further specialist advice if appropriate.
Relationship of the CODS with Salivary Flow
In a study comparing hyposalivation subjects with controls [15], a strong correlation between the CODS score and the salivary flow was found (Fig. 8.3). Controls had a mean CODS of 1 and an unstimulated whole saliva flow rate of 0.46 ml/min, whilst xerostomia groups had mean CODS of four or greater (Fig. 8.3a) and an UWM of 0.15 ml/min or less (Fig. 8.3b). There is an inverse relationship between the COD scores and the salivary flow rates.
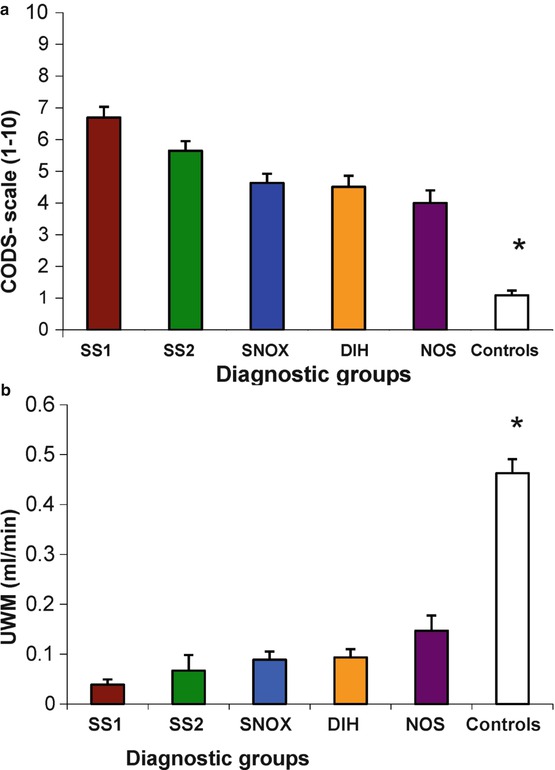
Fig. 8.3
Comparison of clinical oral dryness score (CODS) and salivary flows in different patient groups and controls. (a) Mean CODS ± SEM. (b) Mean unstimulated whole salivary flow rates (ml/min). * = Mean values of were significantly higher in all patient groups compared with controls. SS1 primary Sjögren’s syndrome, SS2 secondary Sjögren’s syndrome, SNOX non-specific sialadenitis, generalised primary nodal osteoarthritis, xerostomia, DIH drug-induced hyposalivation, NOS xerostomia not otherwise specified (From Osailan et al. [7])
Relationship Between CODS and Mucosal Wetness
Mucosal wetness is a term describing the thickness of the mucin layer protecting mucosal surfaces in the oral cavity [17, 18], and methods of assessing this are described elsewhere in this book. In essence there is a layer some 30 μm thick overlying buccal and lip mucosa, with half this thickness on the hard palate and double this thickness on the tongue (Fig. 8.4). When groups of patients are given CODS scores indicating mild, moderate or severe dryness, this correlates very well with the actual mucosal wetness [18] suggesting that the clinical assessment of dryness can be related directly to other more measureable parameters (Fig. 8.4).
Fig. 8.4
The relationship between CODS and wetness of oral mucosal surfaces in patients and controls. The xerostomia patients have been divided into three groups (CODS 1–3, 4–6 and 7–10). * = The mucosal wetness of the three patient groups was significantly less (p < 0.05) than the controls for each of the four mucosal surfaces. Key: AHP anterior hard palate, BUC buccal mucosa, AT anterior tongue, LL lower lip (Figure from Osailan et al. [7])
The clinical oral dryness score is thus related both to salivary flow rates and to mucosal wetness. This suggests that the CODS could be used routinely in clinical oral and dental practice to assess and semi-quantify the severity of oral dryness with confidence that it is related to salivary flow and mucin thickness. In addition, although simpler than some other mucosal disease scoring systems [10–12], it should also be as suitable for monitoring longer term of disease in patients and treatment efficacy. In contrast to inflammatory diseases, long-term success with CODS would be maintenance of a low score.
The clinical features of oral dryness that are included in the CODS, for example, glassy oral mucosa, fissured or depapillated tongue and lack of saliva pooling in the floor of the mouth, are recognised as signs of hyposalivation [19]. In the CODS each feature scores 1 point, but the scale represents an approximate hierarchy of features for dry mouth, and the highest CODS tend to be associated with fissured tongue, cervical caries and the presence of food debris that is not cleared from the mouth.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


