Direct Anterior Restorations—Aesthetics and Function
Since their introduction (Bowen 1956), composite restorations have become increasingly more important in the treatment of anterior and posterior teeth. Skillfully placed composite restorations can be superior to indirect restorations as far as their natural appearance is concerned (Buda 1994) and at the same time they can withstand the occlusal forces. The adhesion of the resin to both dentin and enamel makes it possible not only to restore teeth but also to fundamentally change them. Only little tooth substance needs to be removed for composite restorations. The margins can be gap-free, preventing bacterial penetration. Composites belong to the most important materials in cosmetic dentistry (Christensen 1995b). They can restore fractured or decayed anterior teeth cosmetically, they can close diastemas, and they can alter the color of the teeth. A person’s whole appearance can be improved through a combination of bleaching, ceramic veneers, and composite restorations.

236 Possibilities and limitations of direct composite restorations in the anterior region
Left: Lateral incisor, a pegged tooth that was moved into the middle position between a central incisor and a cuspid by means of orthodontics.
Right: The central incisor, the lateral incisor, and the cuspid are rebuilt with direct composite bonding. An aesthetic result is achieved.
Indications for Composite Restorations
Patient’s Age
To restrict the loss of tooth substance, one should prepare as conservatively as possible. The younger the patient is, the more important it is to minimize the loss of enamel and dentin. Direct composite restorations are the most conservative material available in present-day aesthetic dentistry. The age of the patient should not affect the use of composites.
Selecting Which Teeth to Restore
Small defects can be treated with small fillings, particularly if the tooth is intact and is aesthetically acceptable. As far as larger defects or poor aesthetics of the remaining tooth substance are concerned, an indirect ceramic restoration or an all-ceramic crown should be considered.
Goals
The opinions of both patient and dentist should be considered when drawing up the treatment plan. Have both decided on an aesthetic goal, or is the objective only to restore the defect? The higher the aesthetic goal, the more extensive the restorations may have to be.

237 Selecting composites
The age of the patient plays a role when selecting a suitable restorative material. Since all restorations must be renewed after a certain time, younger patients should be treated using a tooth conservative restoration form. This can be a direct composite restoration. Direct composite bonding covers up this front tooth of a 17-year-old patient with white color inclusions.
Right: Result three years after direct composite bonding.

238 Composite restorations—a tooth conservative method
Small defects should be treated very conservatively, especially if the surrounding tooth structure is caries inactive and aesthetically acceptable. Direct composite restorations are ideal for these conditions.
Occlusal Forces
Composites do not resist high occlusal forces. If the natural tooth substance has been destroyed due to occlusal force, one should use conventional restorations, such as ceramics or metal. Cohesive and adhesive fractures can appear with direct composites. The risk of fracture can be reduced if the enamel area is increased in an attempt to increase the bonding area with the composite. The most stable resin should be used.
Material
The dentist usually chooses the material that fulfills the aesthetic needs, has sufficient occlusal stability, and is easy to process. Hybrid composites are most frequently used because of their strength and surface smoothness. They are available in different shades, opacities, and qualities—from very rigid to fluid. Microfilled composites are chosen primarily when one wants to simulate the appearance of enamel.
Bonding
Many studies show that bonding systems bond to enamel and dentin with sufficient strength. By bonding, cohesive fractures are avoided in the tooth or in the composite restoration. Bonding to enamel is reliable and durable.
Oral Hygiene
All margins must be plaque-free. In vitro tests show a decrease in marginal leaching when the composite is bonded to dentin. Dentin margins need to be observed more closely due to the risk of plaque accumulation and caries. Instructions regarding oral hygiene are crucial, particularly when composites are used.
The Ability of the Dentist
Aesthetic or cosmetic dental treatments are the plastic surgery of dentistry. The dentist’s understanding of shape, proportion, color, material, and the psychological effect of aesthetic dentistry are essential for diagnosis and treatment. The dentist must model the appearance of the teeth so that it corresponds to the physical and psychological requirements of the patient.
Economy
Direct composites are more advantageous than indirect fillings. Patients often choose composites to avoid high expenses, even if they are informed about the inferior durability in comparison to other restoration types.
Choosing a Composite
Hybrid composites are chosen because of their high stability and hardness. Microfilled composites are easier to polish. However, they are more susceptible to fractures and the so-called sandwich technique is often used to cover the hybrid composite. By doing so, the stability of the hybrid composite can be combined with the ename appearance of the surface of the microfilled composite. Microfilled composites are also used for fillings with little stress and on facial surfaces where an enamel look and high polish are important. The differences He in the shades, the opacity, and the processing. The dentist should choose the composite that gives the best aesthetics and fulfills the functional requirements.

239 Limitation of composite restorations
Loss of the vertical dimension through parafunction. With bruxism and with patients who regularly use high occlusal forces, the use of composites on occlusalincisal regions is contraindicated.
Left: Without the support of a stable reconstruction (gold or ceramics) in the molar region, these anterior teeth cannot be rebuilt.

240 Limitation of composite restorations
All composite restorations must be renewed sooner or later. The patient must know that the lifespan of composite restorations depends on many factors that can impair the appearance and the function: composition of the saliva, bacterial activity in the oral cavity, nutritional habits, occlusal forces, type of tooth cleaning, etc.
Clinical Application of Composites
Placing the Composite
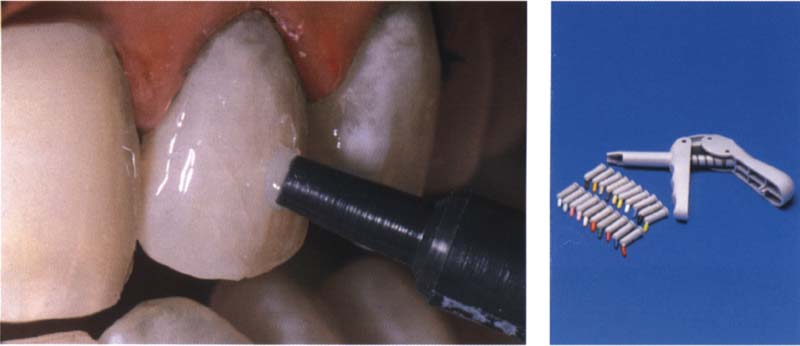
1. Determining Color
The color of the tooth must be decided before it is isolated, while it is still moistened with saliva. Commercial shade guides do not usually show the real tone. The use of specially prepared shade guides, made from the composite used, makes it possible to improve color selection. Teeth appear polychromatic through the deeper layers of dentin covered with translucent enamel. The color at the gingival margin can be distinguished from areas of the middle of the tooth as well as from the proximal and incisal regions.
Selecting and placing the individual color layers and changing opacity requires careful analysis and great skill (Buda 1994). Composites transfer color and light unevenly on enamel and dentin. The irregularities of the natural tooth should be reproduced as close as possible and to achieve this the dentist must place layers of different color tones. Hybrid composites appear like dentin, while microfilled composites imitate the enamel better.

241 Isolation using a rubber dam
A rubber dam is, and remains, the best and most effective isolation technique and should be used with composite restorations as a matter of course. Care must be taken that the teeth do not dehydrate during the bonding procedure.
Right: With molar teeth, isolation with a rubber dam is especially important before bonding. The teeth should be kept moist.
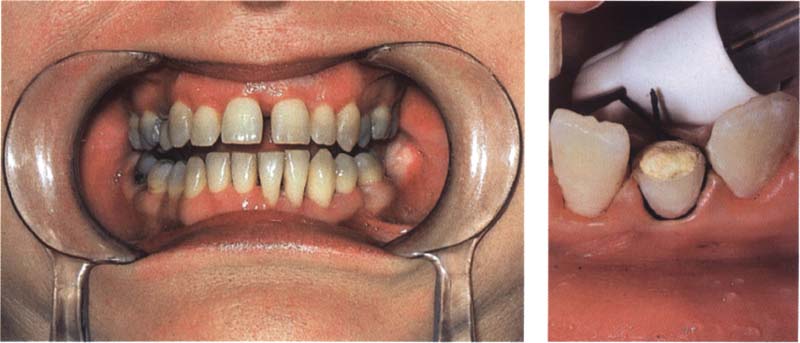
242 Isolation with other aids
If isolation with a rubber dam is not possible one can use cotton rolls, powerful saliva ejectors, and retraction cords. Also a cheek retractor that is normally used for dental photography is sometimes very helpful.
Right: Here, a lower incisor was isolated using a retraction cord.
Several layers of composites or color tones can be placed without losing adhesion or stability, as long as the surface of the polymerizing composite has a moist oxygen-inhibited layer.
2. Field Isolation
Saliva and blood components decrease the bonding ability to the tooth. A rubber dam is the most effective method to avoid contamination with saliva. Drawbacks of this method can be an inferior view and decreased access (Knight et al. 1993). Alternative isolation methods include cheek retractor, retraction cords, and suction, methods that are often sufficiently effective if they are used properly. However, each of these methods must be regarded as compromises in comparison with the absolutely dry field that can be achieved with a rubber dam. The dentist must always guarantee that during all procedures the tooth and the partly finished restoration are free from contaminating saliva.
3. Preparation
4. Adhesion to Enamel and Dentin
As was shown in the chapter on bonding, enamel and dentin are conditioned with phosphoric acid. Both tooth structures are etched and then rinsed with water. The primer and the adhesive are placed on enamel and dentin according to manufacturer’s instructions. The correct procedure is decisive for the quality of the margins and the bonding of the restoration.
Fifth-generation dentin adhesives are suitable for direct composite restorations. The dentist and the assistant should consider the following:
The teeth must be kept moist. Directly before placing the adhesive, open the bottle (the solvent acetone evaporates immediately), place the adhesive on an applicator, close the bottle immediately, briefly dry the tooth, and place the adhesive, wait for 20 seconds (the adhesive must penetrate into all structures and the solvent must evaporate), blow lightly, and polymerize. Always place a second layer.

243 Preparation
Caries is removed with conventional instruments. The best to be used are water-cooled, high torching diamonds, which are used to modify the enamel and to create undercuts and retentions.
Left: Set of coarse diamonds suitable for the preparation of direct composite veneers.
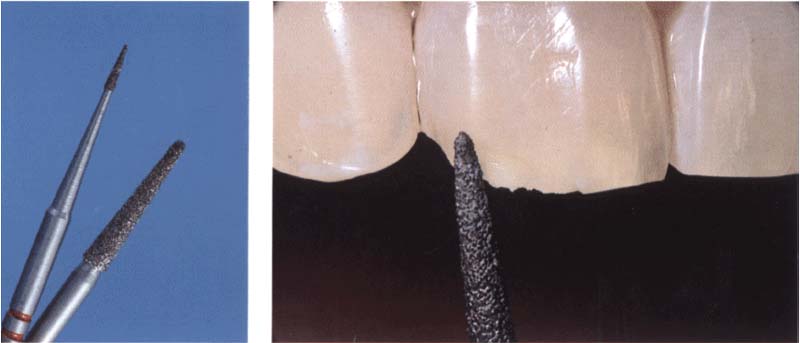
244 Preparing a bevel
Broad bevels should be placed at preparation margins and transitions where the composite meets the enamel.
Left: Diamonds used for preparation of a bevel.
5. Placing the Restoration
Principles of proper composite placement:
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses