Composite Inlays
Direct composite restorations are not always suitable for replacing amalgam. Without doubt it is the restoration of choice in the case of incipient, small carious lesions. However, with bigger defects, when larger parts of the occlusal surface and the interproximal surfaces are involved and need to be replaced, composite inlays and onlays offer clear advantages. The biggest problem with modern posterior composites is their polymerization shrinkage and the stresses it induces around the margins. These stresses can cause debonding, form gaps, increase tooth sensitivity, and lead to progression of the caries process. Therefore, a goal must be to reduce the tensile stresses which arise around the margins during the making of a composite, which is done with a complex, time-consuming layering technique. Today’s resins do not allow polymerization shrinkage to be completely eliminated. The composite inlay should be considered at this point as superior to the direct composite restoration, since the contraction of the inlay takes place extraorally.
296 Composite inlays
Composite inlays can serve as an alternative to amalgam restorations if the defects are large. The cementation technique, among other things, is decisive for the success of these restorations. Composite inlays must be bonded with an adhesive technique.
Advantages and Disadvantages of Composite Inlays
Composite inlays and onlays can be placed to reduce polymerization shrinkage and composite wear. The advantage of this method is that the main part of the composite is cured outside the oral cavity and only a thin resin layer, the resin cement layer, contributes to shrinkage of the restoration in the oral cavity. Advantages of this include a reduced tensile stress level around the margins and reduced risk of debonding, particularly at the tooth-cement interface (Lutz et al. 1991). However, despite reduced tension around the margins between tooth and inlay, a perfect bond is not always formed (Cassin and Pearson 1992; Zuellig-Singer et al. 1992).
Although most posterior composites which are placed nowadays are direct composites, dentists should master the technique of making a posterior composite inlay, since such a technique simplifies many of the curing and trimming stages and will probably increase the chances of success with this type of restoration.
Composite Inlay Systems
All modern small particle/hybrid composites can be used for making composite inlays. A new generation of composites is extremely suitable for this purpose—these materials are Art-Glass, Solidex, and Bellglas.
Methods for making composite inlays:
— The technique for direct composite inlays enables the dentist to prepare inlays directly inside the oral cavity, perform an extraoral polymerization, and place it at the same treatment session.
—Immediate inlay: After the tooth has been prepared, a simple impression (e.g., alginate) is made and poured with a silicone or a quick-setting plaster. The composite is placed and polymerized on this model. It is bonded to the tooth during the same session.
—Laboratory-processed inlay: After a dental impression has been made, the inlays are produced in the dental laboratory and bonded during the second session.
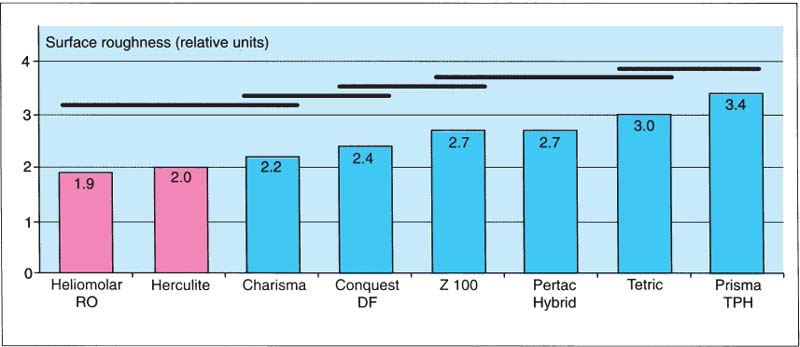
297 Surface roughness of materials used for composite inlays
Any small particle hybrid composite can be used for composite inlays. The surface roughness is a variable that should be considered during selection. The black horizontal lines overlapping two or more bars indicate products that statistically are not significantly different from each other.
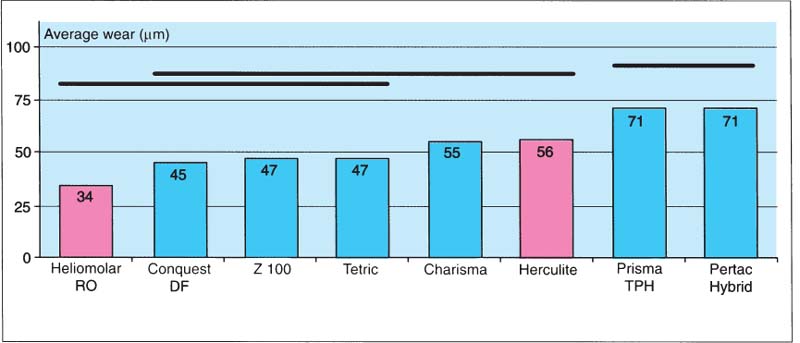
298 Average wear of the same products as in Fig. 297
The wear resistance of the different composites is another criterion to be considered during selection of a suitable inlay material. There is no statistically significant difference between Conquest DF, Z100, Tetric, and Heliomolar RO, which was introduced on the market many years ago.

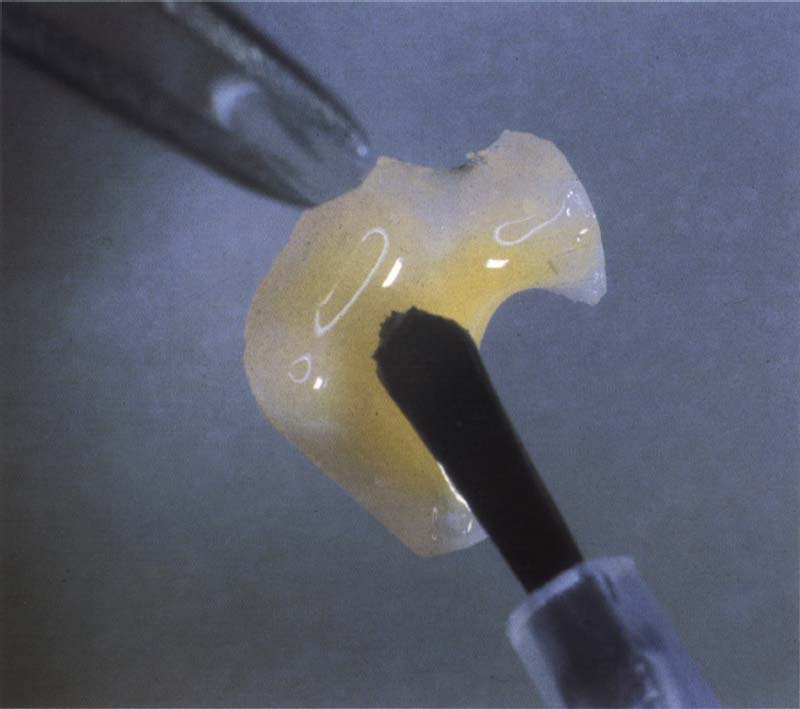
299 New materials and products
In the coming years, many new products, which should not differ significantly in their clinical behavior from ceramic inlay materials, will be marketed as composite inlay material. However, they will be substantially simpler to process. Art-Glass and Solidex are just the beginning.
Diagnostics and Treatment Planning for Composite Inlays and Onlays
A good hygiene phase is important if composite inlays are to be used. The bond site is a weak link in the transition from the tooth to the inlay. The bonding composite is not as filler loaded in this region and is exposed to more severe wear. Such bonding sites have a porous surface and a concavity where plaque can often be seen after the bonding resin has worn. Since this region often is difficult to clean, secondary caries easily originates here. The cervical margin is at particular risk.
Before the treatment, it is necessary to assess the bacterial activity in the oral cavity. If there is a high risk of caries, patients must be informed that secondary caries can originate easily at the bond site of the inlays if they do not clean their teeth perfectly. Patients need to be informed that the margins of the inlay must be checked twice a year after completed treatment. Furthermore, bitewing radiographs should be made at regular intervals.
At the first session the following tasks should be carried out:
The dental hygienist performs most of these tasks. All diagnostic records are available to the dentist at the beginning of the treatment. The situation models are used as counter bite models and to manufacture temporary restorations. It may happen that an inlay was planned originally, but after finished preparation an onlay or a partial crown is necessary. Available situation models then facilitate the provisional care.
Preparation of Composite Inlays and Onlays
The preparation of composite inlays is very similar to that of gold inlays. An essential difference is that no feather edges are prepared and the walls are shaped so that they diverge somewhat. The layer strength with composite inlays is allowed to be 1.5 mm in each direction, while in the case of ceramic inlays it should not be less than 2.0 mm. A blocking restoration is desirable with large defects, otherwise the preparation will become over extended. If maximal conservation of healthy tooth substance is the goal, blocking restoration forms an important part of the preparation.
Making the Blocking Restoration, Materials, and Techniques
It is not necessary to prepare the inner line angle. Nevertheless, refining the preparation with hand instruments leads to straight walls, which leads to better results in the case of impression taking, model and inlay processing, but also cementation and finish/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


