Since the World War II era, innovations in the management of cranio-maxillofacial trauma have continued to evolve. The introduction of rigid internal fixation has transformed the treatment of facial fractures by optimizing primary bone healing, as opposed to secondary bone healing seen with closed techniques. Rigid fixation has significantly improved treatment outcomes of the maxillofacial trauma patient, allowing the surgeon to restore form and function sooner, and with more stable and predictable results.
The treatment of mandible fractures is a central component of facial trauma that the oral and maxillofacial surgeon must be adept at managing. Retrospective studies indicate that mandible fractures are the most common fracture encountered in maxillofacial trauma. These fractures range in complexity from isolated injuries as a result of low-velocity trauma to comminuted or avulsive injuries paired with multisystem injury. Interpersonal violence and motor vehicle accidents are cited as the most frequent causes of mandibular fractures. Different fracture patterns and degrees of severity create wide variability in both the degree of dysfunction and the assortment of complications. Because the mandible is such a unique anatomic structure with a ginglymus (hinge) diarthrodial joint, several different modalities of treatment can be applied with similar success. Gear et al performed a survey of AO/ASIF (Arbeits-gemeinschaft fur Osteosynthesefragen/Association for the Study of Internal Fixation) faculty members regarding their treatment of mandibular angle fractures. Although the “Champy technique” (discussed later) was the most commonly used among the 104 faculty members, it is interesting to note the variability in forms of treatment for just this type of fracture pattern. Despite the diversity of treatment alternatives reported, most options held fast to the same basic principles of fracture management in order to be successful.
The goals of treatment should be as follows:
- •
Early return to function
- •
Anatomic reduction and stabilization of fractures
- •
Establish and preserve the occlusion
- •
Avoidance of infection
- •
Avoidance of malunion or nonunion
An understanding of these goals is paramount in treatment planning. The surgeon must understand the indications and objectives for each type of treatment and he or she then must weigh the risks versus the benefits of the proposed management. At times, the more “aggressive” treatment proves to be the best. The objective of this chapter is to provide the clinician an overview of the advancements made in the treatment and management of mandible fractures.
HISTORICAL OVERVIEW
As you review the historical progression of mandible fracture management, you will appreciate the emphasis on the importance of reduction and immobilization. One of the first descriptions of the mandible fracture was from the Egyptians in 1650 BC. It was described as an incurable process that would result in infection and lead to death of the patient. Hippocrates described the importance of reduction and immobilization with the use of the “bridal wire,” which is still used in practice today by some surgeons for early stabilization.
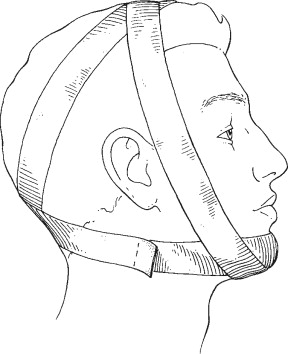
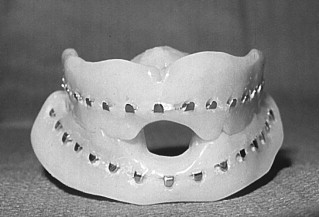
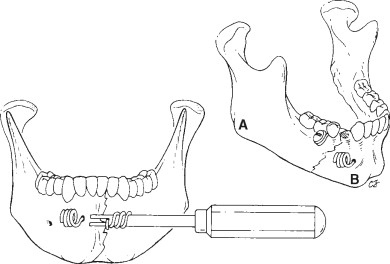
As centuries passed, closed reduction and stabilization techniques were developed. The concept of maxillomandibular fixation (MMF) was then introduced; that is, by keeping the teeth wired together into a stable occlusion, the fracture could be stabilized. Many types of MMF have been described; some examples detail the use of external bandages (e.g., Barton’s bandage), the fabrication of internal splints (e.g., Gunning’s splints), or the use of external frame and pin fixation ( Figures 10-1 , 10-2 , and 10-3 ). Various forms of interdental wiring techniques for fracture fixation have been described, and usually Erich arch bars are used today ( Figure 10-4 ). A more recent permutation of traditional MMF has been the introduction of intermaxillary fixation (IMF) screws, which are self-drilling or self-tapping screws placed in the alveolus between or above the dental roots ( Figure 10-5 ).
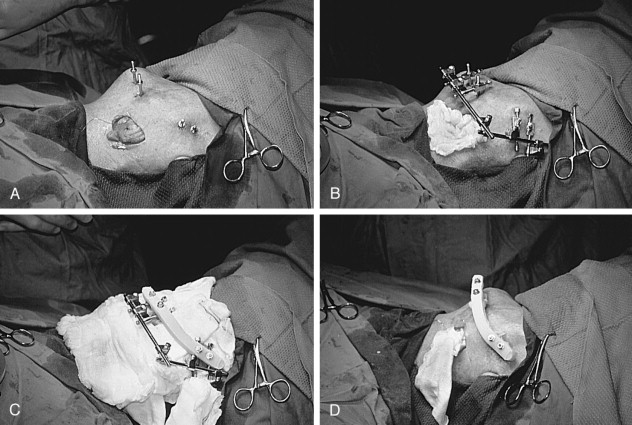


Although the closed techniques were effective, they still had many limitations: function was limited for the duration of treatment, precise bone reduction was not possible, and occasionally bone gaps were present that exceeded the body’s ability to heal. This led to the development of open reduction and internal fixation techniques. Before the antibiotic era, the risk of infection was high from open repair procedures. One of the first descriptions of an open reduction with internal fixation came in 1869 with the “Thomas silver wire” technique ( Figure 10-6 ). The fracture was opened and a transosseous wire was used to help stabilize and reduce the fracture. Other early techniques described the use of rods and wires made of iron, which were later abandoned because these metals began to corrode within the wounds. Limitations of these techniques included the lack of stability across the fracture line, resulting in secondary bone healing.
Recognizing that a stable rigid mode of fixation would optimize primary bone healing and thereby allow early return of function for the patient, transosseous wiring began to be replaced by plate and screw techniques in the 1960s and 1970s. Plate and screw techniques were also being used by AO/ASIF for the treatment of extremity fractures. These were compression plates that used bicortical screws that would compress the fractured edges together. Attempts were made to translate this technique to the treatment of maxillofacial fractures, but it since has fallen out of favor with many surgeons. Muscle actions of the mandible differ significantly from those of the extremity. Compression plates apply compression to areas of the mandible that are already under biomechanical compression.
Advancements in plating techniques have optimized the surgeon’s versatility. This is no longer the era of “a screw is a screw and a plate is a plate.” Many different forms of plating technology are now available to the surgeon: nonlocking plates, threaded locking plates, tapered locking plates, bicortical and monocortical fixation, and rigid and semi-rigid plates. To be proficient in the subspecialty of trauma the surgeon must be educated in each modality’s strengths and limitations in order to strive for excellence in the treatment of each patient.
EPIDEMIOLOGY
There are many causes of mandible fracture, and there is much variability depending upon the population examined. In rural populations, motor vehicle collisions are the more common cause. In contrast, urban patients are often subject to interpersonal violence. However, the following are the more common causes of mandible fractures :
- •
Motor vehicle collisions
- •
Assaults
- •
Industrial injuries
- •
Falls
- •
Sports-related injuries
- •
Ballistic injuries
- •
Pathologic fractures
EPIDEMIOLOGY
There are many causes of mandible fracture, and there is much variability depending upon the population examined. In rural populations, motor vehicle collisions are the more common cause. In contrast, urban patients are often subject to interpersonal violence. However, the following are the more common causes of mandible fractures :
- •
Motor vehicle collisions
- •
Assaults
- •
Industrial injuries
- •
Falls
- •
Sports-related injuries
- •
Ballistic injuries
- •
Pathologic fractures
CLASSIFICATION
Fractures of the mandible can be categorized on the basis of location, pattern, and biomechanics. In addition to understanding the injury, the surgeon must recognize the role of biomechanics in the creation of the injury. It is the release of kinetic energy that results in both hard and soft tissue injury. The energy and the vector of the injury will determine the fracture pattern and location, and this will directly impact how the surgeon manages the injury.
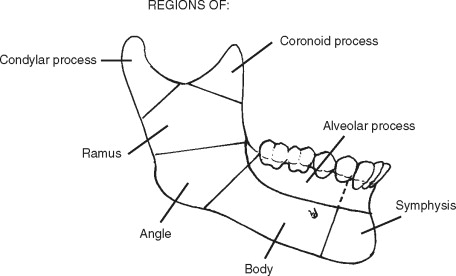
LOCATION
- 1.
Symphysis: Occurring in the midline, between the central incisors.
- 2.
Parasymphysis: Area bound between vertical lines distal to the canines.
- 3.
Body: Area bound from the distal symphysis of the canine to the anterior border of the masseter muscle (distal of the second molar).
- 4.
Angle: Area bound from the anterior border of the masseter (distal of the second molar) to the posterior border of the masseter. Third molars, if present, are typically involved in angle fractures.
- 5.
Ramus: Area from the posterior border of the masseter to the height of the sigmoid notch; the term “subcondylar fracture” is typically within the region of the ramus.
- 6.
Condylar:
-
Intracapsular: A fracture of the condylar head, which is bound by the capsule.
-
Condylar neck : A fracture from the height of the sigmoid notch to the attachment of the capsule. These fractures are further subdivided:
-
Dislocated: The head of the condyle is dislocated from the glenoid fossa.
-
Displaced: The head of the condyle remains in the glenoid fossa, but the neck of the condyle has been pulled out of alignment with the ramus. This can be in any direction, but most commonly is anteromedial because of the pull of the lateral pterygoid muscle.
-
- 7.
Coronoid: The area of the coronoid process superior to the height of the sigmoid notch.
- 8.
Dentoalveolar: A fracture of the alveolar bone and supporting root structure; it does not involve the basal bone of the mandible.
The distribution of fractures has also been examined, with the angle and parasymphyseal regions being most common, followed by condyle fractures. The least common fracture is the coronoid process; these fractures often are associated with a fracture of the zygomatic arch ( Figure 10-7 ).
FRACTURE PATTERNS
- 1.
Open fracture (compound): This type of fracture has communication with the external environment, either through skin or through mucosa, including the periodontal ligament. Any fracture involving a tooth-bearing segment is an open fracture by definition.
- 2.
Closed fracture (simple): This type of fracture has no communication with the external environment.
- 3.
Comminuted: Multiple segments of bone are shattered, crushed, or splintered in this type of fracture.
- 4.
Greenstick: This fracture is incomplete and only involves one cortex.
- 5.
Pathologic: A fracture occurring from pre-existing disease that has structurally weakened the bone is pathologic.
- 6.
Complex (complicated): This can be either a simple or a compound fracture that is associated with significant adjacent soft tissue injury.
- 7.
Multiple: In a multiple fracture, there are two or more fractures within the same bone, but the fractures do not communicate with each other. A mandible fracture will typically have at least two fractures. An analogy typically used is the mandible being like a ring or pretzel; it is very difficult to break in only one place.
- 8.
Atrophic: An atrophic fracture is a spontaneous fracture resulting from mechanical weakening because of atrophy. An atrophic mandible is defined as an edentulous mandible that has 20 mm or less in height.
- 9.
Indirect: This is a fracture that occurs at a site distant from the area of impact (for example, the classic “guardsmen fracture,” having bilateral condylar necks and a symphyseal fracture). The point of impact at the chin creates multiple fractures—a direct symphysis fracture and indirect condylar neck fractures.
-
10. Impacted: A fracture in which segments have “telescoped” upon each other is impacted.
BIOMECHANICS
Mandibular fracture displacement is defined as follows:
- 1.
Favorable (stable): The fracture line and the vector of the muscle pull keep the fracture buttressed and appropriately reduced.
- 2.
Unfavorable (unstable): The fracture line and the vector of the muscle pull cause displacement ( Figure 10-8 ).
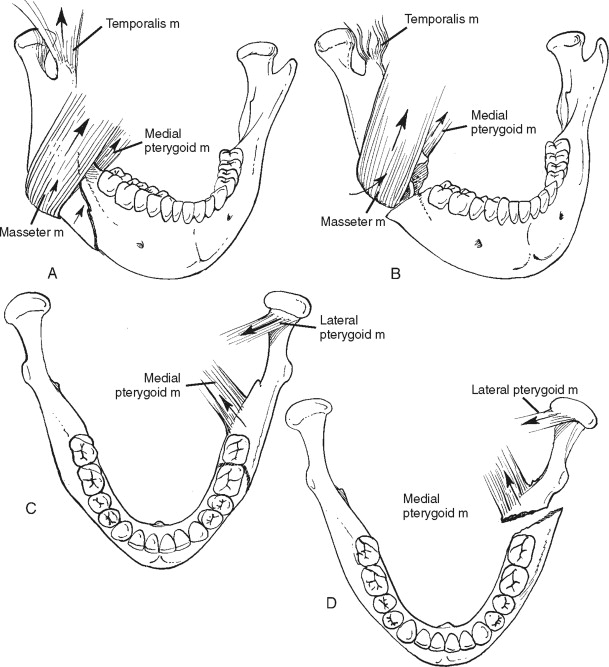
FIGURE 10-8 A, Horizontally favorable fracture. B, Horizontally unfavorable fracture. C, Vertically favorable fracture. D, Vertically unfavorable fracture.
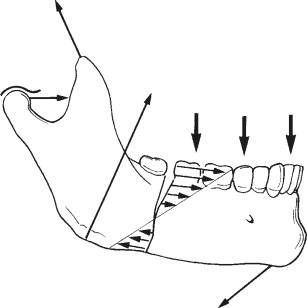
Understanding muscle attachments and the forces imposed upon the mandible will aid the surgeon in the management decisions. A mandible fracture has three forces acting upon it: compression, tension, and torsion ( Figure 10-9 ). These forces vary in magnitude depending upon the location of the fracture. The muscles responsible for the vertical displacement are the masseter, temporalis, and, to a degree, the medial pterygoid. Horizontal displacement can be caused by the lateral and medial pterygoid and torsion by the mylohyoid, digastrics, and geniohyoid. The favorability and unfavorability are described based on the plane of the films obtained; so a “horizontally unfavorable” fracture is displacement noted on an orthopantomogram. Conversely, a “vertically unfavorable” fracture is displacement noted on an anteroposterior film. This can be confusing at times because the vectors of the muscle pull are opposite to the plane of the film. It is probably more important to denote simply whether or not a fracture is favorable or unfavorable in nature. This feature of the fracture significantly impacts the treatment plan. For example, the buttressing effect seen in some favorable fractures will make these more amenable to closed reduction and MMF. In contrast, unfavorable fractures are typically more amenable to open reduction and internal fixation because of lack of buttressing.
DIAGNOSIS
When the patient presents to the trauma resuscitation unit, the trauma team initiates an Advanced Trauma Life Support (ATLS) protocol. The primary survey is completed, with stabilization of the patient including the airway and cervical spine. This is followed by the secondary survey where a general but systematic cranio-maxillofacial exam occurs. Necessary images are obtained based on clinical signs, and appropriate consultants are notified.
PHYSICAL EXAM
After the patient is stabilized and an appropriate history is ascertained, including the mechanism (energy) of injury, a complete head and neck exam should occur. Some of the signs and symptoms of a mandible fracture include the following:
- 1.
Pain: Examination should include a complete head and neck exam with palpation of the mandible along its entire contour, including the temporomandibular joints. The exam should also include intraoral palpation along the alveolus, external oblique ridges, and anterior border of the ramus.
- 2.
Swelling: Upon extraoral (resulting in facial asymmetry) or intraoral examination, one may note vestibular or floor of mouth edema.
- 3.
Paresthesia of the mental distribution
- 4.
Trismus
- 5.
Malocclusion
- 6.
Ecchymosis of vestibule and/or floor of mouth
- 7.
Gingival laceration
- 8.
Mobility of bone segments or teeth
- 9.
Palpable bony steps
-
10. Deviation of the mandible; changes in facial contour or arch form
RADIOGRAPHIC EXAM
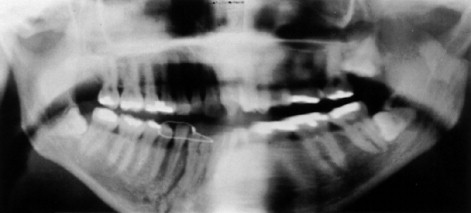
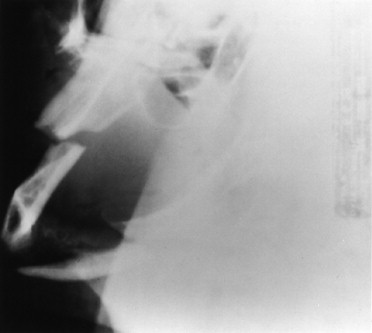
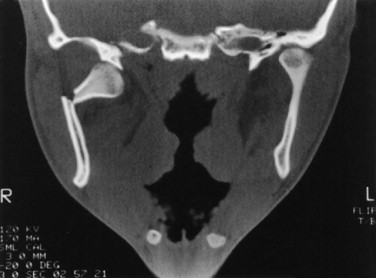
Radiographic imaging is additional objective data that should confirm (or complement) the practitioner’s working diagnosis. The plain film is still the most cost-effective and accurate radiographic modality. When obtaining plain films, two views at right angles must be obtained in order to assess fracture displacement. A “mandible series” consists of the orthopantomogram (or it can be substituted with right and left lateral oblique views), posterior/anterior view, and reverse Towne’s view ( Figures 10-10 through 10-13 ). A reverse Towne’s view will aid in the assessment for a condylar fracture. In many institutions computerized tomographic (CT) scans are readily available and can be viewed in three planes: axial, coronal, and sagittal. Additionally, they now can be reconstructed into three-dimensional images ( Figures 10-14, 10-15, and 10-16 ). CTs are obtained in circumstances in which the patient has suffered multisystem trauma and may need to be scanned for other injuries, or when the patient is unable to be appropriately positioned for conventional radiographs.




OVERVIEW OF BONE HEALING
An understanding of the principles of bone healing is an important factor when determining the technique for fixation as well as the time allotted for the return of function. There are two processes by which a mandible fracture can heal: primary (direct) or secondary (indirect) bone healing. Either process will appropriately heal the mandible to a state that will withstand the biomechanical stress of function and form.
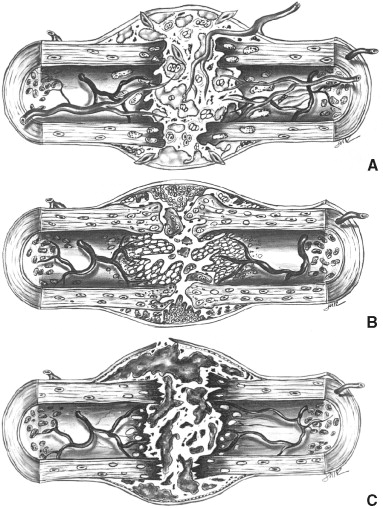
SECONDARY (INDIRECT) BONE HEALING
Secondary bone healing occurs through a process of remodeling and callus formation when the fracture is immobilized without the use of rigid fixation. Bone healing occurs according to the principles of Wolff’s law. Julius Wolff proposed that mechanical stress was responsible for determining the architecture of bone. Remodeling of bone occurs in response to physical stresses (or lack thereof) from the soft tissue envelope and musculature, whereby bone is deposited at sites subjected to stress and is resorbed at sites where there is little stress. In contrast to second intention healing of soft tissue, which will not return the tissue to its pre-injury state (i.e., formation of scar tissue), secondary bone healing will regenerate the injured bone to its pre-injury state. Remodeling of the mandible to a full load-bearing state requires 4 to 6 months (a diminished time frame compared to long bones). The initial healing process, in order to return to normal function, typically takes an average of 4 to 6 weeks (depending on the type and severity of the fracture) and occurs in four stages ( Figure 10-17 ).
- 1.
Inflammatory stage: The fracture causes a disruption of the vascular supply within the bone. Initially the fracture site hemorrhages, with the formation of a hematoma throughout the fracture. This is followed by an inflammatory process with the presence of macrophages, monocytes, neutrophils, and platelets. The vascular compromise initially causes necrosis of bone at the fractured edges, but a reparative process of angiogenesis ensues, as well as the formation of osteoprogenitor cells, mesenchymal cells, and fibroblasts.
- 2.
Cartilaginous stage: This stage is the initiation of a cartilaginous (soft) callus that is comprised of fibrocartilaginous tissue. At the conclusion of this stage the mobility across the fracture is eliminated.
- 3.
Bony callus stage: This stage involves the conversion of the cartilaginous callus to a bony callus comprised of immature woven bone, which typically occurs within 3 to 4 weeks of the injury. This is initiated by the conversion of chondrocytes to osteocytes, leading to the formation of endochondral bone.
- 4.
Remodeling stage: This stage is the return of the osseous tissue to its pre-injury state and occurs for months following the injury. It is the final stage and results in the conversion of endochondral bone to mature lamellar bone.
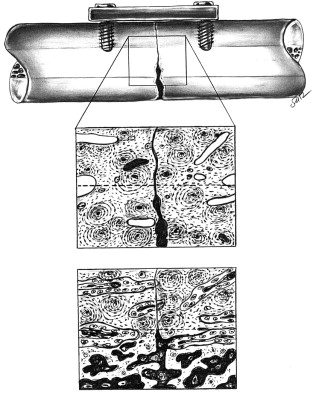
PRIMARY (DIRECT) BONE HEALING
Primary bone healing is a process of directly remodeling the haversian systems of compact lamellar bone by the use of rigid fixation. The use of rigid fixation stabilizes the fracture, optimizing contact healing. This eliminates the need for the intermediate steps required for a bony callus, and more rapidly returns the fracture to a pre-injury state ( Figure 10-18 ).
TREATMENT MODALITIES
CLOSED TREATMENT TECHNIQUES
Maxillomandibular Fixation
MMF is a basic and fundamental principle in the management and treatment of the maxillofacial trauma patient. It serves as a cornerstone, providing a stable base from which facial form and function can be restored. It re-establishes the patient’s premorbid occlusion, assisting in the reduction and fixation of simple and complex facial fractures. Most mandible fractures will require 4 to 6 weeks of MMF when used as the sole means of fixation; however, depending upon the fracture pattern, location, severity, and co-morbidities, some fractures will require 8 weeks. A variety of MMF techniques are available in today’s modern practice, including the following:
- 1.
Arch bars
- 2.
Intermaxillary fixation (IMF) screws
- 3.
Interdental wire fixation
- 4.
Skeletal suspension wires
- 5.
Various bonded and nonmetallic tooth-borne systems
Closed reduction techniques should be reserved for minimally to nondisplaced, favorable fractures, and for patients who have a complement of teeth sufficient to provide a stable occlusion. Some authors have advocated the use of MMF for comminuted mandible fractures, and in circumstances with compromised soft tissue. The concern is to avoid open techniques because of periosteal stripping, which could lead to necrosis of small bone fragments and potentially create a continuity defect and possible additional soft tissue loss. One concern with this type of management is the risk of infection, especially if there is soft tissue compromise or if the fracture involves a tooth-bearing portion of the mandible (open fracture). In addition, malunion or nonunion is possible considering that these fractures are highly unstable with inadequate bone buttressing. Lastly, severely comminuted bone does little to support the overlying soft tissue envelope. As scarring and contracture occur, regaining volume is often difficult to accomplish without recruiting distant tissue. These complications are often avoidable with early rigid stabilization, the use of external fixators, or the primary reconstruction with vascularized tissue when indicated.
Arch bars, which are the traditional workhorse for MMF, are applied to the dentition using circumdental wires. The patients are placed into their premorbid occlusion upon the final tightening of the intra-arch and inter-arch wires. Arch bars are very useful when managing dentoalveolar fracture segments because they assist in reestablishing the intra-arch contour; they also serve as a “tension band” that will resist the forces of tension seen along the alveolar level of the mandible. In addition, arch bars serve in directing vectors of force to assist in fracture reduction and reestablishment of the premorbid occlusion. While arch bars provide an effective and versatile means of MMF, their use is not without consequence. Increased surgical time both in placement and in removal, risk of penetrating injury to the surgeon, trauma to the periodontium, and compromised oral hygiene are all shortcomings of traditional arch bars. Arch bar placement in the pediatric patient can be complicated, depending on the patient’s age and stage of eruption. First, the position of the height of contour and contacts in the primary dentition may prevent application of circumdental wires. Second, there is the potential for extrusion of the primary tooth upon tightening the wire, especially in the root resorption stage for exfoliation ( Figure 10-19 ).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


