Traumatic injuries to the dentoalveolar structures are relatively common and occur from various causes. Among adults, these injuries may be caused by motor vehicle accidents, motorcycles, bicycles, assaults, falls, sports, and industrial-related accidents. In this age group, these injuries can also result iatrogenically from dentists and physicians during intraoral procedures, endotracheal intubation, and the management of comatose patients. Among younger children and toddlers, dentoalveolar injuries are most often caused by falls, especially during the first year of life. Another cause of dentoalveolar injuries and surrounding soft tissue among children can result from child abuse. In fact, roughly 50% of all physical injury associated with child abuse occurs in the head and neck region. Finally, certain medical conditions may predispose one to dentoalveolar trauma, such as a history of uncontrolled seizures. Among children of school age, dentoalveolar injuries occur mostly in the playgrounds and from bicycle accidents. At the teenage years, these injuries are most often caused by contact sports, motor vehicle accidents, and interpersonal violence. Mouth guards have been shown to significantly decrease the incidence of such injuries among this age group, and their use has been strongly supported by the American Dental Association. In addition, National Facial Protection Month, which occurs every April, has been successful in bringing attention to the prevention of sports-related injuries. This campaign has been promoted by the American Association of Oral & Maxillofacial Surgeons, as well as other specialties.
The reported prevalence of dentoalveolar injuries varies widely depending on factors such as the age of the studied group, the cause of injury, environment, and gender. In addition, because many of these injuries are treated in an outpatient setting, they tend to be overlooked in studies that look at the incidence of various types of focus on pediatric facial trauma. The general prevalence of dentoalveolar injury among pediatric patients is reported to be 5% of all facial fractures. Among adolescents with sport-related trauma, the incidence of dentoalveolar injuries is reported to be 36%. Overall, the prevalence of dentoalveolar injuries among children with primary dentition is 11-30%; among children with permanent dentition, it is 5-20%. Boys are affected almost twice as often as girls with a peak incidence at 2-4 years and 8-10 years.
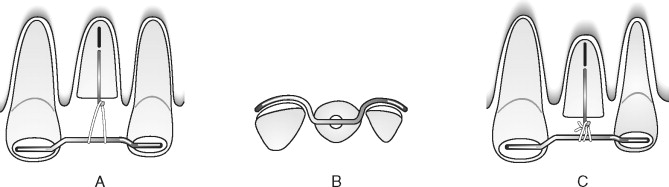
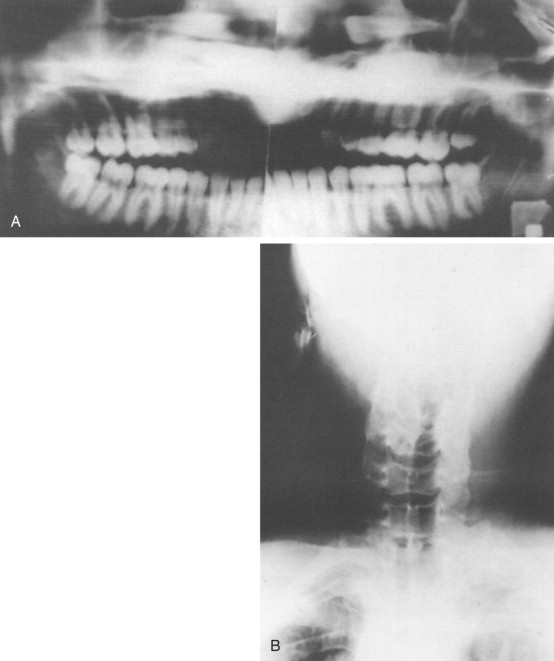
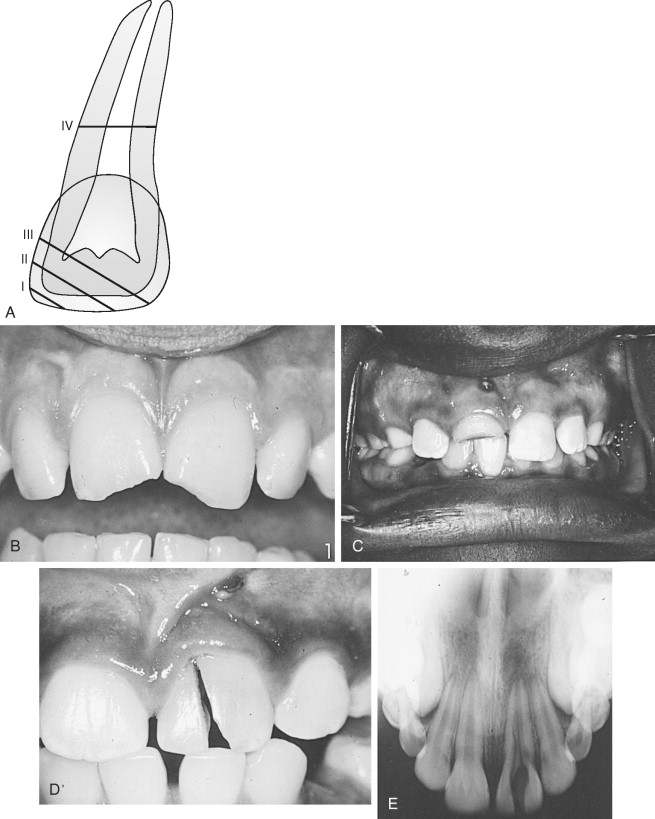
Injuries to the dentoalveolar structures can present as an isolated injury or in association with multi-system injury as seen in motor vehicle accident victims. Dentoalveolar injuries can also result from direct trauma to the teeth or from indirect trauma from mandibular dentition forcibly closing against the maxillary dentition. If the injury is caused by direct trauma, the most likely teeth to sustain injury in both the primary and permanent dentition are the maxillary central incisors because of their relatively exposed position ( Figure 9-1 ). This occurs most commonly when these teeth are protruding as in patients with Class II division I malocclusion or an overjet >5 mm or in patients with insufficient lip closure. These are followed in incidence by the upper and lower lateral incisors and the upper canines.
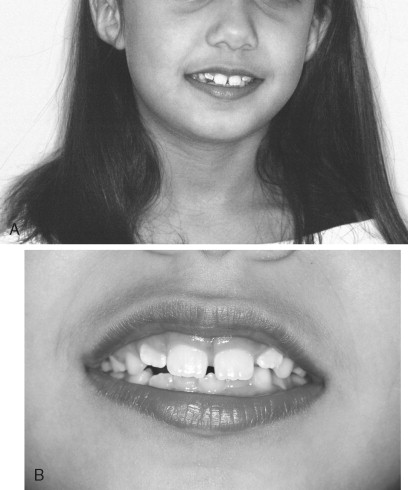
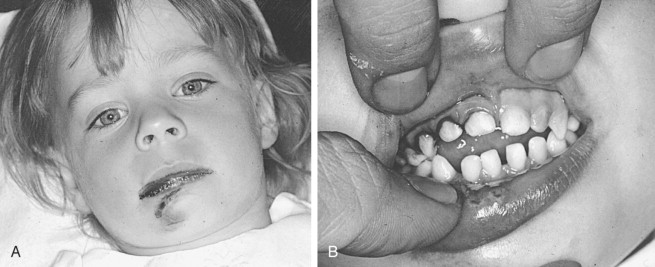
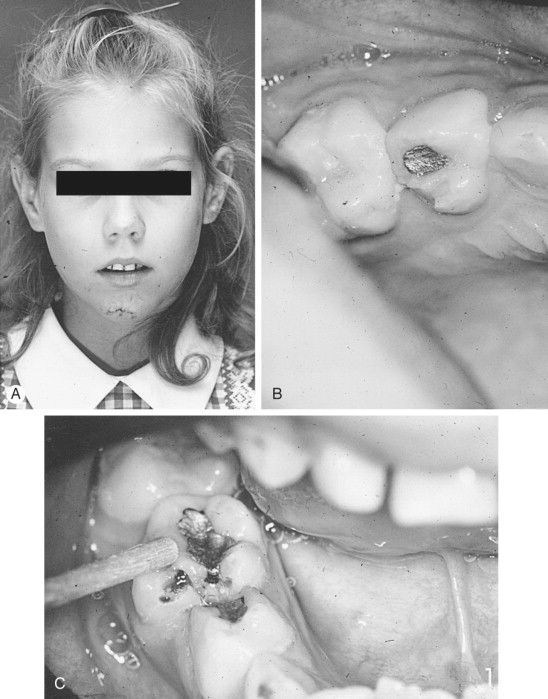
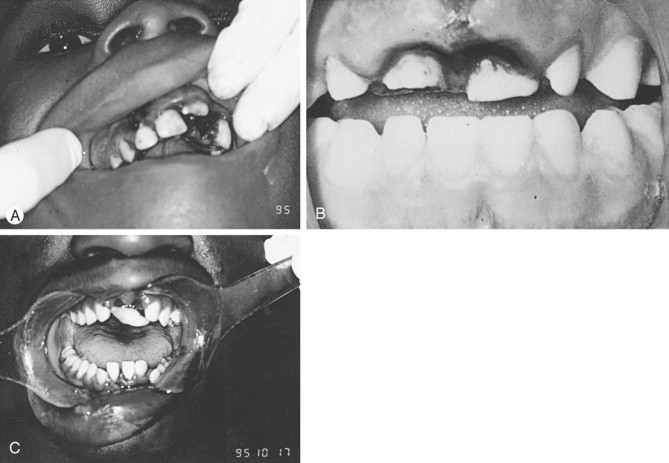
Depending on the force of the impacted trauma, direct injury mechanism can affect the upper or lower lip, occasionally causing laceration of the lip as well as dental or osseous alveolar fracture ( Figure 9-2 ). Dentoalveolar injury from indirect trauma usually results from force applied to the chin forcing the mandibular teeth against the maxillary dentition. The impact of this force often results in crown or crown-root fracture as well as condylar and/or symphyseal mandibular fracture and anterior intraoral soft tissue and submental laceration ( Figure 9-3 ).
The nature of dentoalveolar injuries also varies with age, possibly because of the anatomic differences between the teeth and supporting structures of adults and pediatric patients. The lack of sinus pneumatization, higher cancellous-to-cortical bone ratio, and the developing dentition within the facial skeleton tend to increase the elasticity of the facial bones, making them less vulnerable to fractures. Trauma to the primary dentition most often affects the supporting structure (luxation and exarticulation), whereas trauma to the permanent dentition mostly affects the teeth themselves (causes crown fractures). Only 10% of injuries to the primary dentition are crown and crown-root fractures. Seventy-five percent involve luxation or exarticulation of the tooth compared with incidence of mostly crown, crown-root fracture involvement in the permanent dentition.
HISTORY AND PHYSICAL EXAMINATION
Appropriate dentoalveolar injury repair must be preceded by a methodical and systematic diagnostic evaluation. Such an evaluation is primarily based on history and physical examination. Results of the history and physical examination will dictate the need for diagnostic radiographic or pulp testing. Once a diagnosis is established, a treatment can be formulated. Because length in time until treatment is important for the prognosis of dental and dentoalveolar injury, the process of diagnosis should commence immediately. However, definitive repair of a dentoalveolar injury may be delayed until the primary trauma survey is completed and life-threatening injuries are managed.
HISTORY
Obtaining a proper history can provide invaluable information for the diagnosis and management of dentoalveolar injuries. However, the practitioner must keep in mind that children in particular do not often offer a reliable and detailed history, especially after a traumatic event. In this situation, one must depend on the accompanying adult or other eyewitnesses. The history obtained from patients with dentoalveolar injury should include the following information :
- 1.
Biographic and demographic data of the patient including name, age, sex, race, address, and phone number.
- 2.
The time interval between the injury and presentation to the clinic or emergency room. This information is important since studies have shown that the sooner an injured tooth is treated, the better the prognosis. Furthermore, the success of treatment of luxated teeth, crown fractures with and without pulp exposure, and alveolar bone fractures may be influenced by delayed treatment.
- 3.
The place where the accident occurred may provide clues to the degree of bacterial contamination and possible need for tetanus prophylaxis.
- 4.
The nature of the accident can provide insight into the type of injury to be suspected. For example, a fall can cause injury to the maxillary anterior dentition, whereas a blow to the chin will often cause crown-root fractures of the premolar region with symphyseal or condylar fractures. In children and women, if the history of the injury does not correspond to the type of injury expected, abuse should be considered. In such instances it is important that the clinician carefully document the discussion with the patient and the findings. The nature of the injury may also provide information regarding other associated occult injuries. For example, if the patient is thrown forward against the dashboard as an unrestrained passenger or against the guard rail from a bicycle accident, an occult injury to the neck should be ruled out during the examination of the patient.
- 5.
Information related to the events surrounding the accident should also be recorded. In children, any discrepancy between the history and severity of injury should raise the suspicion of child abuse. This information should include whether there have been teeth or pieces of teeth noted at the site of the accident. Radiographic examination of the periapical tissues, chest, abdominal region, and perioral soft tissue is indicated when all the preinjury dentition has changed in form or quantity. Unaccounted for teeth or fragments of teeth must be searched for in body tissues or cavities. Information regarding the events surrounding the accident should also include whether any partially or completely avulsed teeth were replanted by the patient or parent and how a tooth was stored prior to presentation to the dentist or the emergency room. Finally, information of the events surrounding the accident should include whether the patient had loss of consciousness, confusion, nausea, vomiting, or visual disturbances after the accident. If any of these symptoms occurred, intracranial injury should be suspected and referral for neurological evaluation should be done following the treatment. If the patient is still having any of these symptoms, the patient should be referred for evaluation immediately and treatment of the dentoalveolar injury delayed until such evaluation is completed.
- 6.
The patient or parent should also be asked for information regarding any changes in the occlusion as a result of the injury. Such changes may indicate tooth displacement or dentoalveolar or jaw fractures.
- 7.
A short medical and dental history is taken to delineate any systemic or dental factors that can influence the immediate and later treatment plans. Such factors include the presence of major systemic illness, especially those that may influence the treatment, such as bleeding disorders and epilepsy. Also, knowledge of any previous oral and maxillofacial trauma may be helpful.
PHYSICAL EXAMINATION
An important aspect of the physical examination is the overall evaluation of the physical status of the patient. Guided by the finding of the history, the patient should be examined for presence of concomitant injury. Historical findings will direct the examiner to anticipate injury patterns, thereby promoting a focused examination. In addition, as with any trauma patient, the basic principles of ABCDE taught by Advanced Trauma Life Support (ATLS) should always take precedent. Abnormalities in vital signs may indicate intra-cranial injury, cervical spine injury, chest or abdominal injury, or even aspiration of an avulsed tooth. The mental status of the patient should also be assessed both by asking specific questions and by observing the patient’s reaction and behavior during the history and examinations. Once a general examination is completed and a concomitant injury is ruled out, a thorough oral and maxillofacial examination is performed. Such examinations should include the following :
- 1.
Extraoral soft tissue examination
Lacerations, abrasions, and contusions of the face, chin, forehead, and scalp should be identified and their depth, location, and proximity to vital structures should be established. The site of soft tissue trauma is a predictor of associated hard tissue injuries. Palpation of the temporomandibular joint and examination for range of jaw motion should be done to rule out condylar fracture.
- 2.
Intraoral soft tissue examination
Injuries of the oral mucosa, gingiva, lips, tongue, floor of the mouth, and cheek should be considered ( Figure 9-4 ). If present, such injuries should be carefully evaluated for the presence of foreign bodies, debris, and teeth or teeth fragments embedded within the tissue. It may be necessary to debride the oral cavity of clots and debris and to stop active bleeding before completing a thorough examination.

Gingival lacerations are often indications of displacement of teeth, whereas bleeding from non-lacerated marginal gingivae is often indicative of periodontal ligament damage or mandibular fracture. It is important that all teeth be accounted for at this time. Missing teeth or pieces of teeth that have not been left at the scene of the accident should be considered to have been aspirated, swallowed, or displaced into the soft tissues, the nasal cavity, or the maxillary sinus ( Figure 9-5 ). Therefore, a radiographic examination of the head and neck, chest, and abdomen should be performed to rule out presence of teeth or fragments in these tissues or organs.
- 3.
Examination of the jaws and alveolar bone
Fractures of the alveolar process protruding through the overlying mucosa are normally evident and readily detected by visual inspection. Mobility and crepitation of the palpated alveolar fracture segments confirm the underlying bone injury when the overlying mucosa is not lacerated. Fractures of the jaw may be detected by presence of gross malocclusion, step-off deformities, pain, and mobility of the fractured segment to palpation. Bleeding from the gingival crevice of a tooth, vertical laceration of the attached mucosa, and submucosal ecchymosis of the floor of the mouth are other signs of jaw fracture.
- 4.
Examination of the teeth
Direct examination of tooth structure is preceded by removing blood and debris from the teeth. Any infraction or fractures of the crowns should be noted. Infraction lines in the enamel can be detected by directing a light beam parallel to the long axis of the tooth. Crown fractures should be evaluated for extending into the dentin and the pulp. The size and location of pulp exposure should be recorded. Crown-root fractures in all quadrants should be evaluated as well. Changes in the color of a traumatized tooth and its translucency may indicate a pulp exposure. It is important to remember that indirect trauma leading to crown-root fractures in one quadrant is often accompanied by similar fractures in the ipsilateral opposing jaw.
- 5.
Examination for displacement of teeth
Displacement of teeth as a result of dentoalveolar trauma can usually be readily detected by visual examination. Examination of the dental occlusion may also be helpful in detecting minor degrees of tooth movements. Although displacement of teeth as a result of dentoalveolar trauma can occur in any direction, the most common displacement is in a buccolingual direction ( Figure 9-6 ). The direction and extent of displacement should be recorded. Lateral luxation and intrusion of teeth may present very minimal clinical symptoms because the teeth remain locked in this displaced position. Lingual and apical displacement of the apex of a primary tooth can interfere with its permanent successor.
- 6.
Examination for mobility of teeth
All teeth should be tested for both horizontal and axial mobility either by manual palpation or by use of a tongue blade. If a tooth does not appear to be displaced but is very mobile, a root fracture should be suspected. In such instances the location of the fracture usually determines the degree of mobility. When testing for mobility of one tooth, observing mobility of the adjacent teeth is suggestive of a dentoalveolar fracture.
- 7.
Reaction to percussion
Increased sensitivity to percussion in the absence of tooth displacement is indicative of injury to the periodontal ligament. This test can be performed by vertical and horizontal tapping of the tooth or by gentle finger tip pressure when examining smaller children. A non-injured tooth should be used for control. Sound elicited by percussion, with the use of the handle of a mouth mirror, has been mentioned in the literature as providing diagnostic information. An uninjured tooth will generally have a solid, metallic sound, whereas a luxated tooth will be dull. However, for this to be of any value would require a quiet environment.
- 8.
Pulp testing
The tooth vitality tests register the conduction of stimuli to the sensory receptors of the dental pulp. Vitality testing, however, may be difficult to perform or relatively unreliable in the acute setting following traumatic injury. Lack of cooperation and unreliability, especially among children, and false-negative results, common in acute injury, diminish the usefulness of pulp testing in the acute setting. Nonetheless, pulp testing several weeks later may be more accurate and should be performed before endodontic therapy. It can also be beneficial and important for planning treatment. Some of the methods used in pulp testing include a thermal test using treated gutta-percha, ice, ethyl chloride, carbon dioxide snow dichlorodifluoromethane, or electric vitalometers. The low sensitivity of some of these techniques led some to search for new methods of pulp testing. Laser Doppler flowmetry has been used in recent years as a more reliable method of assessing pulpal flow and vitality. Although promising, it still remains technique sensitive and time consuming.
RADIOGRAPHIC EXAMINATION
The purpose of radiographic examination is to provide information regarding injuries affecting the root portion of the tooth, periodontal ligaments, and status of the bone. Such information includes presence of root fracture, root infraction, and root dislocation ( Figure 9-7 ). It also serves to provide data on the presence of pre-existing periapical disease; presence of jaw fracture; degree of extrusion or intrusion; and presence of tooth, tooth fragment, or foreign bodies lodged in the soft tissue. In children and young adults radiographic examination serves to provide information regarding the extent of root development, size of the pulp chamber and root canal, and proximity of succedaneous teeth to the injured primary tooth. A single radiograph may not be sufficient to show a crown or root fracture. Radiographic imaging of dentoalveolar trauma usually consists of more than one radiograph and occasionally more than one projection (periapical, occlusal, and panoramic).
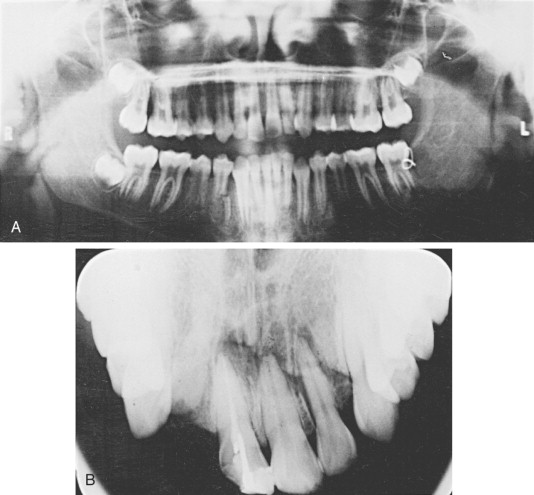
Correctly positioned periapical radiographs (central beam of x-ray parallel to the line of fracture) provide the most detailed information to adequately evaluate root fracture and dislocation of teeth. Often multiple views (ideally three) with different vertical and horizontal angulations of the central beam may be necessary to achieve this parallelism. Periapical radiographs are also used postoperatively to confirm position of the root.
Occlusal radiographs are particularly useful to diagnose a root fracture or lateral luxation with lingual displacement of the crown. Occlusal radiographs are also often made for patient comfort because they place minimal pressure on the traumatized area. They are also valuable in examining the floor of the mouth, tongue, cheek, or lip lacerations for teeth or teeth fragments in the soft tissue. When occlusal radiographs or other x-ray exposure is used to examine soft tissue, a reduced radiographic exposure time is recommended.
Radiographically displaced teeth will appear as a widening of the periodontal ligament space or displacement of the lamina dura. Extruded teeth may appear as a periapical radiolucency compatible with the pattern and shape of the apical portion of the root. Lateral and extensive luxation of teeth will also appear as a widening of the periodontal ligaments. Intruded teeth often will show minimal radiographic findings or only a blurred or absent periodontal space.
If jaw fractures or fractures of the alveolar ridges are suspected, extraoral radiographs such as panoramic view of the maxilla and mandible should be taken. Although panoramic radiographs can demonstrate fractures of the jaw, alveolar ridges, and teeth, they are best suited as a screening image for fractures of the condyle, subcondylar region, and angle or body of the mandible. Occasionally, access or use of routine dental radiograph is limited, such as in a hospital setting and in children under the age of 2 years old. Although CTs are more readily available in the emergency department setting, they have limited usefulness for dentoalveolar injuries. However, it remains the gold standard for imaging most facial bone fractures.
CLASSIFICATION OF DENTOALVEOLAR FRACTURES
Once the diagnosis of dentoalveolar injury is confirmed, a classification for such injury should be established. The purpose of such classification is to provide a comprehensive and universal description of the injury for communication and treatment planning purposes. Over the years many classifications of traumatic injuries to the teeth and supporting structures have been developed. These systems are based on a variety of factors such as etiology, anatomy of injury, pathology, and therapy. All systems of classification of dentoalveolar injuries have advantages and disadvantages. The three most common systems used for simple and comprehensive classification of dentoalveolar injuries are those developed by Ellis, by Sanders et al, and by Andreasen.
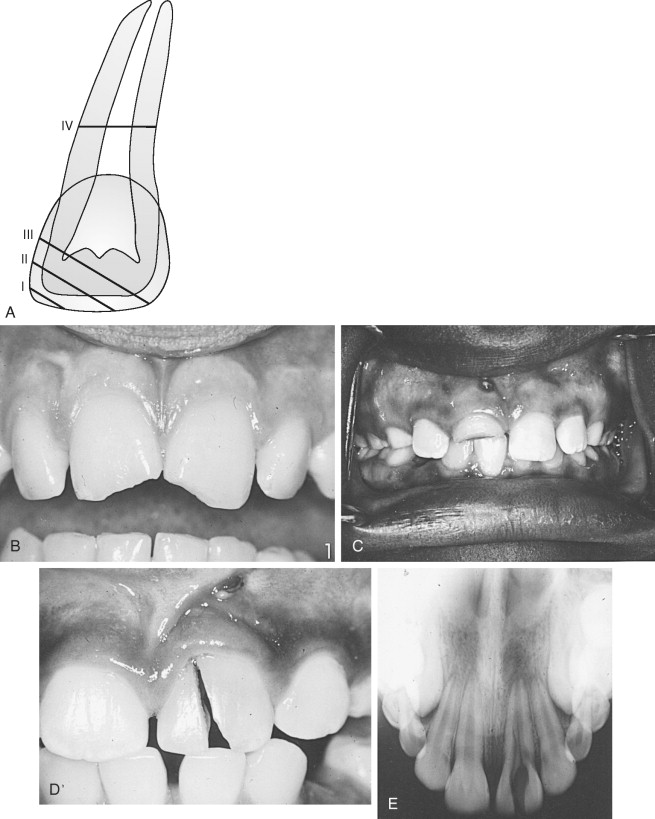
Ellis and Davey’s classification was originally developed and intended for classification of injuries to the anterior teeth ( Box 9-1 ). According to this classification, fractures of the teeth are divided into four categories. Class I fracture involves the enamel only; Class II fracture involves enamel and dentin; Class III fracture involves the pulp; and Class IV fracture involves the root ( Figure 9-8 ). Fractures can be further subdivided into diagonal, horizontal, and vertical (see Box 9-1 ). The major disadvantage of this classification is that it relies on memorization of a specific definition for each class.
| Class I | Enamel |
| Class II | Enamel and Dentin |
| Class III | Enamel, Dentin, and Pulp |
| Class IV | Root |
| Descriptive Classification of Fractures | |
| 1. Class II | Mesioangular |
| 2. Class III | Horizontal |
| 3. Class IV | Vertical |
Sanders et al offered a tooth fracture classification that simplified and eliminated the need for memorization by basing it solely on description of the injury sustained as a result of trauma. The classification depends on the tooth structure involved, the type of displacement (if any), and the direction of the crown or root fracture ( Box 9-2 ).
-
Crown craze or crack
-
No loss of tooth structure
-
Horizontal and vertical
-
Crown fracture
-
Only enamel involved
-
Enamel and dentin involved
-
Enamel, dentin, and pulp involved
-
Horizontal, vertical, or oblique
-
-
Crown-root fracture
-
No pulpal involvement
-
Pulpal involvement
-
-
Root fracture
-
Apical, middle, or cervical third
-
Horizontal or vertical
-
Sensitivity or concussion
-
Mobility, subluxation, or looseness
-
-
Tooth displacement
-
Intrusion
-
Extrusion
-
Labial
-
Lingual
-
Lateral
-
Avulsion or exarticulation
-
-
Compression fracture of the alveolar socket
-
Alveolar socket wall fracture
-
Lingual alveolar process fracture
-
Maxillary fracture
-
Mandibular fracture
Andreasen’s classification consists of the system originally adopted by the World Health Organization (WHO). It is the most widely used classification in the literature and includes description of injuries to the teeth, supporting structures, gingiva, and oral mucosa with some modifications to take into account anatomic, therapeutic, and prognostic considerations. The classification can be applied to both the permanent and primary dentition. In this classification, dentoalveolar injuries are divided into four major categories: injuries to the dental tissues and pulp, injuries to the periodontal tissues, injuries to the supporting bone, and injuries to the gingiva or oral mucosa. A description and illustration of the four categories are shown in Tables 9-1 to 9-4 .
| Injury Type | Description |
|---|---|
| Mucosal or gingival laceration | Shallow or deep mucosal wound from a tear and usually produced by a sharp object |
| Mucosal or gingival contusion | A bruise that is submucosal hemorrhage without mucosal break and usually produced by a blunt object |
| Mucosal or gingival abrasion | A superficial wound resulting in a raw, bleeding surface usually produced by rubbing or scraping of the mucosa |
CLASSIFICATION OF DENTOALVEOLAR FRACTURES
Once the diagnosis of dentoalveolar injury is confirmed, a classification for such injury should be established. The purpose of such classification is to provide a comprehensive and universal description of the injury for communication and treatment planning purposes. Over the years many classifications of traumatic injuries to the teeth and supporting structures have been developed. These systems are based on a variety of factors such as etiology, anatomy of injury, pathology, and therapy. All systems of classification of dentoalveolar injuries have advantages and disadvantages. The three most common systems used for simple and comprehensive classification of dentoalveolar injuries are those developed by Ellis, by Sanders et al, and by Andreasen.
Ellis and Davey’s classification was originally developed and intended for classification of injuries to the anterior teeth ( Box 9-1 ). According to this classification, fractures of the teeth are divided into four categories. Class I fracture involves the enamel only; Class II fracture involves enamel and dentin; Class III fracture involves the pulp; and Class IV fracture involves the root ( Figure 9-8 ). Fractures can be further subdivided into diagonal, horizontal, and vertical (see Box 9-1 ). The major disadvantage of this classification is that it relies on memorization of a specific definition for each class.
| Class I | Enamel |
| Class II | Enamel and Dentin |
| Class III | Enamel, Dentin, and Pulp |
| Class IV | Root |
| Descriptive Classification of Fractures | |
| 1. Class II | Mesioangular |
| 2. Class III | Horizontal |
| 3. Class IV | Vertical |
Sanders et al offered a tooth fracture classification that simplified and eliminated the need for memorization by basing it solely on description of the injury sustained as a result of trauma. The classification depends on the tooth structure involved, the type of displacement (if any), and the direction of the crown or root fracture ( Box 9-2 ).
-
Crown craze or crack
-
No loss of tooth structure
-
Horizontal and vertical
-
Crown fracture
-
Only enamel involved
-
Enamel and dentin involved
-
Enamel, dentin, and pulp involved
-
Horizontal, vertical, or oblique
-
-
Crown-root fracture
-
No pulpal involvement
-
Pulpal involvement
-
-
Root fracture
-
Apical, middle, or cervical third
-
Horizontal or vertical
-
Sensitivity or concussion
-
Mobility, subluxation, or looseness
-
-
Tooth displacement
-
Intrusion
-
Extrusion
-
Labial
-
Lingual
-
Lateral
-
Avulsion or exarticulation
-
-
Compression fracture of the alveolar socket
-
Alveolar socket wall fracture
-
Lingual alveolar process fracture
-
Maxillary fracture
-
Mandibular fracture
Andreasen’s classification consists of the system originally adopted by the World Health Organization (WHO). It is the most widely used classification in the literature and includes description of injuries to the teeth, supporting structures, gingiva, and oral mucosa with some modifications to take into account anatomic, therapeutic, and prognostic considerations. The classification can be applied to both the permanent and primary dentition. In this classification, dentoalveolar injuries are divided into four major categories: injuries to the dental tissues and pulp, injuries to the periodontal tissues, injuries to the supporting bone, and injuries to the gingiva or oral mucosa. A description and illustration of the four categories are shown in Tables 9-1 to 9-4 .
| Injury Type | Description |
|---|---|
| Mucosal or gingival laceration | Shallow or deep mucosal wound from a tear and usually produced by a sharp object |
| Mucosal or gingival contusion | A bruise that is submucosal hemorrhage without mucosal break and usually produced by a blunt object |
| Mucosal or gingival abrasion | A superficial wound resulting in a raw, bleeding surface usually produced by rubbing or scraping of the mucosa |
TREATMENT OF DENTOALVEOLAR INJURIES
GENERAL CONSIDERATIONS
Once all the appropriate diagnostic information has been obtained, a treatment plan can be formulated. Factors that will influence the treatment plan include the age and cooperation of the patient; whether it is a primary, mixed, or secondary dentition; the location and extent of the injury; and any concomitant injuries or co-morbidities. The overall goal of treatment of dentoalveolar fractures is to preserve the functional state of teeth, bone, and gingiva. Although every attempt should be made to maintain all of these structures permanently, it is sometimes necessary to either sacrifice or only temporarily maintain teeth for the overall good of the patient. Therefore, the final restorative plan should be taken into consideration when deciding whether and when to remove teeth or bony segments at the initial phase of treatment. The periodontal status of the teeth in the alveolar fracture should also be considered. Heroic attempts to maintain teeth that are otherwise unsalvageable for periodontal reasons should be avoided. Accordingly, teeth not useful in the final restorative plan should not be retained. On the other hand, teeth indicated for extraction in alveolar fractures may be retained temporarily to preserve at-risk alveolar bone. Maintaining proper alveolar contour and bulk will often allow for a more satisfactory dental rehabilitation. Likewise, avulsed teeth that have an extremely poor prognosis when associated with alveolar fractures may be replanted for a period of time as both a means of properly reducing the fracture and as physiologic space maintainers. Such a tooth or teeth can always be removed at a later date.
If root fractures are clinically evident, the teeth are removed if it can be accomplished without compromising the alveolar segment. Otherwise, they are left in place for removal at a later date after the segment is healed. Root fractures, particularly apical third fractures, are often only discovered on post-reduction radiographs taken in the dental office. These are managed in the same manner as if they had occurred without an alveolar fracture.
When dealing with alveolar fractures, debridement of bone should be conservative. The alveolar bones are highly vascular and vitality may often be maintained by even a very small soft tissue pedicel. Therefore, an attempt should always be made to retain fragments that have soft tissue attachments. The avulsed tooth associated with an alveolar fracture may have to be rigidly splinted for 3-4 weeks instead of physiologically splinted for 7-10 days.
The sequence of treatment of dentoalveolar fractures is an inside-to-outside approach that includes bone, teeth, and then soft tissue. Accordingly, underlying alveolar bone injuries are treated first, followed by placement or reduction of the teeth as they relate to the underlying bone, and then the soft tissues are repaired. Treatments of the dental injuries, such as the restoration of tooth fractures, are the last priority. Finally, the presence of other, more serious injuries, or the hospital setting rather than a well-equipped dental office, may preclude optimal treatment of the dental injury. For example, avulsed teeth may not be promptly replanted, fractured teeth may not be efficiently pulp capped and restored, and ideal splints may not be placed. Compromises are often necessary and appropriate for the overall good of the patient.
TREATMENT OF INJURIES TO THE HARD DENTAL TISSUES AND PULP
CROWN INFRACTION
No treatment is indicated for crown infraction or cracks in the enamel layer. These injuries may be easily missed and may require direct transillumination to diagnose. However, teeth with crown infraction should be evaluated periodically to monitor the status of the pulp to determine the need for or the nature of treatment at a later time.
CROWN FRACTURES
Enamel Fractures
The usual treatment for an enamel fracture is to smooth the sharp edges of the enamel and observe the tooth. The accident impact force is not always proportional to the size of the fracture and the pulp could later become necrotic, hence the need for periodic follow-up.
Enamel and Dentin Fractures
Crown fractures account for 60-70% of all traumatic injuries seen in the dental office. Emergency treatment of enamel and dentin fractures is designed to reduce the hyperemia and protect the pulp against any thermal stimuli and bacterial contamination. A calcium hydroxide base should be placed on the exposed dentin followed by an immediate temporary protective acid-etch resin restoration. Acid-etch resin restorations should hold the calcium hydroxide in place for a sufficient length of time (ideally 6-8 weeks) to allow secondary dentin formation. A light-cured glass ionomer liner/base (e.g., Vitrebond [3M Dental Products, St Paul, MN]) can be used in place of calcium hydroxide. Resin restorations should restore the contact area, prevent movement of adjacent teeth into the fractured area, and provide sufficient incisal length to prevent the tooth from moving lingually ( Box 9-3 ).
Class I (Enamel)
-
Smooth sharp edges and observe
-
Relieve occlusion
Class II (Enamel and Dentin)
-
Calcium hydroxide base or light-cured glass ionomer liner/base on dentin
-
Restore with acid etch resin
-
Relieve occlusion
Class III (Pulp Exposure)
Vital Pulp
-
Calcium hydroxide direct pulp cap for small exposures within 24 hours
-
Incomplete apex:
-
Calcium hydroxide pulpotomy for large exposures within 24 hours or small exposures over 24 hours old
-
Closed apex:
-
Root canal therapy for large exposures or small exposures over 24 hours old
-
Non-Vital Pulp
-
Incomplete apex: apexification
-
Closed apex: root canal therapy
Class IV (Root)
-
Vertical—extract
-
Apical or middle third—splint 12 weeks only if excessive mobility
-
Cervical third—root canal therapy and orthodontic extrusion of segment
Concurrently, restoring crown contour will prevent over-eruption of the opposing tooth. Intermediate resin restorations also allow the tooth to be pulp-tested. After allowing for secondary dentin buildup, the final acid-etch resin restoration can be placed.
Enamel, Dentin Fractures, and Pulp Exposure.
Four factors contribute to the management of more complex (Class III) crown fractures: (1) the length of time elapsed since the injury occurred, (2) the size of the pulp exposure, (3) the condition of the pulp (vital or non-vital), and (4) the stage of root development. The main factor in determining prognosis after any form of pulp exposure is minimizing the bacterial invasion of the pulp.
Pulp Exposure with Vital Pulp.
The prognosis is best for teeth with a vital pulp exposure if the fracture is treated within the first 2 hours. A direct pulp cap is indicated for small pinpoint exposures occurring at the pulp horn of a tooth, but not on axial pulpal line angles. If a tooth with an open apex and a small pulp exposure (1.0-1.5 mm; 1 pulp horn) is seen within 24 hours, it should be directly pulp-capped with calcium hydroxide. Calcium hydroxide pulpotomies or partial calcium hydroxide pulpotomies remove the superficial area of infected pulp and should be performed for larger exposures or small exposures over 24 hours old in teeth with open apices. This procedure has a very high success rate, regardless of the size of the exposure or time elapsed since injury, provided the pulp was healthy prior to injury. The direct pulp cap or calcium hydroxide pulpotomy is designed to allow a tooth with an open apex to complete root development (apexogenesis). An intermediate protective restoration should be placed. The treatment objective is to maintain the vitality of the pulp and to allow for apexogenesis. A tooth with a vital pulp and incomplete root formation has the best recovery prognosis. Usually teeth that have calcium hydroxide pulpotomies will ultimately need root canal therapy along with a post-and-core plus a crown.
In fractures with a vital pulp and a closed apex, a direct pulp cap should be performed if there is a small pulp exposure and the patient is seen within 24 hours. If the pulp exposure is larger than 1.5 mm, or if it has been present longer than 24 hours, root canal therapy should be performed.
Pulp Exposure with Non-Vital Pulp.
Root canal therapy should be performed if the pulp is necrotic and there is a mature apex. Apexification procedures should be performed if there is a necrotic pulp with an immature apex. The purpose of this procedure is to provide a calcific seal at the apex prior to condensing the gutta-percha. This differs from apexogenesis in which completion of the root occurs. In the apexification technique, the canal is cleansed and a calcium hydroxide paste is placed in the canal ( Figure 9-9 ). In 3-6 months the tooth should be evaluated radiographically for a calcific bridge. If bridging has occurred, a root canal with gutta-percha can be performed. On occasion the apexification technique might take up to 18 months and the calcium hydroxide might have to be replaced every 3-6 months. In successful apexification treatment, teeth do not undergo physiologic dentin apposition and they are left with thin dentinal walls. If a tooth with a successful apexification technique is injured again, the tooth would be more susceptible to a cervical third root fracture caused by the thin dentinal walls.

Crown-Root Fractures.
The treatment of crown-root fractures depends on several factors, including the location of the fracture, the apical extent of the fracture, and whether or not the pulp is involved. Generally, emergency treatments of this type of fracture include stabilization of the coronal fragment to the adjacent teeth and removal of loose fragments before definitive treatment can be started. In fractures that are longitudinal and follow the long axis of the tooth, or if the coronal fragments comprise more than one third of the clinical root, extraction is generally recommended. If the fracture line is above or slightly below the cervical margin, appropriate forms of conservative therapy can usually be used to restore the tooth. Such therapies usually include crown-lengthening procedures or orthodontic elevation of the fracture site to provide for access for restorative margins. The treatment of this type of fracture is also influenced by whether the apex of the tooth is open or closed. If the tooth is mature and restorable, endodontic treatment is indicated prior to restoration, whereas if the tooth is immature and the apex is open, a pulpotomy should be performed with a calcium hydroxide base and the tooth followed radiographically for closure of the apex. After such closure, definitive root canal therapy and permanent restoration can be completed.
Root Fractures.
Root fractures generally occur in teeth with complete root development and are usually of the oblique type. Clinically, a root fracture is usually seen as an extruded tooth displaced lingually. Most root fractures occur in the apical and middle third and only rarely in the cervical third.
Radiographs taken immediately after an injury may not show a horizontal or diagonal root fracture. Separation of the fragments must be substantial in root fractures to appear on a radiograph. Only after a week or two—when hemorrhage, inflammation, and resorption have caused the fragments to separate—will the radiograph show the damage more conclusively. Diagonal root fractures are the most difficult to diagnose. In suspected diagonal root fractures, a foreshortened (45-degree angulation) and an elongated (110-degree angulation) periapical film should be taken in addition to the standard 90-degree angulation. Vertical root fractures in a labio-lingual but not in a mesio-distal direction are easily discernible on a radiograph ( Figure 9-10 ). Extraction is the proper treatment in vertical root fractures.
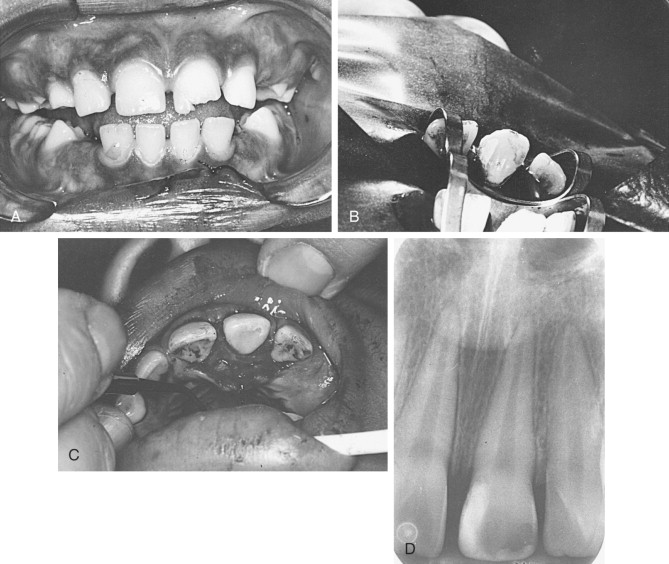
Root fractures in the apical or middle third are usually not splinted unless there is excessive mobility. Treatment of root fractures with mobility consists of apposition of the fractured segments with rigid splinting for 12 weeks. Splinting for 3 months is necessary since the repair of root fractures is similar to, although slower than, the repair in bone fractures.
Root fractures can heal by four different modalities: (1) calcified tissue, (2) connective tissue, (3) bone and connective tissue, and (4) granulation tissue. Healing by calcified tissue is usually seen in teeth with immature roots or in teeth with little or no fragment separation. Radiographically, the segments are not rounded at the edges. In connective tissue healing, radiographically the segment edges are rounded, with partial or complete pulpal obliteration. In healing with bone and connective tissue, each segment has its own periodontal ligament, and total calcific metamorphosis of both segments is a usual occurrence. In healing with granulation tissue, the teeth are usually loose, slightly extruded, and sensitive to percussion. The pulp in the coronal segment is usually necrotic whereas in the apical segment it is vital.
Root canal therapy is withheld for apical and middle third root fractures, until there is evidence of pulpal necrosis. Pulpal necrosis is usually seen only in the coronal segment. Increased separations of the segments with an adjacent radiolucency are indications of pulpal necrosis. Endodontic treatment for root fractures consists of: (1) pulpectomy of the coronal segment only, (2) pulpectomy of both segments, or (3) pulpectomy of the coronal segment with surgical removal of the apical segment.
Treatment for cervical third root fractures usually involves extraction of the tooth or orthodontic extrusion of the root. In orthodontic treatment of a cervical third root fracture, the coronal segment is removed and a root canal is performed in the remaining segment. A post space is prepared by removing gutta-percha from the coronal part of the canal. A 0.018-inch, stainless steel wire with a hook at the incisal area is then cemented in the canal with temporary cement. An additional wire (0.036-inch, stainless steel wire) is placed high on the incisal edges of the adjacent teeth using the acid-etch resin technique. The hook is tied into this wire with elastic thread or chain AlastiK (3M Dental Products, St Paul, MN) ( Figure 9-11 ). Rapid extrusion of 3-5 mm can be done in a 2- to 4-week period. The root should be in retention for 6-8 weeks before a post-and-core and crown are fabricated. Formation of new bone and normal periodontal ligament is seen by 7 weeks.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses