Diagnosis
and Management of
Abnormal Frenum
Attachments
An abnormal labial frenum attachment can cause many problems for the dentition, such as an abnormal midline diastema. A midline diastema is a gap between the maxillary central incisors; it can be a normal occurrence during transitory stages of the dentition (during the primary, early, and middle mixed dentitions). However, a diastema can also be considered as an abnormal separation of incisors, that is, as a malocclusion.
Clinicians must be able to differentiate between these two types of diastema and know when and how to manage the abnormal diastema. Figure 9-1 shows two diastemata, developed from two different etiologic factors: an abnormal diastema developed because of impinging deep bite and an abnormal diastema caused by abnormal frenum attachment. Many factors other than an abnormal frenum attachment can cause an abnormal diastema; ways to differentiate between these causes are presented in this chapter.
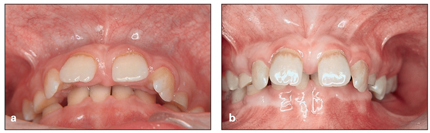
Fig 9-1 (a) Diastema caused by impinging deep bite. (b) Diastema caused by abnormal frenum attachment.
As Baum1 stated, the midline diastema is usually a part of normal dental development during the transitional stage of the eruption of maxillary lateral incisors. It gradually disappears as the canines erupt, and the central incisors come into complete contact with each other.
In 1907, Angle2 described the midline diastema as a common form of malocclusion distinguished by a space of varying degrees (1 to 5 mm in width) between the maxillary incisors. He suggested that it always presented an unpleasing appearance and noted that it was rarely seen between mandibular central incisors. He also suggested that the frenum was a cause of a midline diastema and outlined a method for its removal.
Broadbent3 described the “ugly duckling stage” as a normal developmental phenomenon seen in most children. The permanent maxillary central incisors are flared laterally at the beginning of eruption because the unerupted lateral incisors constrain the roots of the central incisors. During this process, the medial erupting path of the maxillary lateral incisors, and later the maxillary canines, results in normal closure of the midline diastema. However, in some individuals, the diastema may not close spontaneously; an abnormal space remains between the incisors and causes other problems for adjacent teeth and for occlusion.
The presence of a diastema between the maxillary central incisors is considered an unacceptable esthetic and malocclusion problem by many adults. However, other individuals, including some actors, singers, and other celebrities, have a distinct diastema and do not mind.
In contrast to the maxillary diastema, which can be a part of the normal transitional stages of occlusal development, the mandibular diastema is not a normal growth characteristic. Because of the relatively larger size and the position of mandibular permanent incisors compared with the primary incisors, the mandibular permanent incisors often erupt with some amount of crowding.
Prevalence
A review of older literature indicates that the midline diastema was of concern to patients and was considered an unacceptable malocclusion, and clinicians were very interested in the etiology and treatment of this problem. In 1882, Farrer4 described a method for the correction of diastema.
According to many epidemiologic investigations, the prevalence of midline diastema is high during the early mixed dentition and decreases between the ages of 9 and 12 years. In normal conditions, it closes after complete eruption of the permanent canines.5–7
In general, the midline diastema is more prevalent in females than in males. Richardson et al8 studied the sex prevalence of diastema in 5,307 children between 6 and 14 years of age. They found that, at age 6 years, females showed a higher prevalence than males, but, at age 14 years, males had a higher prevalence.
Racial differences also exist; Lavelle9 investigated the distribution of midline diastema in different human populations and reported that the prevalence is greater in Africans (West Africa) than in British whites or Chinese from Hong Kong and Malaysia.
Horowitz10 evaluated the racial differences of midline diastema in a group of over 700 children, 397 black children and 321 white children, between the ages of 10 and 12 years. He found that 19% of the total sample of black children had a midline maxillary diastema of 2 mm or more compared with 8% of the while children.
Taylor5 examined 516 children between 5.5 and 11.0 years of age and found that 66 of 68 children in the 5.5- to 6-year age group (97%) showed spacing between incisors. In the 6- to 7-year group, the prevalence of diastema was 87.7%, and in the 10- to 11-year group, 48.7% showed midline diastema. In another study of children aged 12 to 18 years, Weyman11 reported a 7% occurrence.
Brunelle et al,12 analyzing a national health and nutrition survey carried out in the United States, reported that a maxillary diastema of 2 mm or more was present in 19% of 8- to 11-year-olds, 6% of 12- to 17-year-olds, and 5% of adults aged 18 to 50 years.
Etiology of Midline Diastema
Initiation of any treatment for a midline diastema must be based on proper evaluation of the extent, etiology, and pathogenesis of the diastema. The possible influence of the superior labial frenum in relation to the midline diastema has been of great interest to clinicians for many years. The presence of persistent diastema has often been blamed on an enlarged labial frenum. Sometimes, without a proper evaluation of the etiology of a particular diastema, frenectomy has been performed unnecessarily, although many other factors can be involved in this abnormality. Therefore, the cause of a diastema must be evaluated in regard to both the anatomical structure of frenum tissue and other causes of abnormal diastema.
Morphogenesis and structure of the frenum
The frenum can be the original cause of a diastema in only a small proportion of midline diastemata. According to Huang and Creath,13 the superior labial frenum begins to form in the 10th week of gestation, and by the 3rd month in utero the morphology of the fetal frenum is similar to that of the abnormal frenum of postnatal life. It extends as a continuous band of tissue from the tuberculum on the inner side of the lip, over and across the alveolar ridge, to be inserted in the palatine papilla. Before birth, the lateral halves of the alveolar ridge unite, and the continuous band of tissue becomes totally enclosed by bone; it is divided into a palatal portion (palatine papilla) and a labial portion (superior labial frenum) by this closure.
The frenum of a newborn at the gum pad stage and before eruption of the dentition is a large, fleshy attachment with a wide origin. The tissue gradually narrows, attaching in the midline to the connective tissue of the internal maxillary suture and alveolar process. With the eruption of teeth and development of the alveolar ridge, the position of the frenum changes. As growth progresses, the frenum may atrophy and may assume a higher position or maintain its attachment to the papilla.
It has been suggested that a slight clefting of intercrestal bone can hold the teeth apart and cause an abnormal diastema.14
In a study of dogs, Picton and Moss15 hemisectioned the mandibular first molar and disked the mesiodistal contact of other teeth in one side of the arch and produced artificial interdental spacing between the halves of the first molar on one side. After a few weeks, they found an enlarged space between the two parts of the sectioned tooth. One half moved mesially, and the other half moved distally because the transseptal fibers were not present between the roots of the divided molar, while other created spaces were spontaneously closed. They concluded that the transseptal fibers are one of the principle factors that bring about and maintain the interstitial mesiodistal contacts of the teeth in each arch.
Stubley16 compared the transseptal fibers to an orthodontic chain used for interdental space closure. He stated that transseptal fibers do not contain elastic tissue; they are made of collagen, and the motive power that they exert derives from tiny coils into which they contract as they mature; the force generated varies from individual to individual.
Stubley16 described persistent midline diastema where interdental fibers are characterized by their strength and a wide space develops in the maxillary midline. In the absence of any pathologic condition, the underlying cause is congenital and is due to the presence of a persistent midline suture that interferes with arrangement of the transseptal fibers. Instead of passing directly across the interdental space from one tooth to the other, the fibers turn upward at a right angle from the mesial aspect of each central incisor to enter the suture. Such an arrangement is like a break in the transseptal fiber chain, and the distal transseptal fibers of developing central incisors can move them apart. This fiber pattern could account for difficulty in the spontaneous diastema closures.
Martin and Jones17 examined 17 consecutive individuals with various forms of holoprosencephaly at autopsy or during clinical evaluation and found that 88% of the patients were missing the superior labial frenum, regardless of the severity of holoprosencephaly or other associated craniofacial defects. Holoprosencephaly is a cephalic disorder in which the prosencephalon (the forebrain of the embryo) fails to develop into two hemispheres. Hox genes, which guide placement of embryonic structures, fail to activate along the midline of the head, allowing structures that are normally paired on the left and right to merge. Martin and Jones17 stated that absence of the frenum in individuals with holoprosencephaly provides evidence that the frenum has its embryonic origin in the medial nasal process.
Dean et al18 stated that the maxillary labial frenum is composed of two layers of epithelium enclosing a loose vascular connective tissue. In some instances, the frenum may include muscle fibers that originate from the orbicularis oris muscle of the upper lip. The origin from the lip is often wide, but the tissue of the frenum itself narrows and is inserted in the midline into the outer layer of the periosteum and into connective tissue of the internal maxillary suture and alveolar process. The frenum may attach at variable locations in the attached gingival tissue some millimeters above the crest of the ridge, or on the ridge, or the fibers may pass between the central incisors and attach to the palatine papilla. Figure 9-2 shows an abnormal diastema caused by heavy and low attachment of an abnormal frenum.

Fig 9-2 Abnormal diastema caused by heavy, low frenum attachment.
The frenum may be completely absent, or its existence may be a part of normal transition stage of dentition. With the completion of incisor and canine eruption, the gap spontaneously closes.
Other causes of midline diastema
Besides the anatomical structure of the frenum (size, position, and type of insertion), other causes of midline diastema must be considered before treatment planning and frenectomy are initiated. Possible therapeutic approaches include orthodontics, restorative dentistry, surgery, or various combinations of these. The ideal treatment should seek to close the diastema in question but also address the cause behind it.
During incisor transition, because permanent incisors are larger than primary incisors (incisor liability), some mechanisms interact to compensate for these width differences and enable normal development of occlusion. Mandibular incisors generally erupt with some degree of crowding, while maxillary incisors, because of their position and inclination, erupt with some degree of spacing. Depending on their size, this can be considered a normal transitional condition or can be a sign of an abnormal situation that deserves early detection and intervention before complete development.
In the normal transitional stage of maxillary incisors, a midline gap of up to 3 mm is normal. The mesial inclination of maxillary lateral incisors and their mesial force during eruption reduce or completely close this gap; eruption of the maxillary permanent canines with the same mechanism will completely close the remaining gap between central incisors. However, persistent midline diastema is also an ethnic norm for some races that have large dentoalveolar arches, such as African and Mediterranean groups.
To differentiate between normal transitional changes in the dentition that result in spacing in the maxillary permanent incisors from other factors that cause abnormal spacing, clinicians must carefully examine the patient’s occlusion intraorally and extraorally through clinical and radiographic evaluation. Incisor separations can result from one or more of the following factors:
• Lateral incisor hypodontia
• Microdontia of maxillary lateral incisors (peg-shaped lateral incisors)
• Presence of mesiodens or odontoma
• Deleterious oral habits
• Muscle imbalance (lip dysfunction)
• Impinging deep bite
• Anterior Bolton discrepancy
• Pathologic tooth migration
Lateral incisor hypodontia
One common cause of midline diastema is congenital absence of one or both maxillary lateral incisors (Fig 9-3). Sustained diastema after complete eruption of the central incisors is a diagnostic clue for early detection of this problem, which must be evaluated by radiograph. A remaining diastema with no midline shift is usually accompanied by absence of both lateral incisors, and a remaining diastema with a shift of midline is usually the consequence of one absent lateral incisor.
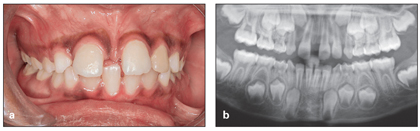
Fig 9-3 (a and b) Severe diastema caused by a congenitally missing maxillary right lateral incisor.
Depending on the type of occlusion and other conditions, treatment options are closing the diastema and using canine substitution or closing the diastema, aligning the anterior teeth, and replacing the missing teeth with conventional prostheses or implants (see chapter 7).
Microdontia of maxillary lateral incisors
Abnormal maxillary midline diastema can be the result of small incisors, that is, peg lateral incisors, which can be unilateral or bilateral (Fig 9-4).

Fig 9-4 Diastemata caused by missing teeth and microdontia of the central incisors.
Depending on the type of occlusion, the age of the patient, and the patient’s desires, treatment options can be building up the small lateral incisor with composite resin, veneers, or crowns or extraction and space closure (see chapter 7).
Presence of mesiodens or odontoma
Another common cause of midline diastema is the presence of supernumerary teeth. The mesiodens is the most common type of supernumerary tooth (Fig 9-5). Early detection and diagnosis are not difficult if the incisor transition is carefully monitored. The presence of supernumerary teeth in the incisor area has some clinical signs that can help in early detection, including asymmetric or retarded tooth eruption, retained diastema after complete eruption of the lateral incisors, and rotation of the central incisors.

Fig 9-5 Diastema caused by mesiodens.
The treatment of choice depends on the patient’s occlusion, dental age, and root formation of the incisors. Some treatment options include early detection and extraction of the supernumerary tooth and guidance of eruption and incisor alignment by segmental bonding (see chapter 8).
Deleterious oral habits
Another common cause of midline diastema or interdental spacing of incisors is abnormal habits, such as finger sucking, tongue thrust, and lip biting or lip dysfunction (Figs 9-6 and 9-7).

Fig 9-6 Diastema caused by thumb sucking.

Fig 9-7 Diastema caused by tongue dysfunction.
The treatment of choice in this situation is early detection, habit control, and space closure (see chapter 6).
Muscle imbalance (lip dysfunction)
One of the most important factors influencing incisor relationships and maintaining normal occlusion is inner and outer muscle balance around the dental arches. Midline diastema can be caused by orofacial muscular imbalances, such as macroglossia, improper tongue posture and position, and flaccid lip muscles (Fig 9-8).
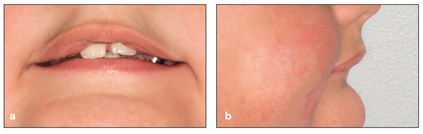
Fig 9-8 (a and b) Diastema caused by lip dysfunction.
Proper treatment of these conditions involves elimination of causative factors and space closure. Long-term stability depends on proper long-term retention.
Impinging deep bite
Deep bite malocclusions, especially Class II division 1 malocclusions with impinging bite caused by a severe curve of Spee and overeruption of mandibular incisors, is a common type of malocclusion that can cause incisor flaring and midline diastema.
The treatment of choice for this type of diastema is early intervention and correction of the curve of Spee, correction of deep bite, and then space closure and incisor retraction (see Fig 9-1a).
Anterior Bolton discrepancy
Another cause of midline diastema is an abnormal anterior ratio, which can be determined through the Bolton analysis.19 This discrepancy results from the presence of relatively large mandibular incisors or small maxillary incisors in comparison to each other.
Space closure must be accompanied by a reduction in the size discrepancy between maxillary and mandibular incisors, either by enamel stripping or extraction of the bigger incisors or buildup of the smaller incisors (see chapter 5 on correction of incisor crowding).
Pathologic tooth migration
Another cause of incisor spacing and flaring, especially in the adult dentition, is development of a pathologic condition, such as cystic formation, bone loss due to periodontal problems, or some systemic condition that causes bone loss and tooth migration. Increased areas of inflammation cause bone loss, loss of attachment, and consequently migration of teeth from the pocket (Fig 9-9).

Fig 9-9 Diastema caused by pathologic tooth migration.
Management of this condition, especially in advanced situations, is very challenging and requires a multidisciplinary approach. Any orthodontic tooth movement and treatment must wait until a thorough evaluation has been completed and the cause has been eliminated.
Effects of Abnormal Frenum Attachment on Occlusion
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


