Introduction
Our aim was to assess the prevalence of gingival recessions in patients before, immediately after, and 2 and 5 years after orthodontic treatment.
Methods
Labial gingival recessions in all teeth were scored (yes or no) by 2 raters on initial, end-of-treatment, and posttreatment (2 and 5 years) plaster models of 302 orthodontic patients (38.7% male; 61.3% female) selected from a posttreatment archive. Their mean ages were 13.6 years (SD, 3.6; range, 9.5-32.7 years) at the initial assessment, 16.2 years (SD, 3.5; range, 11.7-35.1 years) at the end of treatment, 18.6 years (SD, 3.6; range, 13.7-37.2 years) at 2 years posttreatment, and 21.6 (SD, 3.5; range, 16.6-40.2 years) at 5 years posttreatment. A recession was noted (scored “yes”) if the labial cementoenamel junction was exposed. All patients had a fixed retainer bonded to either the mandibular canines only (type I) or all 6 mandibular front teeth (type II).
Results
There was a continuous increase in gingival recessions after treatment from 7% at end of treatment to 20% at 2 years posttreatment and to 38% at 5 years posttreatment. Patients less than 16 years of age at the end of treatment were less likely to develop recessions than patients more than 16 years at the end of treatment ( P = 0.013). The prevalence of recessions was not associated with sex ( P = 0.462) or extraction treatment ( P = 0.32). The type of fixed retainer did not influence the development of recessions in the mandibular front region ( P = 0.231).
Conclusions
The prevalence of gingival recessions steadily increases after orthodontic treatment. The recessions are more prevalent in older than in younger patients. No variable, except for age at the end of treatment, seems to be associated with the development of gingival recessions.
A gingival recession is defined as the displacement of the marginal tissue apical to the cementoenamel junction. Although its etiology is unclear, periodontal disease and mechanical trauma are considered the primary factors in the pathogenesis of gingival recessions. Orthodontic treatment might promote the development of recessions. A possible mechanism is that orthodontic tooth movement can result in root positions close to or outside alveolar cortical plates; this can lead to bone dehiscences. As a result, a marginal gingiva without proper alveolar bone support can migrate apically, leading to root exposure. Furthermore, a fixed orthodontic appliance creates retention areas for dental plaque. In case of inadequate removal of the plaque, gingival inflammation could lead to periodontal breakdown. In addition, a similar effect might be caused by long-term wear of a plaque-accumulating bonded retainer attached to the 6 anterior teeth in patients with poor oral hygiene. Irrespective of the mechanism, the results of a recent systematic review imply that orthodontic therapy can cause a small mean worsening of periodontal status, including the development of gingival recessions.
An understanding of the association between orthodontic treatment and the development of gingival recessions is important because more and more children, teenagers, and adults are being treated orthodontically. For example, data from the United States show that the proportion of children who received orthodontic therapy increased from about 15% to more than 30% for those born in 1950s and 1970s, respectively. Furthermore, most patients desire orthodontic treatment for esthetic reasons. This motivation is independent of the geographic location or the affluence of the country. However, gingival recessions can negatively affect the esthetics of the dentition and compromise the treatment results.
Population-based investigations have demonstrated that the development of gingival recessions depends on age: their prevalence is lower at younger ages and increases over time. For example, recessions of more than 3 mm were present in 6%, 24%, and 54% of patients aged 14 to 19, 20 to 29, and 30 to 39 years, respectively. In other words, the proportion of patients with severe recessions increased almost 10-fold from the late teenage years to adulthood. To date, studies that focused on the development of gingival recessions in orthodontic patients evaluated samples either immediately or several years after treatment. The latter ones, however, were limited to only 1 long-term observation. Consequently, the dynamics of the development of gingival recessions could not have been evaluated. Moreover, most investigations were limited to the assessment of incisors and canines, with little attention given to other teeth. Therefore, the aims of this study were (1) to assess a change of prevalence of gingival recessions in a large representative cohort of patients during and 2 and 5 years after orthodontic treatment, (2) to evaluate the development of recessions in various regions of the dental arches, and (3) to identify variables associated with their development.
Material and methods
A cohort of 302 patients was selected from the archives of the Department of Orthodontics and Craniofacial Biology, Radboud University Nijmegen Medical Centre in The Netherlands, according to the following inclusion criteria: (1) treated with full fixed appliances; (2) bonded lingual retainer placed directly after active orthodontic treatment; (3) no orthodontic retreatment; and (4) good-quality dental casts available before treatment, after treatment, 2 years after treatment, and 5 years after treatment. All patients had a lingual retainer bonded either only to the mandibular canines (type I retainer; Fig 1 ) or to all 6 mandibular anterior teeth (type II retainer; Fig 2 ) during the entire posttreatment period. In all patients, 4 mandibular incisors were present 5 years after treatment.


Sex, age at the 4 assessment times, information on extraction vs nonextraction treatment alternative, and type of retainer were obtained from the patient files. Angle classification was determined on the right side of the pretreatment plaster models. The type of retainer was confirmed by inspection of the plaster models made after treatment.
In the 302 subjects, 117 (38.7%) were male and 185 (61.3%) were female. The distribution of the Angle classifications at pretreatment was as follows: 51 patients (16.9%) were Class I, 247 patients (81.8%) were Class II, and 4 patients (1.3%) were Class III. The mean ages were 13.6 years at the beginning of orthodontic treatment and 16.2 years at the end of treatment ( Table I ). The mean treatment duration was 2.8 years. One hundred ninety-five patients (64.6%) were treated without extractions, 52 (17.2%) had extractions of 4 teeth (1 tooth in each quadrant), 29 (9.6%) had extractions of only 2 maxillary teeth, and 26 (8.6%) had other types of extractions. In 167 patients (55.3%) patients, a lingual retainer was bonded only to the mandibular canines (type I retainer), whereas 135 patients (44.7%) had a retainer bonded to all 6 mandibular anterior teeth (type II retainer).
| Mean | SD | Minimum | Maximum | |
|---|---|---|---|---|
| Age at pretreatment | 13.6 | 3.6 | 9.5 | 32.7 |
| Age at end of treatment | 16.2 | 3.5 | 11.7 | 35.1 |
| Age 2 years after treatment | 18.6 | 3.6 | 13.7 | 37.2 |
| Age 5 years after treatment | 21.6 | 3.5 | 16.6 | 40.2 |
| Duration of treatment | 2.6 | 0.8 | 1 | 6 |
| Posttreatment period | 5.4 | 0.4 | 4.6 | 6.4 |
Labial gingival recessions in all teeth were scored (yes or no) on initial, end-of-treatment, and posttreatment (2 and 5 years later) plaster models. A recession was noted (scored “yes”) if the labial cementoenamel junction was exposed. The judgment was made independently by 2 calibrated observers (A.M.R. and A.R.) after meticulous inspection of the plaster models.
The recessions were analyzed as recessions in the mandibular incisors, recessions in the rest of the dentition, and recessions in all teeth.
Statistical analysis
Descriptive statistics with means and standard deviations were calculated to report the findings at the 4 assessment times. The presence of a recession is a dichotomous variable; therefore, kappa statistics were used to assess observer performance. In the pilot study, the kappa values were computed to express agreement between the 2 scores for the gingival recessions: one obtained by clinical examination, and the other by scoring the plaster models. In the main study, the kappa values were calculated for interobserver and intraobserver concordance.
Fisher exact tests were run to identify differences in the development of recessions between male and female subjects, those younger than 16 years vs those older than 16 years of age at the end of treatment, subjects with extraction vs nonextraction treatment, subjects with type I vs type II retainers, and subjects with the various Angle classifications.
Regression analyses were carried out to investigate an association between the increase of gingival recessions from the end of treatment to 5 years later in the whole dentition, the mandibular incisor region, the remaining teeth, and the 6 teeth with the highest prevalence of recessions (maxillary right and left first premolars, mandibular right and left first premolars, and mandibular right and left central incisors) (dependent variables), and age at the end of treatment, sex, and extraction vs nonextraction treatment (independent variables).
The validity of the use of plaster casts for scoring recessions was assessed in a pilot study with 30 randomly selected adults (mean age, 42.0 years; SD, 10.4; range, 18.1-54.8 years). First, an observer (A.M.R.) scored (yes or no) the presence of gingival recessions in all regions of the dental arches during clinical examinations. Then, maxillary and mandibular alginate impressions were taken to make plaster casts. Finally, the same observer determined the presence of gingival recessions on the plaster models 3 months after the clinical examinations.
Clinically, 147 recessions were identified (scored “yes”) in 20 of the 30 patients, whereas 137 recessions were identified on 20 of the 30 plaster models. In 21 teeth, the clinical and model scores were identical (kappa = 1). The scores were different for 7 teeth (once for the maxillary right second premolar, maxillary left canine, mandibular left second molar, and mandibular right central incisor; twice for the maxillary right canine, maxillary left central incisor, and mandibular right second molar). However, the mean kappa score was greater than 0.800, suggesting good agreement.
To determine intraobserver agreement for the judgment of gingival recessions in the main study, we randomly selected 80 dental casts of 20 patients to be reevaluated by both observers (A.M.R. and A.R.). The kappa values for recession were calculated for each tooth and each time. At pretreatment and end of treatment, perfect agreement was found (kappa = 1) for all scored teeth. At 2 years after treatment, the agreement was perfect for 28 teeth (kappa = 1) and good or very good for the remaining teeth (kappa values of 0.67-0.93). At 5 years after treatment, the concordance was perfect (kappa = 1) for 26 teeth and very good for the remaining teeth (kappa values of 0.80-0.95). Because of the high interobserver concordance, the scores of observer 1 (A.M.R.) were used for further analysis. Intraobserver agreement ranged from 0.798 (for the mandibular right second molar) to 1. The mean kappa value was 0.98.
Results
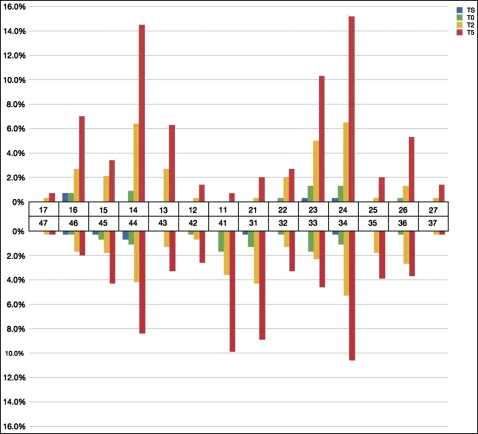
The prevalences of gingival recessions at the 4 times are shown in Table II . The frequencies of gingival recessions per tooth at all time points are given in Figure 3 .
| Subjects | Recessions in mandibular incisors | Recessions in rest of dentition | Recessions in all teeth | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| TS | T0 | T2 | T5 | TS | T0 | T2 | T5 | TS | T0 | T2 | T5 | |
| With no recessions (n) | 301 | 294 | 281 | 259 | 297 | 286 | 249 | 199 | 297 | 282 | 241 | 188 |
| With recessions (n) | 1 | 8 | 21 | 43 | 5 | 16 | 53 | 103 | 5 | 20 | 61 | 114 |
| With recessions (%) | 0.3 | 2.6 | 7 | 14.2 | 1.7 | 5.3 | 17.5 | 34.1 | 1.7 | 6.6 | 20.2 | 37.7 |
| With 1 recession (n) | 1 | 6 | 15 | 22 | 2 | 8 | 20 | 29 | 2 | 11 | 21 | 32 |
| With 2 recessions (n) | – | 1 | 4 | 13 | 2 | 5 | 14 | 29 | 1 | 4 | 18 | 25 |
| With 3 recessions (n) | – | 1 | 1 | 5 | 1 | 2 | 5 | 15 | 2 | 2 | 7 | 20 |
| With 4 recessions (n) | – | – | 1 | 3 | – | 1 | 6 | 12 | – | 2 | 5 | 14 |
| With 5 recessions (n) | – | – | – | – | – | – | 4 | 6 | – | – | 2 | 6 |
| With 6 recessions (n) | – | – | – | – | – | – | – | 1 | – | 1 | 2 | 3 |
| With 7 recessions (n) | – | – | – | – | – | – | 1 | 2 | – | – | 1 | 2 |
| With 8 recessions (n) | – | – | – | – | – | – | – | 5 | – | – | 2 | 2 |
| With 9-14 recessions (n) | – | – | – | – | – | – | 3 | 4 | – | – | 3 | 10 |
| Total recessions (n) | 1 | 11 | 30 | 75 | 9 | 28 | 143 | 315 | 10 | 39 | 173 | 390 |
The increases of overall gingival recessions from pretreatment to after treatment were similar in both sexes ( P = 0.462). Also, patients who had been treated without extractions showed comparable overall development of gingival recessions at posttreatment as did the patients who had had extractions ( P = 0.320).
Age at the end of treatment was associated with the increased numbers of recessions. Patients who were younger than 16 years at completion of orthodontic treatment were less likely to develop recessions than patients who were 16 or older at the end of treatment ( P = 0.013).
The type of fixed retainer—bonded to canines only or bonded to all 6 front teeth—did not influence the development of recessions in the mandibular front region ( P = 0.231). Also, the pretreatment Angle classification had no association with the number of recessions at 5 years posttreatment ( P = 0.523).
The results of the regression analyses estimating the effects of age at the end of treatment, sex, and extraction vs nonextraction treatment on the increased number of recessions from end of treatment to 5 years later are presented in Table III . The age at pretreatment was associated with the increase of the overall number of recessions after treatment. The value of the odds ratio (OR = 1.097; P = 0.014) can be interpreted as follows: a risk of increasing the number of recessions grows by 9.7% with each subsequent year after the end of treatment. In other words, an 18-year-old patient has a 9.7% higher chance to develop more recessions 5 years after treatment than does a 17-year-old.



