Introduction
In this cephalometric investigation, we analyzed the treatment effects of bone-anchored maxillary protraction (BAMP) with miniplates in the maxilla and mandible connected by Class III elastics in patients with Class III malocclusion.
Methods
The treated sample consisted of 21 Class III patients consecutively treated with the BAMP protocol before the pubertal growth spurt (mean age, 11.10 ± 1.8 years) and reevaluated after BAMP therapy, about 1 year later. The treated group was compared with a matched control group of 18 untreated Class III subjects. Significant differences between the treated and control groups were assessed with independent-sample t tests ( P <0.05).
Results
Sagittal measurements of the maxilla showed highly significant improvements during active treatment (about 4 mm more than the untreated controls), with significant protraction effects at orbitale and pterygomaxillare. Significant improvements of overjet and molar relationship were recorded, as well as in the mandibular skeletal measures at Point B and pogonion. Vertical skeletal changes and modifications in incisor inclination were negligible, except for a significant proclination of the mandibular incisors in the treated group. Significant soft-tissue changes reflected the underlying skeletal modifications.
Conclusions
Compared with growth of the untreated Class III subjects, the BAMP protocol induced an average increment on skeletal and soft-tissue advancement of maxillary structures of about 4 mm, and favorable mandibular changes exceeded 2 mm.
The literature reports a series of treatment approaches regarding orthopedic treatment in Class III malocclusion. However, effective maxillary protraction remains limited to the deciduous or early mixed dentition. Preliminary studies have indicated success of maxillary protraction in the late mixed or permanent dentition phase (ages, 10-12 years) with innovative treatment techniques that use bone anchors and Class III elastics. The use of temporary anchorage devices in maxillary protraction has increased over recent years, but they have not yet been assessed in controlled studies.
The purpose of this controlled clinical trial was to evaluate the effects of a treatment protocol for Class III malocclusion consisting of surgically placed miniplates in both the maxilla and the mandible connected by Class III elastics (bone-anchored maxillary protraction, BAMP). Specifically, we assessed the active treatment effects in skeletal, dentoalveolar, and soft-tissue facial structures of consecutively treated patients, compared with growth changes in a matched control group of untreated Class III subjects.
Material and methods
The treated group comprised 21 consecutive patients with dentoskeletal Class III malocclusion treated by 1 operator (H.D.C.) with the BAMP technique. Success of therapy at the end of the observation period was not a determining factor for selection of patients, since the treated sample was collected prospectively.
At the initial observation (T1), all patients had Class III malocclusion in the mixed or permanent dentition characterized by a Wits appraisal of –1 mm or less (mean, –4.8 ± 2.8 mm), anterior crossbite or incisor end-to-end relationship, and Class III molar relationship. All patients were of white ancestry, with a prepubertal stage of skeletal maturity according to the cervical vertebral maturation method (stage 1 or 2). Eighteen of the 21 patients were still prepubertal at the end of treatment (T2) (stages 1-3), whereas 3 patients were in stage 4.
A control group of 18 untreated subjects with dentoskeletal Class III malocclusion was obtained from the Department of Orthodontics of the University of Florence in Italy. The control group matched the treated group as to type of dentoskeletal disharmony, skeletal maturation at each time point, sex distribution, and mean duration of observation intervals ( Table I ).
| BAMP (n = 21) Mean |
SD | Controls (n = 18) Mean |
SD | Difference | t | Significance | |
|---|---|---|---|---|---|---|---|
| A-VertT (mm) | 63.9 | 4.1 | 63.3 | 3.9 | +0.6 | 0.64 | NS |
| Co-A (mm) | 93.7 | 3.8 | 92.4 | 4.1 | +1.3 | 0.32 | NS |
| Ptm-VertT (mm) | 13.8 | 3.2 | 12.9 | 3.4 | +0.9 | 0.40 | NS |
| Or-VertT (mm) | 52.3 | 3.9 | 51.6 | 3.5 | +0.7 | 0.56 | NS |
| Pr-VertT (mm) | 66.6 | 4.9 | 65.3 | 4.1 | +1.3 | 0.38 | NS |
| Id-VertT (mm) | 65.7 | 6.6 | 66.9 | 5.5 | −1.2 | 0.54 | NS |
| B-VertT (mm) | 61.9 | 6.7 | 62.5 | 5.6 | −0.6 | 0.76 | NS |
| Pg-VertT (mm) | 61.5 | 7.2 | 62.6 | 6.5 | −1.2 | 0.59 | NS |
| Co-Gn (mm) | 123.1 | 4.5 | 124.1 | 3.7 | +1.3 | 0.34 | NS |
| Co-Go (mm) | 60.0 | 3.2 | 61.9 | 3.8 | +1.9 | 0.04 | ∗ |
| Go-Gn (mm) | 72.5 | 3.4 | 73.4 | 2.9 | +0.9 | 0.44 | NS |
| Wits (mm) | −4.8 | 2.8 | −5.2 | 2.9 | +0.4 | 0.43 | NS |
| Mx-Md diff (mm) | 29.8 | 4.1 | 31.7 | 3.9 | −1.9 | 0.15 | NS |
| Ba-T-VertT (°) | 40.2 | 4.1 | 38.3 | 3.6 | +1.9 | 0.14 | NS |
| Co-T-VertT (°) | 44.6 | 4.3 | 43.1 | 3.9 | +1.5 | 0.21 | NS |
| ML-SBL (°) | 29.6 | 4.8 | 27.9 | 3.7 | +1.7 | 0.22 | NS |
| NL-SBL (°) | 1.6 | 1.9 | 0.8 | 2.2 | +0.8 | 0.23 | NS |
| NL-ML (°) | 27.9 | 4.3 | 27.2 | 3.4 | +0.7 | 0.58 | NS |
| Co-Go-Me (°) | 128.9 | 3.3 | 127.2 | 3.8 | +1.7 | 0.36 | NS |
| ANS-Me (mm) | 61.6 | 4.1 | 60.4 | 3.7 | +1.2 | 0.54 | NS |
| U1-NL (°) | 112.4 | 6.2 | 114.4 | 5.1 | −2.0 | 0.02 | ∗ |
| L1-ML (°) | 88.5 | 4.0 | 87.0 | 4.2 | +1.5 | 0.25 | NS |
| Overjet (mm) | −1.0 | 2.1 | −1.3 | 2.0 | +0.3 | 0.65 | NS |
| Overbite (mm) | 1.3 | 1.6 | 2.2 | 1.9 | −0.9 | 0.07 | NS |
| Molrel (mm) | −5.2 | 1.5 | −4.5 | 1.8 | −0.7 | 0.24 | NS |
| Sn-VertT (mm) | 79.2 | 4.6 | 77.7 | 4.1 | +1.5 | 0.29 | NS |
| A′-VertT (mm) | 79.4 | 4.7 | 77.6 | 4.2 | +1.8 | 0.32 | NS |
| Ulip-VertT (mm) | 82.3 | 5.2 | 80.9 | 5.4 | +1.4 | 0.42 | NS |
| Llip-VertT (mm) | 82.1 | 6.3 | 82.0 | 4.8 | +0.1 | 0.95 | NS |
| B′-VertT (mm) | 75.7 | 6.5 | 76.6 | 4.6 | −0.9 | 0.63 | NS |
| Pg′-VertT (mm) | 75.3 | 7.1 | 75.6 | 5.9 | −0.3 | 0.88 | NS |
| Age (y.mo) | 11.10 | 1.8 | 11.6 | 1.7 | +0.4 | 0.73 | NS |
In the BAMP orthopedic protocol, in each patient, 4 miniplates were placed on the left and right infrazygomatic crest of the maxillary buttress and between the mandibular left and right lateral incisors and canines. Small mucoperiosteal flaps were elevated, and modified miniplates (Bollard, Tita-Link, Brussels, Belgium) were secured to the bone by 2 (mandible) or 3 (maxilla) screws (diameter, 2.3 mm; length, 5 mm). The extensions of the plates perforated the attached gingiva near the mucogingival junction ( Fig 1 ). Three weeks after surgery, the miniplates were loaded. Class III elastics applied an initial force of about 150 g on each side, increased to 200 g after 1 month of traction, and to 250 g after 3 months. The patients were asked to replace the elastics at least once a day and wear them 24 hours per day. In 14 patients, after 2 to 3 months of intermaxillary traction, a removable biteplate was placed in the maxillary arch to eliminate occlusal interference in the incisor region until correction of the anterior crossbite was obtained. The surgeons’ and patients’ experiences and problems with the plates were described by De Clerck et al.

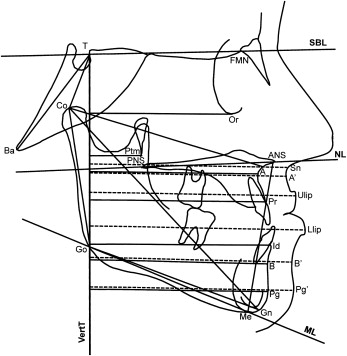
Cone-beam computed tomograms (CBCTs) were taken immediately after the placement of the miniplates at T1 and after approximately 1 year at T2. The scans were acquired by using an iCat machine (Imaging Sciences International, Hatfield, Pa) with a 16 × 22-cm field of view. The CBCTs were used to create synthetic lateral cephalograms with magnification of 7.5% (version 10.5, Dolphin Imaging & Management Systems, Chatsworth, Calif). The enlargement factor of the control cephalograms was similar, and no correction was made for enlargement in the analysis of the films. All cephalograms were digitally traced by 2 examiners, using the Dolphin and Viewbox (version 3.1, dHal, Kifissia, Greece) softwares. The cephalometric measures selected were based on a previously described reference system traced through craniofacial stable structures, with the addition of orbitale (Or) to Vertical T (VertT), pogonion (Pg) to VertT, inclination of the incisors to their respective bases, Wits appraisal, maxillomandibular differential (Mx-Md diff), and a soft-tissue analysis with linear distances from anterior nasal spine (ANS′), Point A (A′), upper lip (Ulip), lower lip (Llip), Point B (B′), and Pg′ to VertT ( Fig 2 ).