Author, year
Study population
Medication (indication)
Implant complication
Time of onset or follow-up
Development of BRONJ
Starck, 1995 [2]
1 patient with 5 implants
Not given
Implant loss, bone exposure
6 months
Yes?
Kushner, 2005 [18]
2 cases
Alendronate
BRONJ and implant loss (both cases) pathological fracture (one case)
3 and 4 months
Yes
Marx, 2005 [6]
119 patients with BRONJ
116 IV (oncologic)
Implant loss, bone exposure
Not given
4 (3,4 %) of BRONJ cases induced by implants (1 on IV rest not given)
3 p.o. (osteoporotic)
Jeffcoat, 2006 [19]
50 patients with 210 implants
25 patients p.o.
Success >99 % in both groups
Longer than 3 years
No
25 controls (no medication)
Brooks, 2007 [9]
1 patient with 10 implants and grafting
p.o. (osteoporotic) for 2 years
Infection, explantation of 1 implant with sequestrotomy
2 years
Yes
Wang, 2007 [20]
1 patient with 5 implants
p.o. for >10 years
Infection, implants kept
1 year
Yes
Marx, 2007 [21]
30 patients with BRONJ, thereof 2 caused by implant placement
p.o.
Yes
Fugazzotto, 2007 [22]
61 patients with 169 implants, 22/39 thereof put at time of tooth removal
p.o. (4 patients osteoporotic dose, 57 patients prophylactic dose) for 3.3 years on average
1 case with bone exposure and spontaneous healing
12–24 months
No
Yarom, 2007 [23]
11 patients with BRONJ, thereof 2 with implants and 1 with “implant extraction”
Oral
BRONJ, implant loss
2, 7, and 14 months in these 3 patients
Yes
Grant, 2008 [24]
115 patients with 468 implants
Oral
2 failed, 1 was successfully replaced, 1 was not replaced
2–10 years
None
Bell, 2008 [25]
42 patients with 100 implants and 68 bone grafts
Oral
5 implants failed but were successfully replaced
4–89 months average: 37 months
None
Kasai, 2009 [26]
65 women of more than 36 years of age
11 on oral BP for osteoporosis with 35 implants
5 implants without osseointegration in 3 patients (14, 3 %)
None
40 on no medication with 161 implants
7 implants without osseointegration in 7 patients (4, 3 %)
Goss, 2010 [27]
16.000 patients with 28.000 implants
Unselected dental implant clientele
7 cases of implant failure in patients with oral bisphosphonate medication
3 cases: no osseointegration 4 cases: late failure
None
Bedogni, 2010 [28]
1 patient with 2 implants and bone augmentation
Oral BP for osteoporosis
Primary osseointegration, late infection
2 years
Yes
Lazarovici, 2010 [29]
114 BRONJ patients with 27 implant-related BRONJ cases
11 implant-related BRONJ cases on oral BP
Early infection or primary osseointegration and late infection
16,2 months mean duration until BRONJ development
Yes
16 implant-related BRONJ cases on i.v. BP
Martin, 2010 [30]
8,752 patients, 589 of them with implants
Oral BP
16 patients with 26 implant complications
Early and late implant failure (4 weeks to 11 years)
None did meet AAOMS criteria
Shabestari, 2010 [31]
21 patients with 46 implants
Oral BP
None
No
Koka, 2010 [17]
137 postmenopausal women
55 on oral BP
1 of 121 implants lost
No
88 without BP therapy
3 of 166 implants lost
Bojer, 2011 [12]
1 patient with 4 mandibular implants
IV (steroid-induced osteoporosis)
Uneventful healing
35 months
No
Famili, 2011 [32]
23 patients with 75 implants
p. o.
1 lost but replaced
1–3 years
No
Zahid, 2011 [33]
26 patients with 51 implants
p. o.
3 implants lost
No
Ferlito, 2011 [34]
1 patient with extractions and immediate implants
IV for multiple myeloma
BRONJ in the only extraction site where no implant was put (!)
Yes
Zebuhr, 2012 [13]
2 patients with cured BRONJ, 9 implants
p.o. (osteoporotic)
None
9 and 12 months
No
Diniz-Freitas, 2012 [35]
20 consecutive BRONJ cases, 2 thereof after implant surgery
p.o. (osteoporotic)
Yes
Flichy-Fernandez, 2012 [36]
1 patient (drug holiday and CTX test before implant surgery)
p.o. (osteoporotic)
BRONJ, bone loss, but implants kept
Yes
Subramanian, 2012 [37]
6 implants in 1 patient
p.o. (osteoporotic)
Primary osseointegration, late implant loss
8 years after implant surgery, 7 years after BP therapy start
No
Gupta, 2012 [38]
2 implants in 1 patient (CTX test before implant surgery)
p.o. (osteoporotic)
Bone sequestration, implant loosening in 1 implant, 1 implant without problems but no prosthetic use
6 weeks
No
Lopez-Cedrun, 2013 [39]
9 patients with BRONJ after dental implants
7 patients: osteoporosis
7 of 9 recovered
Average BRONJ onset 20,9 months after implant surgery, range 1–34 months
9 patients with BRONJ after dental implants
1 patient: osteoarthritis
1 patient: polymyalgia rheumatica
Mattheos, 2013 [40]
Implant surgery and augmentation in 1 patient
IV (osteoporotic)
None
6 months
No
Jacobsen, 2013 [4]
110 BRONJ patients with
Two thirds with oncological indication
Infection, explantation
Average BRONJ onset 20,9 months after implant surgery
12 cases of BRONJ induced by implants
12 cases of BRONJ induced by implants
One third with anti-osteoporotic indication
Number of implants = 23
Yip, 2013 [16]
337 female implant patients, 1,181 implants, aged min. 40 years
Oral BP therapy
In patients with implant failure, odds of oral BP use was 2,69-fold higher (95 %-CI: 1.49-4,86) than in adjusted controls with no implant failure
6–14 years
No
Rugani, 2014 [41]
1 patient with cured BRONJ
IV (osteoporotic)
None
No
Implant-Associated Infections in Bisphosphonate Medication Versus Common Periimplantitis
Periimplantitis in non-bisphosphonate cases usually initiates in the interface between mucosa and implant surface as a mucositis. Then it affects the integrity of the bone-implant junction in a bone resorption process in direction from crestal to apical. If untreated, a gap between implant and bone is generated and osseointegration is lost. Contrarily, it was shown that the jaw bone develops sequestrum which includes the implant itself, but histologically, osseointegration of the implant can persist [3, 42]. One could explain this with regard to the fact that bone resorption is inhibited by the bisphosphonates, especially near to the surface of the bone, while deep in the bone marrow, there is still potential for a process like sequestration (Figs. 17.1 and 17.2).
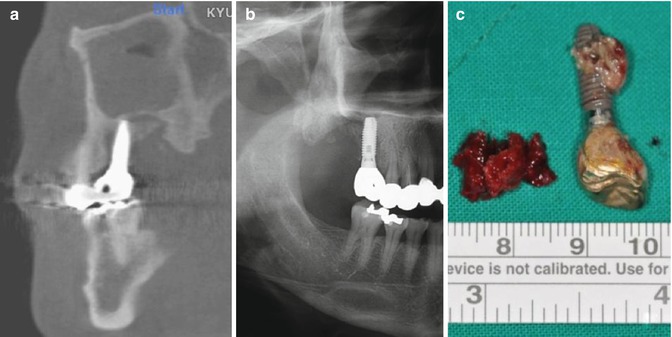
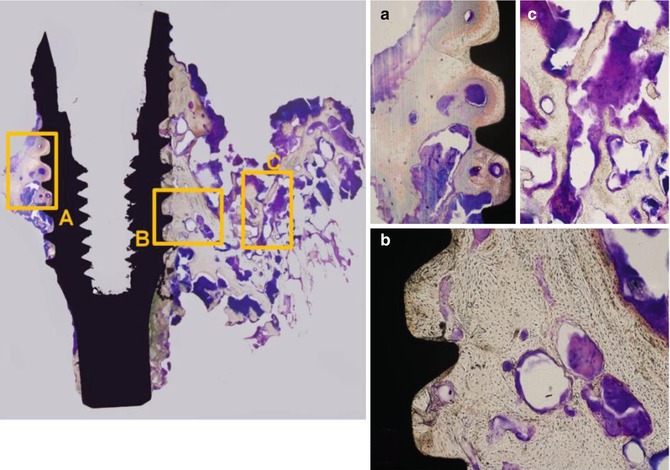
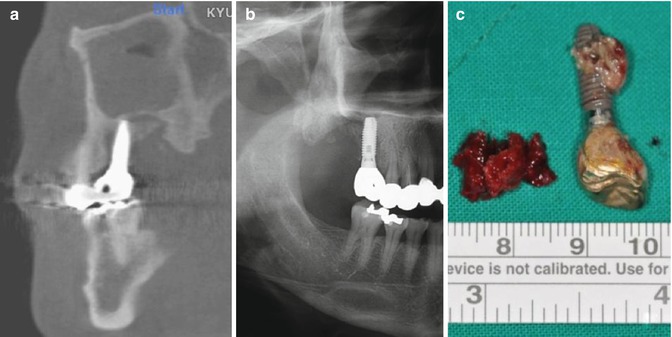
Fig. 17.1
The patient initiated alendronate 1 year before installation of the two implants at the left maxilla. Four years later after implantation and BP coverage, one posterior implant was removed at a local clinic because of the bone exposure and pain. (a, b) Radiographic bone destruction around the remaining implant maintaining the partial bone-implant contact. (c) The specimen was sequestrated with surrounding necrotic bone
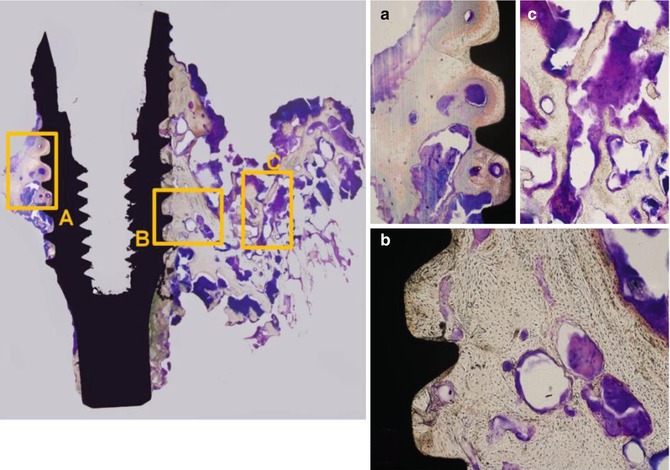
Fig. 17.2
Histological feature of the specimen from sequestrated bone-implant complex. (a, b) Osseointegration was maintained in some part of the implant surface. Microorganisms are dominantly infiltrating to exposed bone surface and not deeply to the implant-bone interface. (c) Abundant bacterial colony infiltrating the necrotic osseous structure at the outer side of the specimen. (Villanueva bone stain, × 100) (Figs. 17.1 and 17.2: Courtesy of Tae-Geon Kwon, DDS, PhD, Professor, Department of Oral & Maxillofacial Surgery, School of Dentistry, Kyungpook National University, Samduck 2 Ga, Jung Gu, Daegu, 700-412, Korea, E-mail: kwondk@knu.ac.kr)
Implants in Rehabilitation After MRONJ
MRONJ has a significant impact on quality of life and a big part of this is caused by bad oral conditions like eating discomfort, lack of self-consciousness, and mucosal irritability [43]. MRONJ itself often leads to relevant destruction of the jaw bone (Fig. 17.3), and surgical treatment of the disease regularly sacrifices parts of the jaw bone, additionally (Fig. 17.4). While surgical protocols to treat MRONJ seem to assimilate as they lead to curing in the majority of cases (see treatment chapter), bony reconstruction is problematic, as MRONJ can affect transferred bone [44] like it does in the jaw bone. As well as, there is lack of protocols for rehabilitation after MRONJ: Dentures should be very stable, because denture sores can trigger MRONJ [45]. But often in these patients, teeth and jaw bone loss leads to conditions where dentures cannot be fit in a sufficient manner (Fig. 17.5). Implants can immobilize dentures perfectly, but a history of MRONJ is a risk factor of relevant and highly debated impact, which excludes these patients from implantology, when regarding the AAOMS recommendations [8]. Consequently, leaving patients without dental prosthodontic rehabilitation is a recommendation given [46]. In the last years, the point of view changed from oral surgery as a true risk factor for MRONJ to the idea of oral surgery as a possible trigger of infection and acidic milieu, which then starts the cascade for MRONJ [47]. While still under debate [15, 48], some evidence for successful implant therapy in patients on oral bisphosphonate medication also came up in the recent literature.
Fig. 17.3
Large BRONJ defect in the anterior mandible of a 73-year-old female with a 5-year oral bisphosphonate medication on osteopenia
Fig. 17.4
Defect after surgical debridement and plating of pathological fracture
In the author’s opinion, surgeons should use implants as a means of oral rehabilitation in selected cases and under control for other risk factors: In a 73-year-old female, which was on oral bisphosphonates for 5 years, MRONJ and MRONJ-induced pathological fractures were treated (Figs. 17.3, 17.4, and 17.5). After MRONJ was cured, implants were inserted (Fig. 17.6) and a bar-retained removable prosthesis was inserted (Fig. 17.7). The patient is on high-frequency recall and without any clinical or radiographical signs of infection (Figs. 17.8 and 17.9). The experience of other authors is consistent with this opinion [41], but of course, there is still lack of data on the topic.

Fig. 17.6
Insertion of four dental implants, four months after fracture plating
Fig. 17.7
Bar retainers, nine months after insertion, 13 months after implant insertion

Fig. 17.8
Healthy conditions at 24-month follow-up exam
Fig. 17.9
Panoramic x-ray at 24-month follow-up exam showing no signs of inflammation, sequestration, or bone loss
Excursus: Antiresorptive Coatings of Dental Implants
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses



