Mechanism of action
Desensitising agents
Nerve desensitisation
Potassium nitrate, chloride, citrate, oxalate,
Protein precipitation
Glutaraldehyde, silver nitrate, zinc chloride, strontium chloride hexahydrate
Tubule occlusion
Stannous and sodium fluoride
Strontium chloride
Ferric oxalate
Potassium oxalate
Amorphous calcium phosphate
Calcium phosphate
Calcium carbonate
Calcium hydroxide
Calcium sodium phosphosilicate
Tricalcium phosphate (TCP)
Dental varnish (Clinpro™ 3M™ ESPE™) containing 5 % sodium fluoride with tricalcium phosphate (TCP)
Prophylaxis polishing paste containing 1.23 % fluoride
Prophylaxis polishing paste containing 1.1 % sodium fluoride +5 % NovaMin
Sensodyne NUPRO (NovaMin® – Dentsply)
1.1 % Sodium fluoride anticavity toothpaste (Clinpro™ 3M™ ESPE™ 5000)
Vanish™ XT Extended Contact Varnish (light-cured resin-modified glass ionomer (RMGI) based on the patented methacrylate-modified polyalkenoic acid)
Bioactive glasses (SiO2–P2O5–CaO–Na2O)
Aluminium
Gingival surgery – recovering the exposed dentin area
Neural action and tubules occlusion
Laser
Neodymium-doped yttrium aluminium garnet (Nd:YAG), laser GaAlAs (gallium-aluminium-arsenide laser), erbium-YAG laser
Anti-inflammatory effect
Homeopathic medication – propolis
Corticoid steroids
Covering the dentin surface
Tooth restoration
Periodontal surgery
Current Therapies for Dentin Hypersensitivity (DH)
Currently, many of the dentin desensitisers that have been used in treating DH have supported evidence from in vitro, in situ or in vivo studies (Orchardson and Gillam 2006). The mechanism of action for the majority of the desensitising agents in these studies was by tubule occlusion. There are however a number of problems with the application of both in-office and OTC/at-home products in that the tubular occlusion was not permanent in nature, particularly following the impact of an acid challenge to the surface deposit (see Chap. 6). Furthermore the resin or toothpaste precipitate in the dentin tubule may only provide a chemical-physical blockage rather than induce the initiation of new dentin (Calabria et al. 2012). Ideally a bioactive/biomimetic material able to modify its composition and/or induce the precipitation of insoluble fluorapatite would be a major advantage in the treatment of DH (see Chap. 6). According to Orchardson and Gillam (2006), the management of DH should be based on a stepwise approach based on the extent and severity of the condition. An inherent component of this approach was the importance of the removal of any aetiological or predisposing factors, counselling the patient with regard to dietary intake (e.g. excessive consumption of acidic drinks) and toothbrushing techniques and appropriate monitoring by the clinician (see Chap. 10). A more recent UK Guidelines publication on the management of DH by Gillam et al. (2013) also stressed the importance of not using a single treatment philosophy to treat DH but recommended management strategies based on the aetiology and predisposing factors of specific presenting conditions, namely, (1) patients with good oral hygiene associated with DH, (2) patients with toothwear and associated DH and (3) periodontally related DH together with an awareness of the potential impact of DH on the patient’s quality of life (see Chaps. 9 and 10).
In-Office (Professionally Applied) Treatment
Following a successful diagnosis of DH, the clinician will base the treatment on the extent and severity of the condition. For example, where the problem is mild to moderate in nature (see Chap. 5), then an OTC/at-home approach may be initiated with the caveat that if the pain does not resolve before the next appointment (or if this approach was ineffective), then the patient may return for a more invasive in-office (professionally applied) procedure. If the pain is localised to one or two teeth and is severe in nature, the clinician may opt for an in-office procedure using one of the restorative materials as suggested by Pashley (2000). There is a tendency however to apply an in-office treatment following several attempts to resolve the patient’s pain following the unsuccessful use of an OTC/at-home product. There are however a vast array of desensitising products currently available which may make the choice of the most appropriate product both confusing and difficult for the clinician (Cunha-Cruz et al. 2010).
Fluoride Application
According to Cummins (2010), fluoride in the form of gels, varnishes and resins has been recommended for an in-office treatment for DH (Gaffar 1999; Orchardson and Gillam 2006; Ritter et al. 2006; Merika et al. 2006; Hoang-Dao et al. 2008; Yilmaz et al. 2011; Trushkowsky and Oquendo 2011; Petersson 2013). High-level fluoride-based desensitisers (solutions, gels and varnishes) have also been reported to provide an instant and relative long-term relief of DH (Al-Sabbagh et al. 2009; Gaffar 1999; Ozen et al. 2009; Petersson 2013; Pradeep et al. 2012; Ritter et al. 2006; Schmidlin and Sahrmann 2013). For example, a single topical application was reported to relieve DH for 3–6 months (Al-Sabbagh et al. 2009; Glockner 2013; Ritter et al. 2006). The combined use of fluoride with iontophoresis has also been reported in the literature (Gangarosa and Park 1978; Brough et al. 1985; Gangarosa 1994; Singal et al. 2005; Gupta et al. 2010; Aparna et al. 2010; da Rosa et al. 2013; Patel and Langalia 2014); however, the clinical effectiveness of this technique (with or without fluoride) has been questioned (Gillam and Newman 1990; Pashley 2000). The mode of action of topically applied fluorides is by tubule occlusion in the form of calcium fluoride (Table 8.1) although the resultant layer is generally not resistant to the frequent acid challenges in the oral environment, resulting in reapplication in order to maintain any efficacy (Cummins 2010; Calabria et al. 2012). Fluoride compounds however have been reported to demonstrate low permeability values in vitro in laboratory studies, which may suggest that the transient effect in reducing DH observed in clinical trials may be as a result of the other properties of the varnish rather than the physical precipitation of crystals inside the dentin tubules. A combination approach using a fluoride mouthrinse has also been recommended by several investigators (Glockner 2013; Marinho et al. 2004). Although currently there does not appear to be a systematic review exclusively addressing the role of professionally applied fluoride varnishes in DH in randomised clinical trials (Ozen et al. 2009; Sharif et al. 2013; Thrash et al. 1994), there was some evidence reported in the published literature that indicated that professionally applied fluoride varnishes were effected in relieving pain associated with DH (Orchardson and Gillam 2006; Sharif et al. 2013).
Potassium Salts
Potassium salts have also been used for the treatment of DH (Hodosh 1974; Pereira et al. 2005; Sauro et al. 2006; Cummins 2010) and have been reported to react with the exposed dentin section with a precipitation of calcium compound crystals onto the dentin surface and sub-superficially into the dentin tubules to effectively occlude the dentin tubules (Pereira et al. 2005; Calabria et al. 2012; Cummins 2010; Markowitz and Pashley 2008) (see Chap. 2). Potassium has also been combined with an oxalate formulation (Cunha-Cruz et al. 2011). Three types of oxalate formulations (6 % ferric, 30 % dipotassium and 3 % monohydrogen monopotassium) have also been classically indicated to occlude the dentin tubules and reduce DH (Al-Sabbagh et al. 2009; Pashley et al. 1987, 2001; Schmidlin and Sahrmann 2013). For example, 3 % Potassium oxalate solutions have been used to treat DH, and the resultant oxalate crystals have been reported to be more resistant to an acid challenge compared to the precipitated fluoride crystals (Pereira et al. 2005; Calabria et al. 2012). The in vitro testing of desensitising agents has been traditionally through the observation of the surface and subsurface of the dentin tubules using a number of techniques, for example, SEM scanning electron microscopy and CLSM confocal laser scanning microscopy, and comparing images before and after conditioning and treatment application (Fig. 8.1a, b) (see Chap. 6). By comparing the images of potassium oxalate-treated dentin before and after an acid challenge (Figs. 8.2b and 8.3a), one can observe the greater precipitation of crystals inside the dentin tubules following an acid challenge. This observation may also be seen with other formulations based on crystal precipitation, except for fluorophosphates.
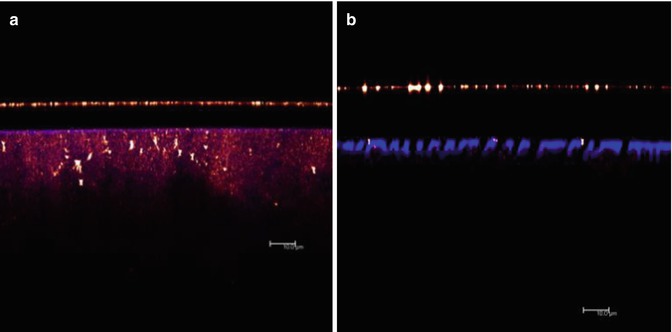
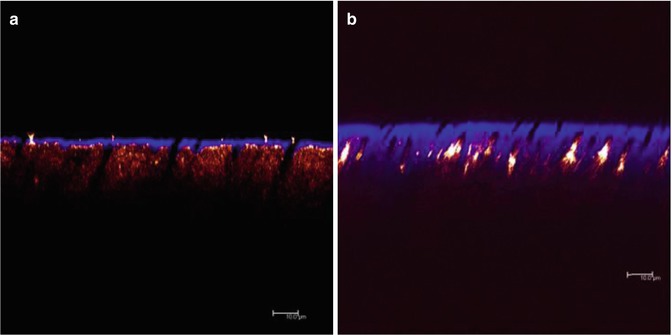
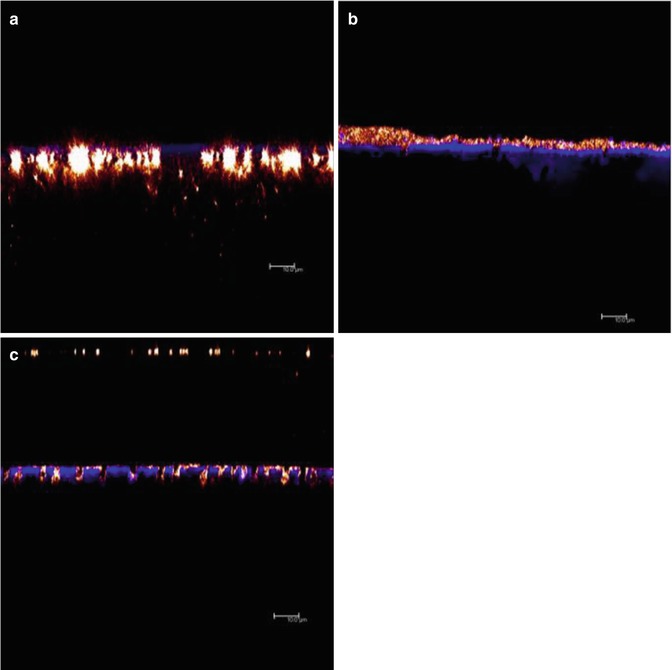
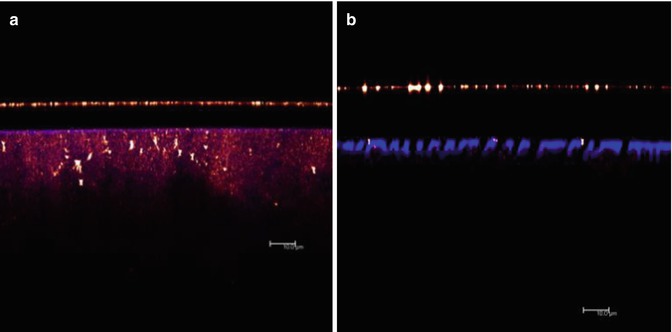
Fig. 8.1
Confocal laser scanning microscopy (CLSM, XZ axis) of mineralised sound dentin. (a) and after dentin conditioning with phosphoric acid (b)
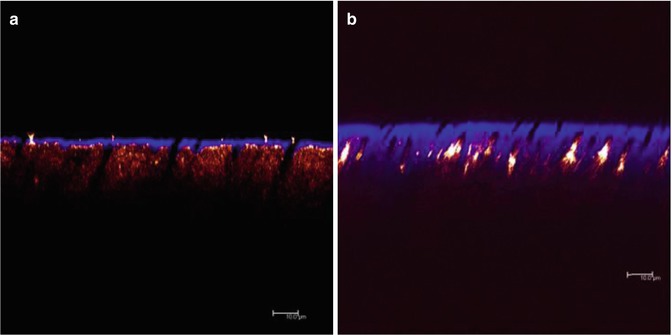
Fig. 8.2
Confocal laser scanning microscopy (CLSM, XZ axis) of demineralised dentin (a) treated with 1.23 % acidulated fluorophosphate (APF) (b) and 3 % potassium oxalate (KOx). Reflexive deposits can be seen inside dentin tubules of the specimen treated with KOx; in the APF specimen reflexive particles appear infiltrated in the body of intertubular dentin, similar to untreated dentin in Fig. 8.1a
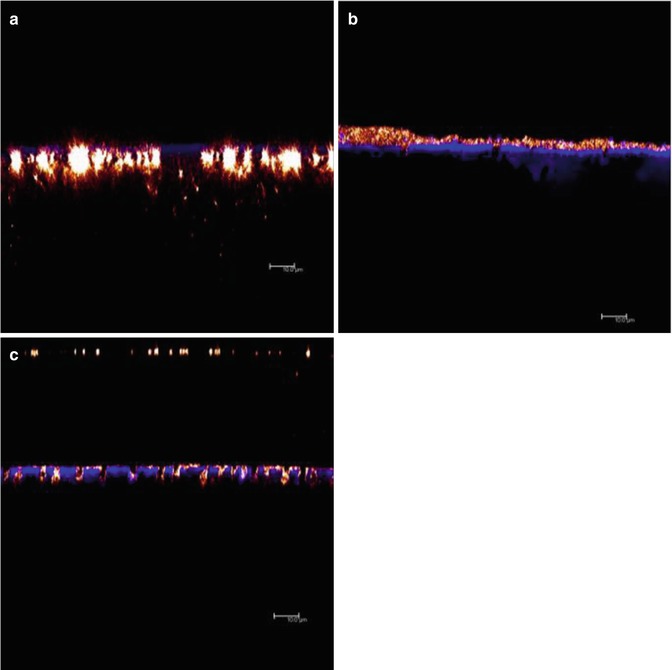
Fig. 8.3
CLSM XZ axis images of specimens before and after acid challenge. (a) Compared with Fig. 8.2b, the specimens treated with KOx challenged with citric acid show greater concentration of crystals inside the dentin tubules. (b) Specimen treated with Desensibilize NanoP® with clusters of crystals on dentin surface. (c) Specimen also treated with Desensibilize NanoP® shows crystals displaced into the dentin tubules after an acid challenge
Several investigators have reported that any relief from DH may be transient in nature as the precipitated crystals may be dissolved or removed over time (Al-Sabbagh et al. 2009; Cooley and Sandoval 1989; Kerns et al. 1991; Knight et al. 1993). According to Al-Sabbagh et al. (2009), oxalate-containing phytocomplexes however may be an alternative to the traditional oxalate preparations. For example, Sauro et al. (2006) reported that these complexes reduced dentin permeability following a single application in an in vitro study. These investigators also postulated that these complexes may protect the smear layer formed by scaling procedures on the root dentin from an acid challenge (Sauro et al. 2007).
A number of reviews recognised that, with the possible exception of the 3 % monohydrate monopotassium, oxalate preparations were not considered to be effective desensitising products based on evidence-based clinical criteria (Al-Sabbagh et al. 2009; Cunha-Cruz et al. 2011; Gillam et al. 1997; Orchardson and Gillam 2000; Schmidlin and Sahrmann 2013; Sharif et al. 2013).
Calcium Phosphate Compounds
Currently there appears to be limited data on the clinical effectiveness of calcium compounds in reducing DH although calcium hydroxide has been reported to immediately reduce DH in over 90 % of treated teeth in clinical studies (Al-Sabbagh et al. 2009; Levin et al. 1973). Calcium phosphate has also been reported in in vitro studies to be more effective than potassium oxalate in occluding the dentin tubules (Al-Sabbagh et al. 2009; Suge et al. 2005).
Recently, nano-hydroxyapatite-based agents (e.g. Desensibilize NanoP® and Clinpro white varnish [Clinpro]) with bioactive and biocompatibility potential have been reported to be effective both as a remineralising and desensitising agent (Calabria et al. 2012; Hanning and Hanning 2010; Tschoppe et al. 2011). These agents contain nano-sized particles, which act in a similar manner to dental apatite in regard to their morphology, structure and crystallinity arrangement (Vandiver et al. 2005). These novel approaches were based on technology that explored the bioactivation with natural compounds with a view to improve the stability of the surface precipitate on the tooth surface following an acid challenge (Fig. 8.3). These images are consistent with the results of dentin permeability following dentin treatment with both potassium oxalate and Desensibilize NanoP®-FGM (Calabria et al. 2012).
One of the problems, however, with most of the products utilising an occlusive strategy was that the precipitate was unable to withstand the continual impact of the acid challenge in the oral environment. This issue has subsequently led investigators to develop innovative bioactive formulations to enhance the remineralising or tubule-occluding properties of the marketed products (Cummins 2010; Markowitz and Pashley 2008; Reynolds 1997; Reynolds et al. 2008; Rusin et al. 2010; Calabria et al. 2012; Nongonierma and Fitzgerald 2012; Pei et al. 2013) (see Chap. 6).
Casein phosphopeptide-amorphous calcium phosphate (CPP-ACP), a milk derivative, has also been reported to be effective in remineralising enamel and dentin (Reynolds 1997; Kumar et al. 2008; Reynolds et al. 2008; Agnihotri et al. 2012; Nongonierma and Fitzgerald 2012). CPP is a bioactive peptide released from caseins, which has been shown to enhance bivalent mineral solubility and also optimise binding ability to minerals, as calcium. Amorphous calcium phosphate (ACP) is the precursor of hydroxyapatite and in an oral environment in the presence of saliva was converted to hydroxyapatite. At the tooth surface interface, both calcium and phosphate are able to precipitate as stable hydroxyapatite (Nongonierma and Fitzgerald 2012). According to investigators, however, the effectiveness of ACP was only comparable to that of a placebo after approximately 3 months (Al-Sabbagh et al. 2009; Yates et al. 1998). According to Reynolds et al. (2008), CPP-ACP may also be successfully incorporated into commercial toothpaste products for the treatment of DH to enhance the occlusion of the dentin tubules through ‘remineralised dentin’ technology.
A number of recent products containing tricalcium phosphate (TCP) has been recently developed for the dental market (3M™ ESPE™ St Pauls Minneapolis, USA), namely, (1) a dental varnish (Clinpro™ 3M™ ESPE™) containing 5 % sodium fluoride with tricalcium phosphate (TCP), (2) a prophylaxis polishing paste containing 1.23 % fluoride, (3) prescription toothpaste 1.1 % sodium fluoride anticavity toothpaste (Clinpro™ 5000) and (4) Vanish™ XT Extended Contact Varnish, which is a light-cured resin-modified glass ionomer (RMGI) based on the patented methacrylate-modified polyalkenoic acid. The indications for use are based on remineralising of the enamel and blocking the open dentin tubules (tubule occlusion) (Vanichvatana and Auychai 2013; Asaizumi et al. 2013).
Several investigators have, however, reported conflicting results when comparing either an ACP (Schemehorn et al. 2011) or an MI Varnish with RECALDENT™ containing CPP-ACP (Cochrane et al. 2014) with 5 % ACP with TCP or CPP-ACP with a functionalised tricalcium phosphate (fTCP). According to these investigators, varnish ACP and MI Varnish had the highest release of calcium and fluoride ions compared to the TCP varnish.
Other calcium-containing desensitisers designed for in-office use are formulations containing arginine and calcium carbonate. These formulations have been reported to effectively occlude the dentin tubules and to provide immediate and lasting relief for DH (Pei et al. 2013; Hamlin et al. 2009; Schiff et al. 2009). According to the manufacturers, arginine is an amino acid naturally available in saliva, which presents a positive charge. Since dentin is negatively charged, arginine may play an important role, in association with calcium, favouring its deposition on the dentin surface. This mechanism is attributed to the deposition of an arginine, calcium carbonate and phosphate complex that physically occlude the dentin tubules and was resistant to normal pulpal pressures and to an acid challenge (Cummins 2010; Hamlin et al. 2009; Schiff et al. 2009; Pei et al. 2013). Pro-Argin™ technology is currently available as an in-office and as an OTC/at-home toothpaste that can be used in association with in-office treatment, for example, scaling and polishing procedures (Hamlin et al. 2009). According to Calabria et al. (2012), there is evidence from CLSM techniques that polishing with a Pro-Argin™ prophylaxis paste was effective in depositing these crystals in covering the dentin surface and occluding the subsurface of the dentin (Fig. 8.4a). Arginine-based products have also been reported to promote relief of DH compared to a negative control in clinical studies (Kapferer et al. 2013). However, there is some concern that these formulations are not able to resist to an acid challenge, as shown in Fig. 8.4b.
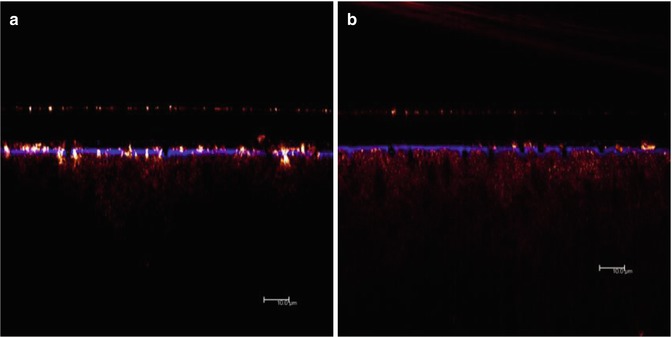
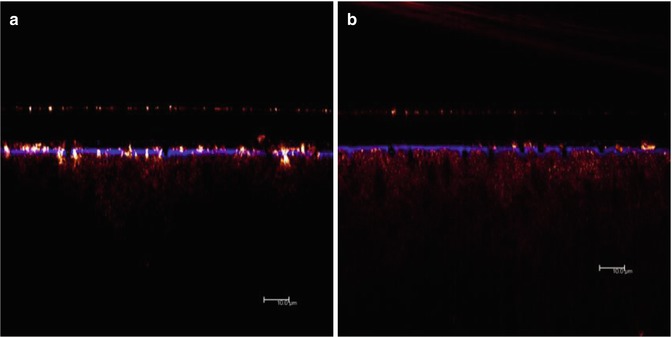
Fig. 8.4
CLSM XZ axis of dentin specimens treated with Pro-Argin™ before (a) and following an acid challenge (b)
Calcium Sodium Phosphosilicate (Bioactive Glass)
Calcium sodium phosphosilicate, for example, NovaMin®, based on the original 45S5 Bioglass® formulation by Larry Hench (2006) was previously used for as a synthetic bone grafting material (PerioGlas®) (US Biomaterials Corp., Jacksonville, FL, USA; now NovaBone®). According to the manufacturer, a bioactive glass material (e.g. NovaBone) has the ability to release Si, Ca and phosphate ions and initiate the upregulation and activation of a family of genes in osteoprogenitor cells, a process defined as osteostimulation (Price et al. 1997; Xynos et al. 2000; Loty et al. 2001; Sollazzo et al. 2010). Both PerioGlas and NovaBone products have been reported to be effective as a synthetic bone graft material in a number of dental indications, for example, in periodontal intrabony defects (Zamet et al. 1997; Park et al. 2001; Sculean et al. 2002), bone regenerative procedures (Yukna et al. 2001), bone augmentation prior to implant placement (Norton and Wilson 2001), furcation defects (Anderegg et al. 1999; Giusto 2005) and extraction sockets (Kates et al. 1998). The original 45S5 Bioglass® formulation was later adapted for use in toothpaste formulations and prophylaxis polishing pastes for the treatment of DH (NovaMin Technology Inc., Alachua, FL, USA; now GSK). According to Lynch et al. (2012), the proposed mode of action for both the toothpaste and the polishing paste was considered to be through the precipitating of hydroxycarbonate apatite (HCA) onto the dentin surface and subsequently occluding the dentin tubules.
In-office prophylaxis pastes containing both arginine/calcium carbonate and bioactive glasses (e.g. calcium sodium phosphosilicate) have subsequently been reported to provide effective clinical pain relief from DH following application (Cummins 2010; Gendreau et al. 2011; Hughes et al. 2010; Pradeep et al. 2012; Pradeep and Sharma 2010). According to Sharif et al. (2013), however, there is currently insufficient evidence on its clinical efficacy in reducing DH following in-office procedures.
Dentin Bonding Agents/Adhesives and Adhesive Restorations
The application of dentin adhesive materials for relieving DH has been also reported by several investigators (Bruton et al. 2000; Mehta et al. 2014). Previous adhesive systems were based on the application of phosphoric acid to promote the interlocking of the resin material to the dentin surface. However, the need of an acidic dentin conditioning before the application of an adhesive may theoretically increase pulpal sensitivity. Although there were concerns that these organic matrix-enriched materials may fail to resist the repeated impact of an acid challenge in the oral environment, a number of glutaraldehyde-based agents (e.g. Gluma Desensitizer™) have been historically indicated for DH treatment (Schmidlin and Sahrmann 2013; Vora et al. 2012). Although the concern about its biocompatibility still persists, there is evidence of its effectiveness in treating DH (Orchardson and Gillam 2006; Schmidlin and Sahrmann 2013; Vora et al. 2012). The introduction of self-etching agents, however, has reactivated interest in applying these adhesive systems as dentin desensitisers. According to Pei et al. (2013), these products are relatively easy to apply and appear to be less aggressive to the dentin-pulp complex than the other etch-and-rinse systems. These agents also have been reported to promote a micro-mechanical interlocking through a hybridisation process, but due to the presence of functional monomers in mild self-etch adhesives, they have the potential to interact chemically with the calcium ions from the residual hydroxyapatite that remains available within the submicron hybrid layer (Pei et al. 2013; Inoue et al. 2005). The functional monomers may also interact with the calcium ions from the smear layer, potentially resulting in additional chemical bonding.
The long-lasting effectiveness of any kind of adhesive system as a dentin desensitiser, for example, the self-etching adhesives, alone or in association with restorative materials, however, remains unclear. For example, it is recognised that dentin in a non-carious lesion is hypermineralised, and theoretically this may be an obstacle to dentin hybridisation. However any superficial layer of any type of material on the exposed dentin may not be able to resist to any outward fluid movement. According to Francisconi et al. (2009), the tooth may be subjected to significant stress concentration at the cervical region during either mastication or during toothbrushing which may present a challenge to the ability of an adhesive material to resist these forces. Although a strong interaction with the dentin substrate and the occlusion of the dentin tubules are mandatory for a long-lasting protective effect of the exposed dentin by a desensitising agent, this does not appear to occur on the exposed dentin of a cervical non-carious lesion. As illustrated in Fig. 8.5b, the hybrid layer is barely seen, and the resin tags only superficially penetrate the tubule openings in a dentin specimen from a non-carious cervical lesion. In Fig. 8.5a, however, in a sound cervical young dentin specimen, there was the presence of long resin tags and a well-defined hybrid layer (Calabria et al. 2010).
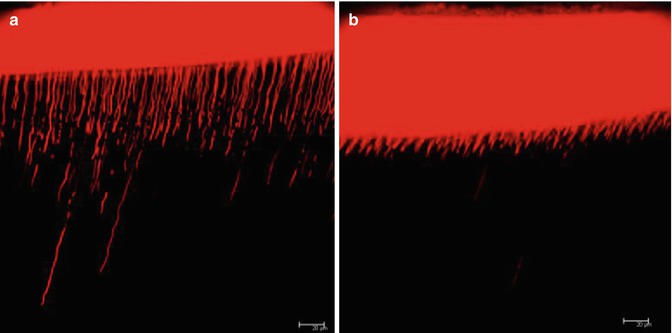
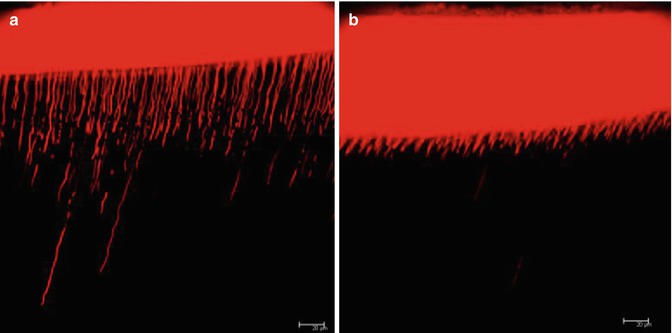
Fig. 8.5
CLSM images from sound cervical young dentin (a) and from a non-carious cervical lesion (b)
Adhesives may also be indicated for severe cases of DH that failed to respond to the other treatment modalities (Al-Sabbagh et al. 2009; Glockner 2013; Schmidlin and Sahrmann 2013; Swift et al. 2001). It is evident from the published literature that there is a vast array of products claiming to be effective in reducing DH. For example, dentin bonding agents (e.g. Scotchbond, Gluma Desensitizer, etc.) have been reported to be effective in reducing DH for up to 18 months post application (Al-Sabbagh et al. 2009; Brahmbhatt et al. 2012; Copeland 1985; Dondidall’Orologio et al. 1999; Ianzano et al. 1993; Kakaboura et al. 2005; Sharif et al. 2013; Schüpbach et al. 1997; Sethna et al. 2011; Yu et al. 2010). According to several investigators, however, the available in vitro and well-conducted clinical studies have provided only limited data on the effectiveness of these products (Al-Sabbagh et al. 2009; Sharif et al. 2013; Tay et al. 1994). A further problem with some of these products is the lack of a filler material which may possibly favour wear from the surface of the material (Schmidlin and Sahrmann 2013).
Glutaraldehyde-based products have also been reported to reduce DH by protein precipitation, and these products have been reported to be effective in treating DH in the clinical environment (Duran et al. 2005; Glockner 2013; Kakaboura et al. 2005; Schmidlin and Sahrmann 2013; Schüpbach et al. 1997). Although several investigators have reported immediate pain relief to DH following application (Aranha et al. 2009; Lopes and Aranha 2013), reapplications are subsequently required in order to maintain the reduction of DH (Lopes et al. 2013). According to several investigators, however, there are biocompatibility hazards associated with these products that cannot be ignored (Arenholt-Bindslev et al. 1987; Schmidlin and Sahrmann 2013; Schweikl and Schmalz 1997). With respect to the glutaraldehyde-containing adhesives, several investigators have reported immediate and long-term relief of pain associated with DH (Dondidall’Orologio et al. 2002; Lopes and Aranha 2013; Qin et al. 2006; Schüpbach et al. 1997).
Although a minimal invasive approach is preferred when treating DH with restorative materials (Orchardson and Gillam 2006), the clinician may be confronted with significant loss of the tooth structure associated with DH which would require restoration of the tooth shape in order to maintain its aesthetic and function. In this situation, restorative intervention may be recommended using glass ionomer cement (GICs) and resin-based materials which are generally indicated when a more resilient material is desirable. For example, where a class V restoration is necessary, an adhesive restoration is a valid option (Schmidlin and Sahrmann 2013). Large and deep cervical non-carious lesions, regardless of the degree of pain, must be restored in order to recover dental anatomy and preserve health of gingival tissue. GICs or composite restorations have been used for these purposes, but evidences supporting their success is weak (Al-Sabbagh et al. 2009; Polderman and Frencken 2007). Several investigators have also used GICs in association with periodontal procedures, including root coverage procedures, where it has been reported that the placement of a GIC may favour the attachment of the periodontal fibres and release fluoride (Tantbirojn et al. 2006; Polderman and Frencken 2007; van Dijken and Pallesen 2008; Francisconi et al. 2009; Santos 2014)
Laser Technology
According to a number of investigators (Al-Sabbagh et al. 2009; Kimura et al. 2000; Moritz et al. 1998; Schmidlin and Sahrman 2013; Bader et al. 2014), the clinical effectiveness of laser technology (e.g. Er:YAG, Er, Cr:YSGG, CO2, GaALAS and low-level diode) in treating DH ranged from 5.2 to 100 %, depending on the laser type and parameters used in the clinical studies. For example, an Nd:YAG laser has been reported to minimise discomfort immediately following application (Al-Sabbagh et al. 2009; Kara and Orbak 2009; Lan and Liu 1996; Liu et al. 1997; Lopes and Aranha 2013). Furthermore, according to Lin et al. (2013), a Nd:YAG laser may also have a supplementary analgesic effect when compared with the other high-power lasers. The clinical efficacy of GaAlAs laser has been reported to be based on tubule occlusion and possibly by interrupting neural transmission (Tengrungsun and Sangkla 2008), but this reported success may be less evident than that reported by the application of a dentin bonding agent. The long-term effectiveness of lasers compared to the other types of treatment approaches has also been favourably reported (Aranha et al. 2005; Birang et al. 2007; Gholami et al. 2011; Kara and Orbak 2009; Lopes and Aranha 2013). However, the reported clinical effectiveness of lasers in the treatment of DH has also been challenged by Schmidlin and Sahrmann (2013) and Sgolastra et al. (2011). According to several investigators, there were no significant reductions in DH in comparison to the other types of laser and placebo therapies (Al-Sabbagh et al. 2009; Lier et al. 2002; Martens 2013). Furthermore, lasers in general are less effective in cases of severe DH (Al-Sabbagh et al. 2009; Kimura et al. 2000). There do not however appear to be any major adverse effects when using lasers if they are used in accordance with the manufacturers’ instructions (Lopes and Aranha 2013).
The mechanisms involved in the laser treatment of DH are relatively unknown (Kimura et al. 2000). The mechanism of the high potency laser devices appears to promote the closure of the exposed dentin tubules, primarily, by producing a melting effect of the dentin. According to Bader (2014), there appears to be a degree of uncertainty as to whether there is also a synergic effect if lasers are combined with other occlusive pretreatments, which, in turn, may help to promote a more stable layer to obliterate the dentin tubules. The low-potency laser has been reported to diminish the neural response to hypersensitive stimuli (Bader et al. 2014), although there does not appear to be any strong evidence to support the use of laser therapy for this purpose due, in part, to the lack of consensus of the type of laser and the parameters that should be incorporated into standardised and efficient protocols.
Combined Treatment of Lasers with Other Treatment Approaches
The combination of techniques (e.g. laser technology with a fluoride varnish) may also be a strategy in the treatment of DH. The rationale for this approach is the association of the combined effects, which may result in significant better outcomes (Duran and Sengun 2004; Erdemir et al. 2010; Ipci et al. 2009; Lin et al. 2013; Lopes and Aranha 2013). Dentin desensitisers with an occluding potential may be used in association with low-level lasers in order to simultaneously block the dentin tubules and decrease the level of neural stimulation which may in turn initiate the formation of tertiary dentin (Farmakis et al. 2012; Lopes and Aranha 2013; Lopes et al. 2013). A similar indication of this combined use has been in the recommendation of an OTC product (e.g. toothpaste) following an in-office treatment (Rösing et al. 2009).
Although the evidence from both randomised controlled trials and systematic reviews supports the clinical use of lasers in treating DH (Deng et al. 2011; He et al. 2011; Sharif et al. 2013), further well-conducted studies with appropriate clinical protocols comparing the use of both low or high frequencies and any association with the other alternatives discussed for treating DH should be implemented (Al-Sabbagh et al. 2009; Ipci et al. 2009; Petersson 2013; Schmidlin and Sahrmann 2013).
Other Restorative-Based Procedures
Periodontal Plastic Surgery (Root Coverage Procedures)
Periodontal disease may lead to changes in the periodontal tissues, and the consequent recession of the marginal tissues (gingival recession) has been reported to be associated with DH as a result of the exposure of the root surface to the oral environment. Both nonsurgical and surgical periodontal procedures together with the effects of periodontal disease on the teeth and their supporting structures may also impact on the patient’s aesthetics and quality of life due to the pain associated with DH (see Chap. 3). The clinician should be aware of the various etiological and precipitating factors associated with gingival recession (e.g. anatomical, plaque, restorative procedures, patient habits, smoking, etc.) (see also Chap. 4). Furthermore the clinician should also consider how to manage both the patient’s and his/her own expectation when proposing a treatment plan for resolving the problem of the aesthetics associated with gingival recession (e.g. posttreatment, presence of the so-called black triangles, etc.) (Fig. 8.6).
Fig. 8.6
Clinical photograph of patient with so-called black triangles which may cause aesthetic concerns
This may present a problem if both the perception and expectations expressed by the patient are either ignored or not met (by the clinician) to their satisfaction. Root coverage procedures associated with root scaling and the covering of the exposed root through periodontal surgical procedures have been reported to reduce or completely abolish DH over time (Orchardson and Gillam 2006; Lin and Gillam 2012). According to Douglas de Oliveira et al. (2013a), root coverage procedures (both partial and complete coverage) have been reported to decrease pain and improve a patient’s quality of life although currently there appears to be insufficient scientific evidence to associate root coverage procedures with the complete suppression of DH (Douglas de Oliveira et al. 2013b).
As indicated above, gingival recession may also occur in the healthy tissues and has been related to a combination of anatomical and physiological aspects of each individual tooth. For example, gingival recession was more often observed on the buccal surfaces compared with other surfaces of the teeth as a result of anatomical factors. According to Kassab and Cohen (2003), more than 50 % of the population in their study had at least one or more sites with gingival recession of 1 mm or more (see Chap. 3).
Gingival recession may be also associated with the periodontal biotype, and the analysis of this factor is essential for the planning of surgical procedures for root coverage. Three different periodontal biotypes have been described in the published literature, namely, the thin scalloped, the thick flat and the thick scalloped (Seibert and Lindhe 1989; Zweers et al. 2014). The teeth in the thin scalloped category have the characteristics of a thin gingival tissue with a more pronounced contour of the gingival margin, with a greater height of the interproximal papilla and with an underlying thin buccal bone that can present with fenestrations. The thick biotype category is characterised by thicker bone tissue surrounding the teeth and covered by a thick and smooth contour gingival tissue, which results in a small height of the papilla. The thick scalloped category displays the characteristics of the two other patterns (Fig. 8.7a–c).


Fig. 8.7
Clinical pictures of (a) normal, (b) thin and (c) thick gingival biotypes
It is important for the clinician to have sufficient knowledge of the relevant characteristics of each of the biotypes, both in health and disease, particularly when planning root coverage procedures, as the different biotypes may respond differently both during the surgery and, subsequently, in the wound healing process. For example, thin biotypes may tear easily during probing and surgical intervention and root coverage may not be optimum, whereas in a thick biotype, the thickness of the flap may be related to a higher mean gain of complete root coverage (Seibert and Lindhe 1989; Müller et al. 2000; Hwang and Wang 2006). Due to the higher incidence of gingival recession in the thin biotype, the aim of the planned surgical procedures should not only consider the root coverage aspect but also the resultant aesthetics together with the treatment of DH (Ahmedbeyli et al. 2014; Cairo et al. 2014; Polack and Mahn 2013; West et al. 2013).
According to Gillam (2014), several classifications for treating gingival recession have been recommended in order for the clinician to facilitate both a diagnosis and a template for the correction of gingival recession defects. One of the classifications that has been favoured over the last three decades is the Miller classification system ([I–IV] (Miller 1985) (Table 8.2, Fig. 8.8a, b) which enabled the clinician to predict successful outcomes of the surgical procedure based on type of defect, taking into account the anatomical features. A number of materials and techniques have been reported in the published literature, and these include guided tissue regeneration (GTR), coronally advanced flap and Emdogain (CAF + EMD), connective tissue graft (CTG) and free gingival graft (acellular dermal matrix allograft/Mucograft ADM) (Gillam 2014) (Fig. 8.9).
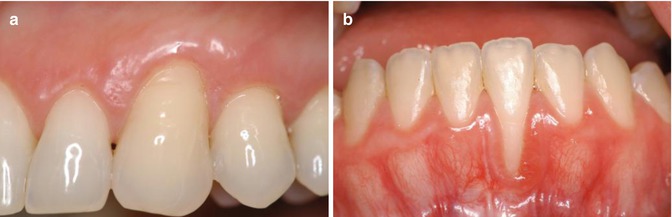
Table 8.2
Miller’s classification of gingival recession (GR)
|
Classification
|
Criteria
|
|---|---|
|
Class I
|
Marginal tissue recession that does not extend to the mucogingival junction (MGJ) with no interproximal tissue
|
|
Class II
|
Marginal tissue recession that extends to or beyond the MGJ, with no periodontal attachment loss (bone or soft tissue) in the interdental area
|
|
Class III
|
Marginal tissue recession that extends to or beyond the MGJ with periodontal attachment loss in the interdental area or malpositioning of teeth
|
|
Class IV
|
Marginal tissue recession that extends to or beyond the MGJ with severe bone or soft tissue loss in the interdental area, to a level apically to the buccal/labial soft tissue margin and/or severe malpositioned teeth
|
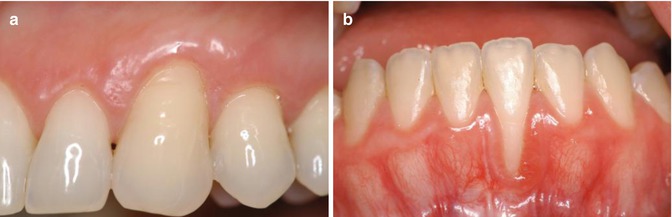
Fig. 8.8
(a, b) Examples of a Miller’ Class I (a) and Class II marginal defect (b)
Fig. 8.9
(a, b) Example of a root coverage procedure using free gingival and connective tissue grafts (a) pretreatment and (b) posttreatment connective tissue graft: Acknowledgement for [Courtesy of D. Chatzapoulou]
Irrespective of the surgical procedures, associated techniques, flap design or materials, the desired outcome for treating gingival recession defects is that the resulting gingival tissue covering the root surface must have the characteristics of a thick keratinised mucosa that will enable optimum plaque control without any change in the graft’s position (e.g. apical direction). When the root coverage along with an increase in thickness is desired, a systematic review of studies indicates an association of repositioned flap with subepithelial connective tissue graft as the best option, and this association can be considered as the gold standard surgery for root coverage (Chambrone et al. 2008).
Several investigators however have reported that in some patients, the clinician may not be able to treat the gingival recession defect by the conventional surgical root coverage procedures described above, and therefore, the remaining exposed root dentin may require a restorative approach, for example, the provision of a partial laminate porcelain veneer, composite material or glass ionomer or contouring of the defect with a finishing bur (Zalkind and Hochman 1997; Tugnait and Clerehugh 2001; Drisko 2002; Özgünaltay and Önen 2002; Santamaria et al. 2007). In patients where there has been extensive periodontal destruction resulting in open gingival embrasures (so-called black triangles), which may be aesthetically unacceptable for the patient (Sharma and Park 2010), a relatively simpler option to the techniques described above may be utilised, for example, a prosthetic gingival veneer (Greene 1998).
Gingival Augmentation
The various methods of soft tissue augmentation for root coverage procedures may also be an option depending on the condition of the hard and soft tissues (Al-Sabbagh et al. 2009; Chambrone et al. 2012; Schmidlin and Sahrmann 2013). According to Al-Sabbagh et al. (2009), however, there are limited clinical data to support this technique as part of a treatment approach in treating DH.
Over-the-Counter (OTC) Products
Individuals with mild to moderate local or generalised DH may decide to resolve any pain associated with DH without going to see a clinician by purchasing desensitising products that have been advertised in the media or through recommendation by a close friend or family member. According to Mantzourani and Sharma (2013), there are three main reasons that contribute to this behaviour: the need of a fast and urgent relief, the easy availability of these products in the market and their low cost, as this does not include the expenses of professional appointments and subsequent remedies. Desensitising products that are available through pharmacies or commercial outlets are called OTC or at-home care products in the form of toothpaste, gel or mouthrinse formulations. These OTC products are available without a medical prescription, but their indications for use are limited in that if the individual continues to have pain for longer than 2–4 weeks, they are advised to see a clinician. These OTC/at-home products may also be recommend by the clinician in association with in-office treatments (see Chap. 10), when the pain is associated with generalised DH, which is mild to moderate in severity.
OTC consumer products are generally based on formulations with the same active ingredients as for in-office products although the concentration permitted in OTC products may be considerably lower than those used by the clinician, for example, fluoride concentrations used in the office compared to fluoride concentrations used in OTC toothpastes. The constituents of these OTC products are usually formulated using a variety of salts (with different concentrations depending on whether the formulation is in a toothpaste, gel or mouthrinse) with the objective of reducing pain by dentin tubule occlusion or nerve desensitisation. Most of the OTC products available to the consumer are toothpaste products, although there is a number of mouthrinses currently available in the market. Although these rinses may deliver the therapeutic agent to all tooth surfaces in the oral cavity, one disadvantage would appear to be the necessity to deliver lower concentrations of a therapeutic agent in the mouthrinse compared to a toothpaste formulation (Markowitz 2013). The mechanism of action of the mouthrinses however is similar to a toothpaste formulation depending on the formulation used to deliver the therapeutic agent. Examples of these salts are potassium nitrate, potassium chloride, potassium citrate, sodium fluoride, strontium chloride, strontium acetate, dibasic sodium citrate, formaldehyde, sodium monofluorophosphate, stannous fluoride, amine fluoride, arginine, hydroxyapatite, calcium carbonate, calcium sodium phosphosilicate (bioactive glass) and amorphous calcium phosphate (Miglani et al. 2010; Orchardson and Gillam 2006; Karim and Gillam 2013; Talioti et al. 2014) (Table 8.3).
Table 8.3
Examples of selected toothpaste formulations for the treatment of DH available either on prescription or OTC
|
Mechanism of action
|
Commercial toothpaste (and mouthrinses)
|
Compounds
|
|---|---|---|
|
Dentin tubule occlusion
|
Colgate Sensitive Pro-Relief (Pro-Argin technology)
|
Calcium carbonate and arginine – an amino acid naturally found in saliva – 0.8 % arginine, PVM/MA copolymer, pyrophosphates and 0.05 % sodium fluoride in an alcohol-free base mouthwash
|
|
Sensodyne Repair and Protect (NovaMin® technology)
|
Fluoride, calcium and phosphate ions
|
|
|
Sensodyne Pronamel
|
Fluoride and potassium nitrate
|
|
|
Sensodyne Rapid Relief
|
8 % Strontium acetate in a silica base, 1,040 ppm sodium fluoride
|
|
|
SootheRx (NovaMin® technology)
|
Calcium sodium phosphosilicate (new hydroxyapatite)
|
|
|
AMFLOR (Pharmaceuticals)
|
3.85 % Amine fluoride
|
|
|
Clinician-prescribed fluoride toothpaste formulations
|
Fluoridex (Philips Oral Healthcare)
|
5,000 ppm Fluoride
|
|
Colgate Gel Kam Sensitive
|
Stannous fluoride 0.4 % w/w, 1,000 ppm F
|
|
|
Colgate Duraphat
|
2,800 ppm Fluoride
|
|
|
Neural desensitisation
|
Potassium-containing products
|
Potassium chloride, citrate, nitrate and oxalate and fluoride compounds
|
|
Dentin tubule occlusion and neural desensitisation
(other products)
|
Sensitive toothpaste (Himalaya herbals)
|
Spinach – natural oxalate compound
|
Fluoride-Containing Toothpaste, Gel or Mouthrinse Formulations
According to Cury and Tenuta (2014), fluoride is the most important therapeutic substance used in toothpaste products and may provide a reduction in dental caries and together with the other beneficial therapeutic substances incorporated into toothpastes (e.g. triclosan/copolymer or zinc) may also have additional benefits in reducing the dental biofilm, gingivitis, periodontitis, calculus formation and halitosis (malodour). Although conventional fluoride-containing toothpaste formulations have been suggested for the treatment of DH, there are limited data to support this claim (Orchardson and Gillam 2006; West 2008). Toothpaste and mouthrinse formulations containing sodium, stannous or amine fluoride (NaF, MFP, AmF and SnF2) have been used as OTC/at-home remedies to alleviate DH (Morris et al. 1999; Plagmann et al. 1997; Pradeep et al. 2012; Rösing et al. 2009). Nevertheless, inconsistent data are available on its clinical effectiveness (Pradeep et al. 2012). Earlier investigators acknowledged that fluoride containing toothpaste formulations may have a beneficial desensitising effect (Kanouse and Ash 1969; Orchardson and Gillam 2000) and in some studies provided similar results to those reported for the specific desensitising toothpaste formulations containing nerve desensitising or dentin tubule-occluding agents (Gillam et al. 1997; Orchardson and Gillam 2000; West et al. 1997). Several investigators have used fluoride-containing formulations in clinical trials as a placebo control rather a desensitising product per se, when evaluating desensitising products (Gillam et al. 1996 b; West et al. 1997; Yates et al. 2004; Pradeep et al. 2012; Rösing et al. 2009).
The mode of action of fluoride in anticariogenic, remineralising and DH strategies was based on its ability to react with hydroxyapatite and form fluorapatite, which was to be considered less susceptible to acid dissolution than hydroxyapatite due to its lower critical pH (Featherstone 2000). Calcium fluoride may also be deposited on the dentin surface when fluoride is incorporated in a toothpaste, mouthrinse or varnish, subsequently blocking the dentin tubules in vitro. With respect to these fluoride compounds, the fluoride ions apparently do not contribute effectively to dentin tubule occlusion (Petersson 2013), probably due to the small size of calcium content precipitated crystals (Calabria et al. 2012). Figure 8.2 shows the pattern of calcium fluoride crystal precipitation (a) in comparison with calcium oxalate crystals (b) from both fluoride-containing formulations and potassium oxalate formulations (in-office products). As demonstrated by these pictures, fluoride precipitates predominantly in the body of the intertubular dentin. Relatively small number of particles can be observed inside the tubules, whereas in the potassium oxalate sample, a large number of dentin tubules are occluded below the surface of the dentin. These CLSM images can also be compared with mineralised and acid conditioned dentin (a and b – in Fig. 8.1). This apparently ineffective action observed in in vitro studies does not however correspond to the clinical studies using fluoride formulations, and this may be due to the difficulties in completely mimicking the oral environment in the laboratory (see Chap. 6). A number of these studies have demonstrated that DH may be reasonably well controlled by using a fluoride-containing toothpaste (1,450 ppm) during the duration of the study, especially in the combination with the various tubule-occluding agents discussed in this chapter.
The incorporation of metal ions (e.g. zinc, tin, strontium and potassium) and abrasive components in a toothpaste or mouthrinse formulation (e.g. alumina, silica, calcium carbonate, zinc, etc.) may also have a synergistic effect with the active ingredient on the dentin surface and block the dentin tubules (Gillam 1992; Petersson 2013). For example, a F-toothpaste with 0.454 % stannous fluoride (SnF2) has been reported to be more effective in reducing DH following 4 weeks of daily use when compared to a toothpaste with 0.76 % MFP (Schiff et al. 2000). He et al. (2011) also reported a significant improvement in both significantly immediate and ongoing relief from a 0.45 % SnF2 toothpaste compared to a 0.76 % sodium monofluorophosphate (MFP) toothpaste utilised as a negative-control group. Other desensitising agents in combination with fluoride and associated metal ions (e.g. strontium, 8 % arginine and calcium carbonate) have also been reported to be effective in clinical studies (Orcahrdson and Gillam 2006). Amine fluorides (AMFLOR™, Pharmaceuticals) have also been used in toothpaste and mouthrinse formulations to alleviate pain associated with DH, although currently there are limited data on its effectiveness as a desensitising agent. A recent study by Pradeep et al. (2012) however reported that a amine fluoride toothpaste formulation had a similar effect on DH, compared to a calcium sodium phosphosilicate and potassium nitrate containing toothpaste.
The adjunctive use of a fluoridated mouthrinse therapy in controlling DH in conjunction with the regular use of a desensitising toothpaste may also be recommended (e.g. potassium and amine fluoride) (Yates et al. 2004; Petersson and Kambara 2004; Glockner 2013; Petersson 2013; Pradeep et al. 2012), although currently there are limited data on their effectiveness (Petersson 2013). Other fluoridated mouth rinse formulations incorporating the various desensitising agents mentioned in this chapter may also enhance the effectiveness of fluoride toothpaste formulations (Petersson and Kambara 2004) and perhaps favour the remineralisation of dentin (Glockner 2013).
Irrespective of the actual active agent, the effectiveness of OTC products is dependent of the individual (patient or consumer) maintaining regular and effective oral hygiene practices by applying the toothpaste and/or mouthrinse on a twice daily basis (Petersson 2013). However, depending on the nature of these OTC products, its active component may take up to 2–4 weeks to achieve relief of DH (Talioti et al. 2014) (see also Chap. 10). One of the problems in evaluating the claims of these desensitising products in clinical studies is the lack of heterogeneity of the published studies which makes the results difficult to understand (Karim and Gillam 2013; Talioti et al. 2014). Furthermore, as discussed in Chap. 7, placebo and non-placebo effects may also impact on the results from these studies, although Lin et al. (2013) in a systematic review reported that despite these observed effects, both in-office and OTC products, techniques and treatment approaches may have a real effect on DH.
With regard to the effectiveness of the regular use of a fluoride-containing toothpaste in reducing DH, it was observed that the prevalence was higher in regions where individuals regularly used fluoride toothpaste and lived in fluoridated water area. This may, to some extent, question the apparent effectiveness of fluoride in minimising DH (Rösing et al. 2009; West 2008). According to Rösing et al. (2009), there are, however, limited data supporting the sole use of OTC fluoride products for treating DH, but fluoride in combination with tubule-occluding toothpaste and mouthrinse formulations may be a valuable option in terms of preventing and controlling other oral conditions, namely, plaque, caries, gingivitis, malodour, etc. (Cummins 2010; Pradeep et al. 2012; Glockner 2013; Petersson 2013). There is no evidence supporting the efficacy of these anticaries claims for specific desensitising toothpaste and mouthrinse formulations per se, but only appended claims of fluoride efficacy from the anticaries studies (so-called piggyback claims) (see Chap. 1). Whether high concentration of fluoride in in a toothpaste, for example, 2,800/5,000 ppm (Duraphat) (see Table 8.2), may be effective as desensitisers has not been fully explored, although they have a recognised anticaries effect and may be effective in preventing and controlling root caries (Bizhang et al. 2009; Nordström and Birkhed 2010; Walsh et al. 2010; Srinivasan et al. 2014).
Strontium-Containing Products
Although strontium (historically in the form of strontium chloride and more recently as strontium acetate) in toothpaste formulations have been extensively evaluated in clinical studies over the last 50–60 years and reported to be effective in treating DH compared to placebo controls (Kobler et al. 2008; Liu and Hu 2012; Sharif et al. 2013; Markowitz 2009; Mason et al. 2010), nevertheless there was controversy over whether these formulations were effective in treating DH (Schiff et al. 1994; Rösing et al. 2009; Cummins 2010; Karim and Gillam 2013). Furthermore, Jackson (2000) in a review on the studies on strontium containing toothpaste formulations reported that none of these studies demonstrated a consistent, significant improvement in the participants’ symptoms from DH when compared with the negative-control toothpaste. There was also, according to Jackson (2000
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


