The goals of craniofacial surgery include establishing a stable morphology and improving facial aesthetics. Surgical treatment may necessitate manipulation of the soft tissues or bony structures based on the particular dysmorphology. The failure of fusion that creates facial clefting is usually repaired in infancy during the growth phase. Just repairing these soft tissues in key growth areas may have negative consequences later in life. This interplay highlights the possible biologic consequences of early intervention during the growth phase.
When skeletal discrepancies exceed the envelope of those that can be appropriately treated with orthopedic growth modification and/or orthodontic compensation techniques, surgical repositioning of the craniofacial structures may be indicated. In many instances, patients with skeletal deformities benefit from surgical correction following the completion of facial growth. This approach allows for a definitive correction that is highly predictable and stable in the majority of cases. In contrast, surgical correction performed before skeletal maturity is less predictable and may require reoperation following skeletal maturation. However, early intervention may be warranted for functional or aesthetic reasons. Unfortunately, the hoped-for advantage of early surgical interventions to “unlock growth” has not been realized, and in most cases, there are no clear benefits to early operative intervention, which is partially due to the associated drawbacks. These common issues emphasize the importance of considering growth when planning treatment for surgical reconstruction.
This chapter reviews the concepts of growth and development in the craniofacial skeleton as they relate to the treatment of soft tissue and skeletal dysmorphologies. The basic principles of craniofacial growth are reviewed, and the specific patterns of craniofacial dysmorphologies are discussed with regard to potential early and/or staged intervention. A balanced approach to treatment planning is presented with growth as the center of discussion. However, functional aspects of the airway and occlusion are of considerable importance in some patients. Certain clinical situations require intervention even at the cost of harming growth potential when there is a significant benefit perceived. Additionally, aesthetic concerns in patients with severe deformity require careful consideration for psychosocial reasons.
GROWTH DISCREPANCY AND THE CRANIOFACIAL SKELETON
Growth discrepancies involving the craniofacial skeleton are common, and many of these discrepancies can be managed with orthopedic growth modification and/or orthodontics alone if they are not severe. In particular, congenital craniofacial malformations, deformities, and disruptions may have severe skeletal dysmorphologies and discrepancies. For example, deformational plagiocephaly causes cranial and possibly orbital asymmetry that when diagnosed early is treated with a form of growth modification using custom-molding helmets or bands. In instances when the discrepancy is particularly large or other deformities of the cranio-orbital region are encountered, surgery may be helpful to dismantle the craniofacial components and reposition them in a more normal conformation. There are a number of examples of skeletal and soft tissue discrepancies that occur in childhood requiring treatment. Deciding when to intervene is important to optimize the long-term results for these clinical challenges.
Growth abnormalities and dysmorphology of the lower face are the most commonly encountered clinical problems for the craniomaxillofacial surgeon. When these discrepancies involve the teeth, most minor discrepancies are treated with orthodontic compensation. However, some are beyond the envelope of orthodontic compensation techniques and may benefit from surgical repositioning of skeletal components. Orthognathic surgery for the correction of skeletal discrepancy and malocclusion has traditionally been undertaken following the completion of growth, and there is considerable contemporary literature regarding the effects and stability of these procedures. However, there are only a limited number of studies that have investigated the outcome following orthognathic, craniofacial, or other types of maxillofacial surgery performed in the growing child. The supposition that surgical intervention before skeletal maturation may “inhibit” the future growth potential of the involved bone is long standing, especially if a growth center is involved. This concept is in part based upon the findings obtained from studies of patients with cleft lip and palate deformities, Robin sequence, craniofacial microsomia, Treacher Collins syndrome, and a range of other conditions in those who had undergone surgical procedures during growth. The results and observations from these studies do provide information about growth potential; however, is it imperative to recognize that these patients also have an underlying dysmorphology that may influence facial growth independent of surgical correction. In the assessment of subsequent facial growth problems, it is difficult to delineate between that related to the preexisting condition with its aberrant growth pattern and that potentially caused by the surgical osteotomy or other manipulations. Early surgery has usually been reserved for individuals with marked skeletal dysmorphologies and/or severe functional concerns (e.g., intracranial pressure increases, choanal atresia, or severe obstructive sleep apnea). The presence of severe functional problems or implications for the psychosocial development of the child may become important when considering early surgery. A firm understanding of the patterns of facial growth is essential when planning surgical reconstruction.
There is some predictability to the growth of the cranium and face, but individual variation and pathologic conditions must be considered. Common growth variations (e.g., vertical maxillary excess with mandibular hypoplasia) and pathologic clinical situations (e.g., maxillary hypoplasia in the patient with a cleft palate) should be recognized, and treatment planned and staged with these issues in mind. Clinicians must be aware of these early discrepancies, not to force early intervention in most cases, but to develop a diagnosis and stage the reconstruction for the most predictable result. Treatment plans can then be formulated based on the best estimation of the expected pattern of growth.
CONCEPTS OF CRANIOFACIAL SKELETAL GROWTH AND DEVELOPMENT
Craniofacial development, growth, and remodeling are a complex interplay of structure and function beginning in the embryo and continuing throughout adult life. The delicate equilibrium that exists between various parts of the craniofacial skeleton is stimulated by genes and local function and coordinates complex biomechanical and molecular signaling to yield a composite skeletal form. Problems can occur at anytime during this process and negatively impact the growth and development process. Understanding the basic biology of craniomaxillofacial growth is essential when planning treatment for malformations, disruptions, and deformities. The basic definitions of growth are important to understand when discussing the biology of growth and development ( Table 43-1 ).
| Term | Definition |
|---|---|
| Dysmorphology | Abnormal morphology of tissues |
| Malformation | Formation of tissue is poor as a result of an intrinsic problem with development |
| Disruption | A breakdown in normal tissue development causing abnormal morphology |
| Deformation | Changes in morphology caused by external forces on normal tissue |
| Growth | Increase in cell size (plasia) or cell number (trophy) |
| Remodeling | Compensatory or adaptive changes of tissue |
| Development | Increase in complexity |
| Hypertrophy | Increase in the size of the cells |
| Hyperplasia | Increase in the number of cells |
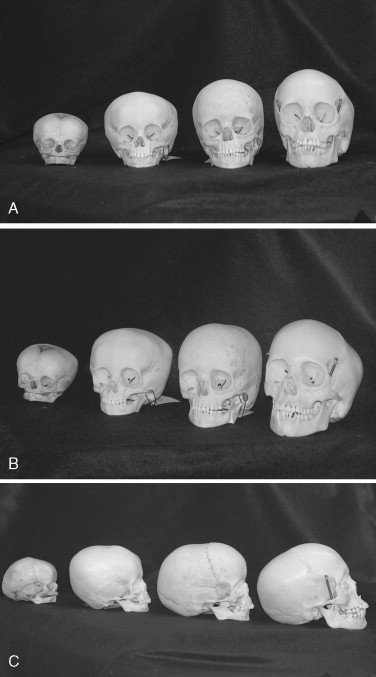
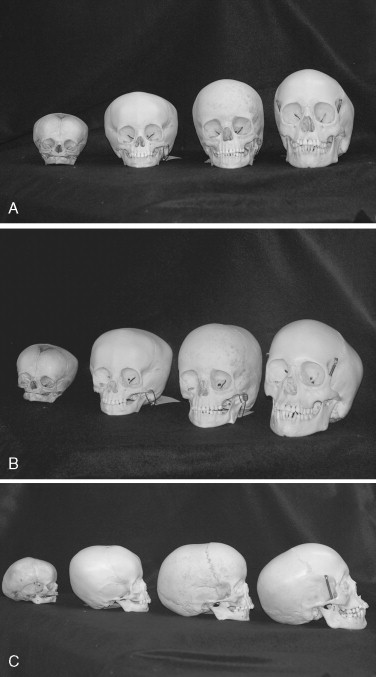
In general, there is a cephalocaudal growth vector that occurs throughout early life and facial development that is thought to be closely linked to the functional demands of each region ( Figure 43-1 ). Enlow has previously discussed the concepts of growth in detail and outlines the two main morphologic events that direct craniofacial growth. These include (1) basal cranium growth and (2) development of the pharyngeal and facial airway structures . This vector of cephalocaudal growth is directly related to the changes seen in the proportions of the head and face during early life. In the early phase, this is reflected in the relative importance of cranial growth as a response to the rapid growth of the brain tissues. This occurs in the neurocranium, which houses the structures of the brain, orbits, and olfactory system, and this region comprises the cranium and upper third of the face. The remainder of the facial tissues accelerate their growth at a later phase as the airway and muscles of mastication increase their function. This represents the viscerocranium ( Table 43-2 ).
| Average Adult % Completed by Age 1 | Average Adult % Completed by Age 5 | Average Age at Maturity | |
|---|---|---|---|
| Cranium | 84%-86% | 90%-94% | Males: 14 yr |
| Females: 16 yr | |||
| Orbits | 84%-86% | 88%-93% | Variable |
| Zygoma | 72% | 83% | Males: 15 yr |
| Females: 13 yr | |||
| Maxilla | 75%-80% | 85% | Males: 15 yr |
| Females: 14 yr | |||
| Mandible | 60%-70% | 74%-85% | Males: 16 yr |
| Females: 14 yr |
The bones of the craniofacial skeleton grow and develop by remodeling and displacement throughout young life. Remodeling occurs as a result of local factors that result in the change in the size and shape of various components of the facial skeleton. Displacement occurs by bones that move apart at the joint, suture, or articular regions. This displacement occurs away from the articular surfaces (i.e., cranial sutures, temporomandibular joints, or maxillary sutures). Bone growth is modulated through this process by augmenting or diminishing various regions in response to the functional needs and the timing of gene expression. The two processes of remodeling and displacement should occur in a coordinated and interdependent fashion. If the processes are balanced, the skeleton develops appropriately. In contrast, if the balance is disturbed (i.e., nasal obstruction or prenatal cranial suture fusion), the skeleton develops outside the envelope of equilibrium resulting in a skeletal discrepancy.
Local signaling appears to occur between the bony components of the face to develop each area in response to the increasing functional demands of mastication and breathing. The orbits, maxillae, and mandible are each dependent upon one another early in this phase, whereas the cranial base has a more intrinsic or genetically based control mechanism. The cranium and orbits will develop in response to the rapid growth of the brain and globes, which occurs during the first year of life, and hence the cranio-orbital complex is comparatively much larger than the maxillomandibular complex in infancy. The early developing neurocranial complex creates a craniocaudal growth vector that is clockwise in direction when viewing the right lateral skull. Later, the functional demands of mastication and deglutition on the mandible become prominent, and the nature of the equilibrium balance with the maxilla is also altered in response to the growth and development of the airway and the functional needs of mastication and speech development. Constant modifications to this process are made throughout growth and development to obtain a functional state of equilibrium.
The equilibrium of the craniofacial complex is altered following a series of normal developmental events. These include:
- 1.
Central neurologic development
- 2.
Optic pathway development
- 3.
Speech and swallowing development
- 4.
Airway and pharyngeal development
- 5.
Facial expression and muscular changes
- 6.
Tooth development and exfoliation
Each region has a unique growth curve, and there are various peaks of growth velocity that alter craniofacial equilibrium resulting in skeletal growth changes to restore this equilibrium. It is essential to have an understanding of each region when deciding the timing of various reconstructive efforts. In general, more definitive corrections are performed later in the growth phase and ideally should be undertaken at the completion of growth because earlier intervention may alter the growth curve and disrupt the equilibrium. Relapse toward the original dysmorphology is more likely to occur when the body attempts to restore the balance that has been altered by surgical intervention performed before skeletal maturation.
CONCEPTS OF CRANIOFACIAL SKELETAL GROWTH AND DEVELOPMENT
Craniofacial development, growth, and remodeling are a complex interplay of structure and function beginning in the embryo and continuing throughout adult life. The delicate equilibrium that exists between various parts of the craniofacial skeleton is stimulated by genes and local function and coordinates complex biomechanical and molecular signaling to yield a composite skeletal form. Problems can occur at anytime during this process and negatively impact the growth and development process. Understanding the basic biology of craniomaxillofacial growth is essential when planning treatment for malformations, disruptions, and deformities. The basic definitions of growth are important to understand when discussing the biology of growth and development ( Table 43-1 ).
| Term | Definition |
|---|---|
| Dysmorphology | Abnormal morphology of tissues |
| Malformation | Formation of tissue is poor as a result of an intrinsic problem with development |
| Disruption | A breakdown in normal tissue development causing abnormal morphology |
| Deformation | Changes in morphology caused by external forces on normal tissue |
| Growth | Increase in cell size (plasia) or cell number (trophy) |
| Remodeling | Compensatory or adaptive changes of tissue |
| Development | Increase in complexity |
| Hypertrophy | Increase in the size of the cells |
| Hyperplasia | Increase in the number of cells |
In general, there is a cephalocaudal growth vector that occurs throughout early life and facial development that is thought to be closely linked to the functional demands of each region ( Figure 43-1 ). Enlow has previously discussed the concepts of growth in detail and outlines the two main morphologic events that direct craniofacial growth. These include (1) basal cranium growth and (2) development of the pharyngeal and facial airway structures . This vector of cephalocaudal growth is directly related to the changes seen in the proportions of the head and face during early life. In the early phase, this is reflected in the relative importance of cranial growth as a response to the rapid growth of the brain tissues. This occurs in the neurocranium, which houses the structures of the brain, orbits, and olfactory system, and this region comprises the cranium and upper third of the face. The remainder of the facial tissues accelerate their growth at a later phase as the airway and muscles of mastication increase their function. This represents the viscerocranium ( Table 43-2 ).
| Average Adult % Completed by Age 1 | Average Adult % Completed by Age 5 | Average Age at Maturity | |
|---|---|---|---|
| Cranium | 84%-86% | 90%-94% | Males: 14 yr |
| Females: 16 yr | |||
| Orbits | 84%-86% | 88%-93% | Variable |
| Zygoma | 72% | 83% | Males: 15 yr |
| Females: 13 yr | |||
| Maxilla | 75%-80% | 85% | Males: 15 yr |
| Females: 14 yr | |||
| Mandible | 60%-70% | 74%-85% | Males: 16 yr |
| Females: 14 yr |
The bones of the craniofacial skeleton grow and develop by remodeling and displacement throughout young life. Remodeling occurs as a result of local factors that result in the change in the size and shape of various components of the facial skeleton. Displacement occurs by bones that move apart at the joint, suture, or articular regions. This displacement occurs away from the articular surfaces (i.e., cranial sutures, temporomandibular joints, or maxillary sutures). Bone growth is modulated through this process by augmenting or diminishing various regions in response to the functional needs and the timing of gene expression. The two processes of remodeling and displacement should occur in a coordinated and interdependent fashion. If the processes are balanced, the skeleton develops appropriately. In contrast, if the balance is disturbed (i.e., nasal obstruction or prenatal cranial suture fusion), the skeleton develops outside the envelope of equilibrium resulting in a skeletal discrepancy.
Local signaling appears to occur between the bony components of the face to develop each area in response to the increasing functional demands of mastication and breathing. The orbits, maxillae, and mandible are each dependent upon one another early in this phase, whereas the cranial base has a more intrinsic or genetically based control mechanism. The cranium and orbits will develop in response to the rapid growth of the brain and globes, which occurs during the first year of life, and hence the cranio-orbital complex is comparatively much larger than the maxillomandibular complex in infancy. The early developing neurocranial complex creates a craniocaudal growth vector that is clockwise in direction when viewing the right lateral skull. Later, the functional demands of mastication and deglutition on the mandible become prominent, and the nature of the equilibrium balance with the maxilla is also altered in response to the growth and development of the airway and the functional needs of mastication and speech development. Constant modifications to this process are made throughout growth and development to obtain a functional state of equilibrium.
The equilibrium of the craniofacial complex is altered following a series of normal developmental events. These include:
- 1.
Central neurologic development
- 2.
Optic pathway development
- 3.
Speech and swallowing development
- 4.
Airway and pharyngeal development
- 5.
Facial expression and muscular changes
- 6.
Tooth development and exfoliation
Each region has a unique growth curve, and there are various peaks of growth velocity that alter craniofacial equilibrium resulting in skeletal growth changes to restore this equilibrium. It is essential to have an understanding of each region when deciding the timing of various reconstructive efforts. In general, more definitive corrections are performed later in the growth phase and ideally should be undertaken at the completion of growth because earlier intervention may alter the growth curve and disrupt the equilibrium. Relapse toward the original dysmorphology is more likely to occur when the body attempts to restore the balance that has been altered by surgical intervention performed before skeletal maturation.
REGIONS OF CRANIOFACIAL GROWTH AND DEVELOPMENT
CRANIUM
The cranium is made up of the chondrocranium and the neurocranium. The chondrocranium, or cranial base, develops initially in cartilage derived from occipital somites and then becomes bone by endochondral ossification. These ossification centers form the bones of the base of the skull (i.e., the occipital, sphenoid, temporal, and ethmoid bones). Growth of the cranial base bones occurs interstitially at articulations called synchondroses. Whereas the majority of the growth is occurring at the synchondroses, once ossified, the inner and outer surfaces of each bone can also remodel via appositional growth.
The neurocranium, or cranial vault, is made up of large and small curved, flat bones that are formed intramembranously, the majority of which are derived from neural crest cells. The growth of these bones occurs interstitially at the fibrous articulations (i.e., the sutures) and appositionally on the endocortical and ectocortical surfaces. The cranial vault grows rapidly in the first year of life, and the velocity of growth plateaus in the following 5 years. A diploic space is present between two clear cortices of bone in most children between the ages of 2 and 5 years. The vast majority of growth in this area is complete by ages 5 to 7 years. At 1 year of age, the width of the head is 84% of its adult size, and at 5 years of age, the head width increases to 93%. Head circumference is similar with 86% of the growth complete by 1 year of age and 94% of growth completed by 5 years of age. The maturation age of the cranium width is 14 years in females and 15 in males. The incredible amount of growth within the first 5 years of life is reflective of the neurodevelopment that occurs during this time.
Craniosynostosis is the premature fusion of cranial vault sutures, which is generally an antenatal event that causes growth restriction perpendicular to the affected suture. Craniosynostosis is most often seen with only one suture. However, craniofacial dysostosis syndromes occur when the cranial base synchondroses (primarily the presphenoethmoid synchondroses) and, to a lesser extent, the cranial vault sutures are affected to varying degrees. The alteration of the midface occurs in craniofacial dysostosis syndromes, such as Apert’s, Pfeiffer, and Crouzon’s syndromes. These syndromes are characterized by a restriction of growth in the anterior cranial vault and cranial base that results in severe orbital and midfacial hypoplasia and Class III malocclusion. In addition, when the brain and cranial base components do not form in their normal fashion (i.e., Binder sequence and Down syndrome), the development of the midfacial complex and the balance is also distorted.
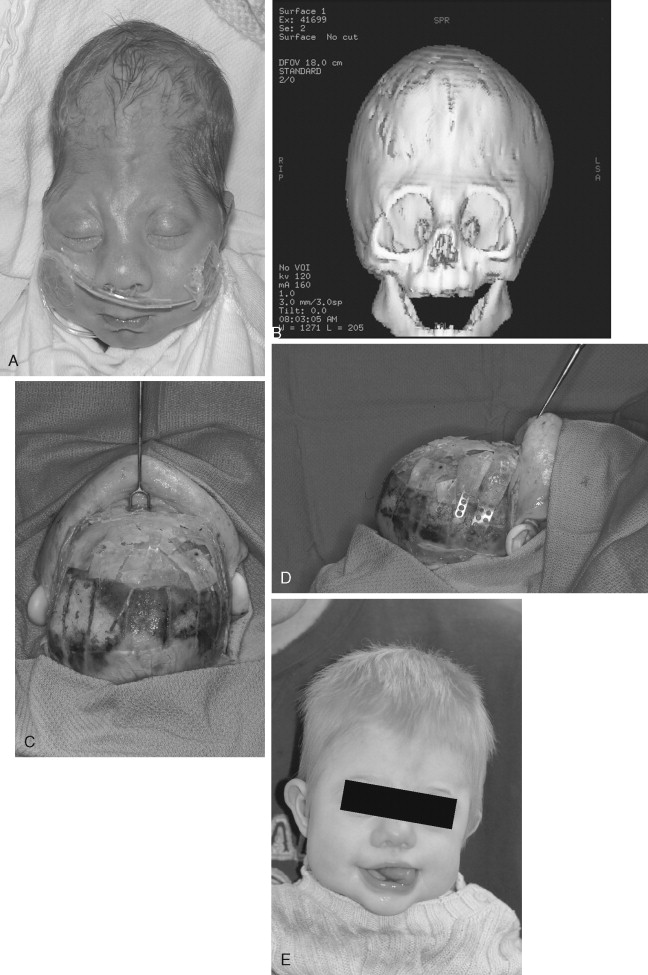
In many cases, treatment of dysmorphology in the cranial vault and orbits is usually more definitive after 1 year of age since the vast majority of growth in the cranium is complete at this time. In the case of craniosynostosis, surgical correction is necessary earlier to allow appropriate volume for brain growth. For patients with craniofacial dysostosis in which skull base fusion has also affected the orbits and midface, this is corrected at a later stage ( Figure 43-2 ).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses