In the field of craniofacial surgery, different surgical methods for treating skull-base lesions have evolved. A thorough understanding of the microsurgical and functional anatomy of the anterior skull base is crucial for optimal selection of surgical approach and minimizing complications. Frazell and Lewis’ observation, “The entire cribriform plate can rarely be resected without creating cerebral complications” , reflects the therapeutic principles generally accepted in 1963. Since then, innovative and aggressive surgical techniques evolved because of the high rate of failure and complications following radiation therapy for nonresectable tumors in this area. Improved survival rates stemmed from the realization that en bloc resection of the tumor in the ethmoidal roof or cribriform plate area is possible only through a combined transcranial and facial approach .
Smith and colleagues first described the combined facial and intracranial tumor resection for frontal sinus tumors. Dandy and Ray and McLean set the stage for surgical possibilities in the skull-base area when they described a combined intracranial orbital approach to posterior orbital tumors. In 1959, Malecki described a combined approach for treatment of posterior frontal, sphenoid, and ethmoidal roof fractures . In 1963, Ketcham and colleagues emphasized the need for ethmoidal roof and cribriform resection of tumors in the paranasal sinuses. Derome applied craniofacial resection techniques when developing transbasal surgery for regions of the sphenoid and clivus. In 1969, Terz and colleagues described modifications for surgery of tumor extensions into the pterygoid fossa. The rate of complications associated with his modifications, however, was high. Over the next 3 decades, multiple publications established the usefulness of combined resection techniques for removal of tumors involving the anterior cranial floor, ethmoidal roof, cribriform plate, or orbital roof.
The risk of intraoperative hemorrhage, injury to intracranial structures, and cerebrospinal fluid (CSF) leaks can largely be obviated by the combined methods. Involvement of important structures, such as the cavernous sinus, internal carotid artery, and optic nerve, however, impose the primary limitations of craniofacial resection techniques for malignant anterior cranial-base lesions .
In the past decade, using endoscopy and endoscope-assisted microsurgery has evolved for the treatment of selected pathologies of the skull base, primarily in the sellar and suprasellar regions. The endonasal transsphenoidal approach permits the exposure and removal of sellar and selected suprasellar lesions without the need for brain retraction .
Craniofacial skull-base lesions
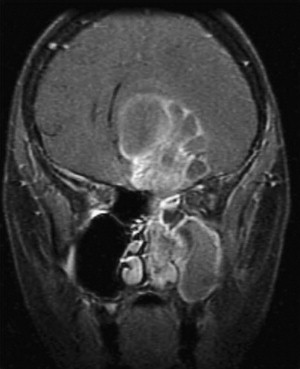
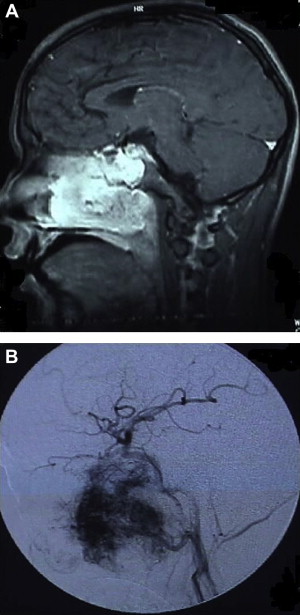
Microsurgery remains the preferred therapeutic modality for a myriad of disorders involving the craniofacial junction. These disorders may be classified as lesions arising extracranially, lesions arising from bones, and lesions arising intracranially but extending beyond the confines of the cranium ( Table 1 ). Clinical behavior can be extremely variable. Fibrous dysplasia of the frontal bone may warrant surgery only when its local extension produces symptoms resulting from compression or expansion. Fibrosarcoma involving the same location, however, mandates immediate surgical excision. Radiographic features often help the surgeon make the proper differential diagnosis. CT scan and MR, with axial, sagittal, and coronal views, are complementary and are necessary for full delineation of the lesion and involvement of surrounding structures ( Figs. 1–4 ). These factors are crucial in deciding operability and planning the surgical approach and its extensiveness. Adequate biopsies, however, are generally required for confirmation of the diagnosis and planning the surgical treatment. Biopsy is generally recommended to exclude tumors that can be treated with radiation or chemotherapy and do not require resection, such as lymphoma. Frequently, an adequate biopsy can be obtained via a transnasal, transantral, nasopharyngeal, or other extracranial approaches .
| Arising Extracranially, May Extend Intracranially | Arising From Cranial Bones, May Extend Extracranially or Intracranially | Arising Intracranially, May Extend Extracranially |
|---|---|---|
| Cutaneous: Basal and squamous cell carcinomas and melanoma Orbital: Neuroblastoma, optic nerve glioma and rhabdomyosarcoma Paranasal and nasal cavities: Adenocarcinoma and squamous cell carcinoma Salivary glands: Adenocarcinoma and mucoepidermoid tumors Others: Esthesioneuroblastoma, nasopharyngeal angiofibroma, and sarcoma |
Chordoma Osteoma Fibrous dysplasia Chondroma Chondrosarcoma Fibrosarcoma Osteosarcoma |
Meningioma Neurofibroma |


Craniofacial resection of anterior skull-base lesions
Indications
This is a transcranial extradural approach to the anterior skull base through a unilateral or bifrontal craniotomy. It is primarily designed for sinonasal and nasopharyngeal tumors (see Fig. 1 ) involving the anterior skull base. Several variations of this approach with extensions involving osteotomies of the orbit and nasal bone allow further exposure of anterior and central skull-base structures in the midline . This approach provides an excellent subfrontal access to midline and paramedian lesion but also for bilateral orbital and cavernous sinus lesions. An extended orbitofrontal approach is used for unilateral orbital and anterior middle fossa lesions.
This approach has many advantages: a cosmetically invisible incision; the ability to reconstruct the face, orbits, and nose, as well as the forehead; access to a large area of the skull base; and ready access to cranial bone for splitting to aid in the reconstruction. In addition, this approach under the frontal lobes minimizes brain retraction and allows both intradural and extradural access if necessary .
Operative Technique
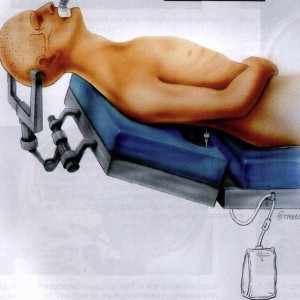
The patient with an anterior skull-base lesion is placed in the supine position with the head in a horseshoe headrest or Mayfield head holder. A lumbar drain is inserted through a split mattress into the lumbar thecal sac and connected to a spinal drainage set ( Fig. 5 ). The head, face, and neck are prepared and draped in the usual manner. The right thigh of the patient is also prepped and draped for possible harvesting of fascia lata and split-thickness skin grafts. The 2 operating disciplines (neurosurgery and otolaryngology) maintain separate instruments and fields to minimize cranial contamination by nasopharyngeal flora .
Cranial component
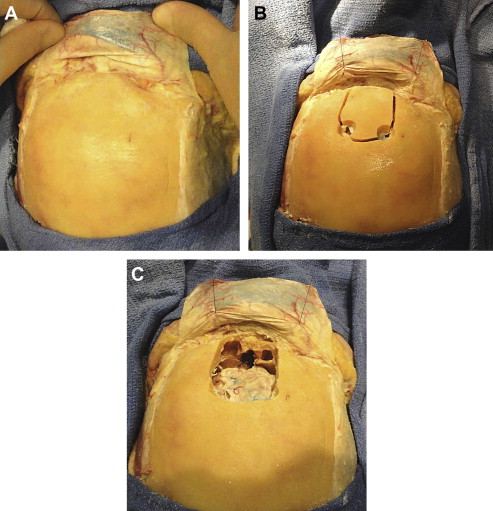
A bicoronal incision is most commonly used for standard craniofacial approach. A skin flap is elevated and retracted anteriorly. The frontalis fascia underlying the galea and temporal fascia are initially preserved. The frontalis fascia is incised bicoronally as posterior as possible along the superior temporal lines, elevated anteriorly without temporalis muscles, and kept attached at the supraorbital margin supplied by the supraorbital vessels. This provides a superbly vascularized pericranial flap that not only offers a barrier at the craniofacial defect but also provides strong support to the brain ( Fig. 6 ).
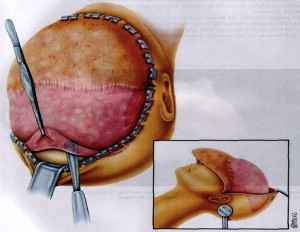
A rectangular craniotomy based at the midline is performed using the high-speed drill. Two posterior holes on each side of the sagittal sinus are connected using a rongeur. The midline burr hole and the keyhole are connected using a Gigli saw. The remaining holes are connected using the craniotome, and the bone flap is removed. The frontal sinus mucosa is exenterated and the posterior wall of the frontal sinus is removed from the cranial flap ( Fig. 7 ).