Maxillofacial trauma as a discipline unto itself has undergone tremendous change over time. These changes have been mandated by the evolving complexity of injuries of this age as well as advances in modern imaging, instrumentation, and techniques such as rigid fixation. Perhaps the greatest impetus for change in the approaches of surgical management of maxillofacial trauma has been born through the conflicts of the world wars. The pioneering efforts of surgeons such as Kazanjian and Gillies are examples of these advancements. These triumphs in the management of maxillofacial trauma were then moved forward and further refined by surgeons such as Thoma, Blair, Ivy, Curtis, Dingman, Natvig, Rowe, and Killey. However, in the surgical management of pediatric cranio-maxillofacial disease and deformity, perhaps the greatest influence came from the contribution of Paul Tessier in his principles of cranio-orbital surgery first introduced in 1967. Gruss et al and Manson et al provided the many operative principles of maxillofacial trauma employed today, such as sequencing of panfacial injuries and autogenous bone grafting, as well as the important role of rigid fixation in re-establishing facial height, width, and projection. These principles have provided the fundamental underpinnings of modern facial fracture treatment. More recently, these principles, which work so well in the adult patient, have been applied in the management of pediatric maxillofacial trauma. Posnick and Kaban have more clearly described the epidemiology and further clarified the advantages of rigid internal fixation for these injuries.
Fundamentally, understanding of complex facial injuries evolved through experience, both good and bad, with adult patients. However, one must carefully consider that children are not simply “small adults” and that the application of adult type treatment can be inappropriate in many circumstances. There is still a place for conservatism in treatment of cranio-maxillofacial injuries in the child.
There are some that feel behavior modification of the surgeon is one of the more important cornerstones of management when dealing with the injured child. However, we believe that while compassion and a pleasing bedside manner should be shown to all patients, especially children, the pediatric patient is done a much greater service through the surgeon’s understanding of the complex issues surrounding growth of the craniofacial skeleton and the potential for traumatic and surgical injury to alter it negatively.
GENERAL CONSIDERATIONS
CRANIOFACIAL GROWTH AND DEVELOPMENT
The role of the human face is significant in both a direct and an indirect fashion for reasons other than purely aesthetic considerations. This is secondary to the highly evolved and specialized functions of the face, such as in vision, breathing, mastication, speech, smell, and hearing. Indeed, it is the culmination of an extremely complex process of growth and development that provides the functional and aesthetic framework of the human face. Interruption of this process, such as insult from maxillofacial injury, may produce deleterious alterations of the facial framework, resulting in aesthetic and functional deficits that are apparent and hard to ignore. For the surgeon who treats pediatric facial fractures, an understanding of this process becomes crucial in developing and exercising sound surgical judgment ( Figure 20-1 ).

The cranial vault at birth is composed of flat plates of intramembranous bone separated by connective tissue. The interposing areas or sutures allow for deformation of the head through the pelvis during delivery and then accommodate rapid brain growth during the first year of life. This is largely accomplished through apposition of bone at the sutural areas and to a lesser degree remodeling of the inner and outer cortex of the skull. Head circumference reaches greater than 90% of its adult size between 3 and 5 years of age. In contrast, the bones of the skull base are formed from areas of endochondral ossification. In between these areas of ossification, synchondroses are formed that continue to allow for growth through the replacement of cartilage with bone. The orbit, although composed of many bones, reaches skeletal maturity relatively quickly at about age 5 to 7 years. This mirrors growth of the soft tissue orbital contents. The midface is composed of intramembranous bone and its growth vector is downward and forward. This is propelled by apposition of bone at the cranial base and deep sutures of the maxilla as well as remodeling of the surface of the midface. The mandible, on the other hand, has a component of endochondral ossification at the temporomandibular joint regions bilaterally as well as both remodeling and apposition of bone everywhere else. The mandibular body and alveolus again follow the downward and forward vector of movement the midface takes, but the rami and condyles grow upward and backward to maintain contact with the skull base. Vertical height is gained at the condyle through endochondral replacement and length is added through an active remodeling of the ramus. Skeletal maturity of the maxilla and mandible is reached by approximately 14 to 16 years of age in females and 16 to 18 years of age in males.
The functional matrix concept of growth first proposed by Moss has gained general acceptance. The theory in essence postulates that growth occurs as a result of expanding functional requirements of the cranial, nasal, and oral cavities and that these requirements are transmitted to the bone and cartilage from the soft tissue envelope of the face. The bones grow in response to the expansion of the cranial and facial capsule. The nasal septum and mandibular condyles thus react to growth requirements and therefore should not be considered the “primary centers” of growth as once believed. Therefore surgical attention in managing injuries of the mandibular condyle, for example, should be directed at preserving as scar-free an envelope of soft tissue as possible and promoting function of the joint. Extending this theory to a myriad of other craniofacial problems leads to similar conclusions. A classic example of the influence of the soft tissue envelope on growth resides in the patient with cleft palate. Maxillary growth restriction in these patients is the result of scarring from palatal surgery. The cleft palate itself, if left unoperated until skeletal maturity, would have little to no effect on maxillary growth. The importance of understanding the deleterious effects of scar tissue, traumatically or surgically induced, and its restrictive effects on growth and development cannot be overstated when managing the child with facial fractures.
SURGICAL ANATOMY
Critical examination of the stages of gross anatomic craniofacial development leads to several particular issues that have an impact in both the epidemiology and the management of facial bone injuries in children. First, during infancy and early childhood rapid brain growth causes a significant increase in head circumference, as noted in the previous discussion regarding growth and development. In addition, the orbits also reach skeletal maturity early in life (5 to 7 years of age). This provides for the characteristic appearance of the very prominent forehead and orbits seen in infancy and early childhood. The later maturing lower facial skeleton remains relatively protected behind these prominent facial features during this timeframe. As such, the relatively exposed forehead and orbits are more prone to injury. The bone itself during the early years of development has a very high osteogenic potential and is characterized by thick medullary space and thin bony cortices, lending the bone to a greater likelihood of greenstick fracture. The teeth in the primary dentition have particularly short, bulbous crowns that can make it difficult to achieve stable maxillomandibular fixation during fracture reduction and stabilization using traditional techniques.
The development of the craniofacial skeleton during the later childhood years into the mixed dentition period also yields further insight. During this time, the lower two thirds of the face becomes more prominent as a result of the forward and downward growth of the face, thus exposing bones in this area to more injuries. This stage of development also is characterized by the development of the permanent tooth buds, which occupy space in the maxilla and mandible. These unerupted teeth also create areas of structural weakness in the bone and a greater probability of sustaining a fracture. In addition, the eruption of the permanent teeth in conjunction with loose, exfoliating primary teeth makes maxillomandibular wiring and thus fracture reduction and stabilization more difficult. The bone itself still has excellent, although decreasing, osteogenic potential and elasticity during this time. The sinuses of the face also continue their development and change fracture patterns secondary to different areas of strength and weakness in the bone as a result of their presence. As the permanent dentition becomes fully erupted at about 12 years of age, and growth continues through the early teenage years, the craniofacial skeleton becomes more adult-like in its form and its surgical management.
EPIDEMIOLOGY
Children have a lower incidence of facial bone injury. For the most part they reside in a very protective social environment. In the early years of life, parental supervision and a child-friendly environment mitigate the likelihood of serious injury. Although falls during these years are common, their low center of gravity ensures that little harmful force is generated that might cause injury. As they reach the later childhood years, children become involved in numerous activities, such as school, and play with other children. Participation in athletic activity later in life is also a cause of facial injury proximate to a developing neuromuscular coordination system and decreased situational awareness. Balls of all sorts, hockey pucks and sticks, lacrosse sticks, bats, elbows, and knees are often the cause of pediatric facial injuries during athletic events, especially when the appropriate personal protective equipment is not worn.
While there have been several excellent studies regarding the epidemiology of pediatric facial trauma, Posnick et al provided the most significant recent description of this problem. In his review of 137 pediatric patients with facial fractures, the majority of injuries occurred to males 6 to 12 years of age. The most common cause of trauma was motor vehicle related followed by falls, sports injuries, and interpersonal violent altercation. Mandibular fractures comprised 55% of the injuries, orbital fractures 30%, dentoalveolar fractures 23%, midface fractures 17%, nasal fractures 15%, zygomaticomaxillary complex fractures 14%, and cranial fractures 6% of the injuries. Among the reported mandibular fractures, condyle fractures were the most common, followed by the symphyseal region, body area, and last the angle of the mandible. However, from a rationale standpoint, actual incidence may vary across the geographic locations dependent upon many factors and the absence or presence of a level I pediatric trauma facility. In addition, many more minor injuries such as nasal and dentoalveolar fractures are likely underreported because they can be commonly managed on an outpatient basis. There were no cervical spine injuries in this study.
PREVENTION
As noted previously, children are ensconced in a relatively well-protected social environment with close adult supervision during their early years. However, as they begin to engage in social and athletic activity, their exposure to situations in which injury might occur heightens. The use of personal protective equipment is critical to reducing the incidence of facial injuries in children. Specifically included are the use of helmets, face shields, and mouth guards during sports play. However, just as crucial is the use of protective equipment during nonathletic activity such bicycling and skateboarding. Recently there has been significant social momentum to change the composition of playground equipment and the surfaces of athletic fields to further lessen the chance of injury. Adults, either indirectly or directly, supervising children engaged in these activities must assume the responsibility of ensuring that the appropriate safety equipment is utilized.
Perhaps the single most important factor in reducing the incidence of pediatric trauma overall is the correct mandatory use of seat belts and safety seats in vehicles. According to recommendations from the National Highway Traffic Safety Administration (NHTSA), a rear-facing seat in the back seat of a vehicle should be used until the child is 1 year of age and weighs 20 pounds. Forward-facing seats in the back seat should then be used until 4 years of age and a weight of 40 pounds. Newer recommendations with a campaign for public awareness from the NHTSA have been proposed, stating that children should next be placed in a booster seat with a seat belt in the rear of the vehicle from age 4 until at least age 8 unless the child is at least 4 feet 9 inches tall. The common use of air bag restraint systems in the modern vehicle has concerns as far as children and infants. Guidelines from the NHTSA here again remain consistent; children and especially infants should never be placed in the right front seat of the car with an active air bag. Rising as a new scourge is the increasing popularity of all-terrain vehicles, especially in rural areas. Little federal or state regulation exists for the operation of these motorized vehicles, and older children with little to no experience and judgment are often allowed in the driver’s position, leading to horrendous facial and other injuries as seen on a nationwide scale. Again, close adult supervision and responsibility are critical to ensure that safety measures are followed.
Other areas of focus regarding prevention include the alarming incidence of gun violence directed at or involving children. It is almost unusual today to have a month elapse in which a school shooting has not occurred somewhere in the nation. Educational efforts directed at firearms’ safety in the home and at schools and heightened awareness by the public about this issue continue to remain the best ways to fight this burden affecting America’s children and youth.
PERI-OPERATIVE MANAGEMENT
As mentioned previously, children are not small adults and there can be little margin for error. As such, a meticulous surgical treatment plan must be designed not only for the management of the facial injuries, but also for the examination, resuscitation, intraoperative, and postoperative care of the patient. Children in general have tremendous resiliency to stress from surgical procedures, but they are not tolerant of inappropriate fluid and drug administration.
Surgical preoperative management begins with the initial examination. The physical examination and history is not significantly different than that for the adult patient with the exception that much of the history must be obtained from the parents or other caretaker. Obtaining co-operation for the physical exam can be very difficult, especially with children who have recently experienced a traumatic injury. Gentle examination with encouragement from the child’s parents is usually sufficient. Examination under general anesthesia or sedation should be approached with caution during initial management because this may obfuscate neurologic injury. In addition, because of difficulty with movement during radiologic procedures such as CT scans, sedation or anesthesia may be necessary to ensure the diagnostic value of the study obtained. In the management of the injured child in extremis, adherence to the prescribed trauma life support algorithm is the treatment of choice. Severe airway embarrassment secondary to cranio-maxillofacial trauma in children is rare. However, management here differs in that cricothyroidotomy for surgical relief of the airway in children less than 12 years of age is contraindicated to decrease the risk of subglottic stenosis.
Intravenous fluids should be calculated using the 4-2-1 rule or; 4 milliliters per kilogram per hour (mL/kg/h) for the first 10 kg of weight, 2 mL/kg/h for the second 11-20 kg of weight, followed by 1 mL/kg/h for each additional kilogram of weight thereafter. The importance of calculating fluid replacement and maintenance from a weight-based standpoint cannot be overemphasized. Maintenance fluids in younger children are usually given as ¼ normal saline with dextrose; ½ normal saline should be reserved for older children and teenagers. Urine output is normally 1-2 mL/kg/h in the child and should be measured to ensure adequate volume. In situations with major volume loss, the surgeon should seek to resuscitate the child appropriately with the appropriate crystalloid fluids in a 3 mL to 1 mL of blood loss ratio. When blood transfusions are required, the transfusion requirement ideally should be weight based. In addition, as a result of the smaller amount of intravascular volume, the surgeon should be cognizant that coagulopathy is more likely given the amount of blood transfused. Acidosis is a particularly ominous sign in children, reflecting inadequate tissue perfusion, and should be managed early and aggressively.
Hypothermia in children remains a great concern. Every attempt should be made to ensure that during preoperative examination and intraoperative positioning, the room temperature is elevated for patient safety and that care is taken to prevent hypothermia. Nutrition is also a major consideration in the pediatric trauma patient. Unlike adults, adequate nutrition in children is necessary for continual growth and development. For those children who are not able to take an oral diet for an extended period of time, tube feeding or possibly parenteral nutritional supplementation may be necessary. However, enteral feeding methods are preferred.
UPPER AND MIDFACIAL INJURIES
FRONTAL BONE AND SUPERIOR ORBITAL FRACTURES
As a result of rapid brain growth in infancy, the upper third of the facial skeleton remains relatively prominent in early childhood. For this reason, injury to this anatomic region is a common fracture pattern. Neurosurgical and ophthalmologic concerns must come first before management of the facial bone injuries. Operative intervention for neurologic injury such as repair of dural tears should viewed by the maxillofacial trauma surgeon as an opportunity to collaborate with the neurosurgeon and simultaneously reduce and fix the fractured segments as necessary, ideally through a coronal incision. In the absence of a cerebrospinal fluid (CSF) leak and significant displacement of the fractured segments, frontal bone injuries can be managed conservatively in a closed fashion without significant functional or aesthetic sequelae. As a rule of thumb, displacement of the anterior cranial vault or superior orbital rim by the full-thickness width of the bone involved is a reasonable indication that there will be postinjury aesthetic concerns prompting the need for operative intervention. Irrespective of the method of management and among the many reasons for close follow-up is the unique pediatric complication of growing skull fracture. Caused by herniation of the leptomeninges or brain at the site of dural tears even in the setting of normal intracranial pressure, physiologic growth and cerebrospinal fluid pulsations allow for development and growth of the fracture. Formal cranioplasty is necessary for repair of the defect and definitive neurosurgical care is required for management of the herniated brain tissue.
Disruption of the superior orbital roof causing direct contact of the dura with the periorbita is a significant concern. If left untreated, this may not only cause orbital pulsations but also increase intraorbital pressure. The roof itself is very thin, especially in the young child, and is often not amenable to fixation even if a large segment is left. Reconstruction of the roof with split autogenous bone grafts harvested from the calvaria remains the gold standard for treatment.
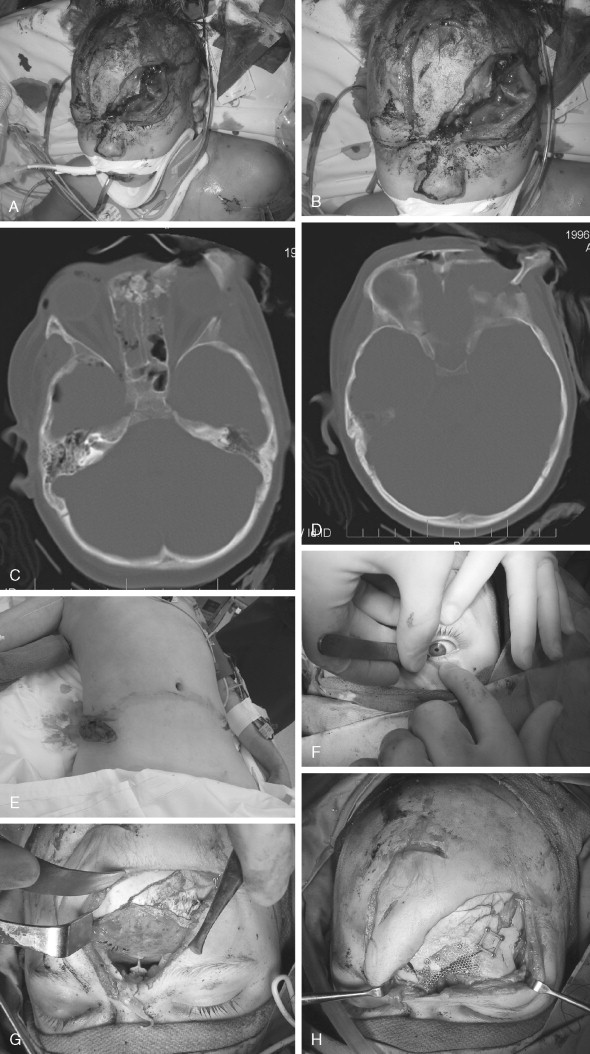
FRONTAL SINUS AND FRONTOBASILAR INJURIES
The frontal sinus, which begins as a cephalic evagination of the middle meatus, begins development around age 1 to 2 years. Radiographically, it becomes visible around age 6 to 7 years and will often continue growth until approximately age 20. The management of these injuries in children when the sinus is present is very similar to the adult patient and realistically is most often dictated by neurosurgical concerns. For posterior table fractures with dural tears, cranialization is the treatment of choice. Every effort must be made to seal the anterior cranial fossa at the conclusion of these craniofacial approaches to prevent CSF leak and minimize the risk of postoperative meningitis. Placement of a pericranial flap with autogenous bone grafts as necessary and fibrin glue on the anterior skull base is an extremely effective maneuver to isolate the anterior fossa from the face below. Osteomyelitis of the skull in children is a very rare postoperative complication, but can have devastating consequences once contracted. Maintaining the sterility and integrity of the operative field is of paramount importance. For anterior table fractures, simple elevation and stabilization is appropriate. Sinus obliteration is generally not done in children. Short-term and long-term follow-up with CT scans to rule out pathology and demonstrate sinus function are mandatory ( Figure 20-2 ).
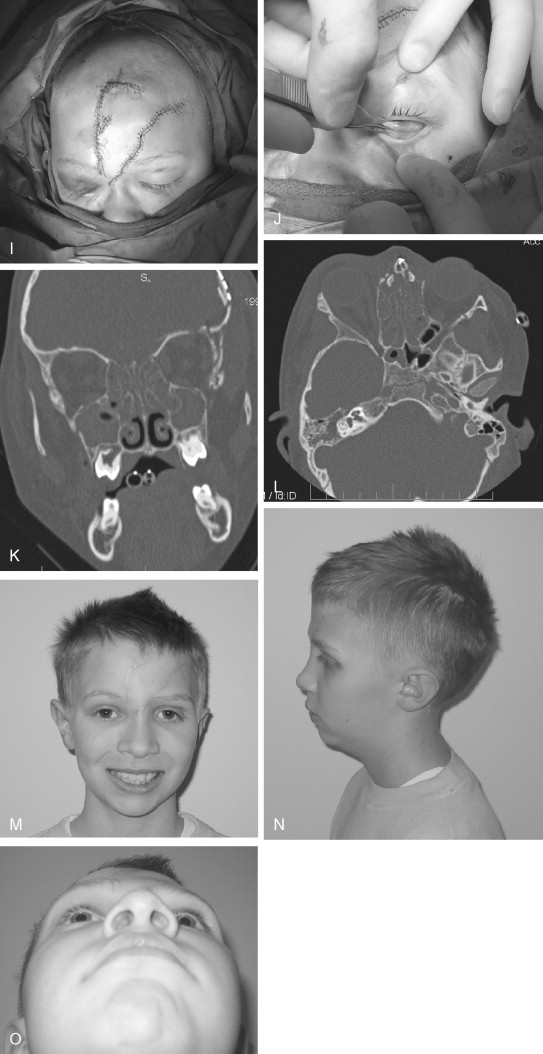
NASO-ORBITO-ETHMOID FRACTURES
The management of naso-orbito-ethmoid (NOE) fractures in children is similar to that for the adult patient. Ophthalmologic consultation is essential to rule out injury to the globe itself and the lacrimal apparatus should also be carefully evaluated. If the fractures extend into the anterior cranial fossa, neurosurgical consultation should also be obtained. If sinus drainage is interrupted by bone displacement, reduction and restoration of nasofrontal drainage is necessary. For the most part, when there is minimal displacement of the medial canthus and medial orbital fractures, NOE fractures in children can be managed closed with one caveat—the nasal reduction must be stable. If the nose can be reduced, but will not stay elevated or cannot be reduced at all, internal fixation is necessary. If the nasal reduction is stable, the use of a nasal cast to compress the tissues medially and maintain the nasal reduction is usually all that is required. Rarely, reduction of the impacted fractures will allow for CSF leakage from the previously injured anterior cranial fossa and necessitate open reduction ( Figure 20-3 ).
Open reduction and internal fixation of the fractures when necessary should be carried out through coronal incision or through an overlying laceration. Severe comminution of the nose is rare, but when present should be strut bone grafted with autogenous calvarial bone to prevent saddle-nose deformity. It is most unusual to see actual disruption of the medial canthal tendon itself, because usually it is attached to a significant fragment of bone. Care must be taken not to strip the canthal attachment from the fragment. This will allow the surgeon to reduce and plate the fracture and thus reposition the tendon. Many surgeons have found that re-creating the pretrauma contour of this region is extremely difficult and it becomes even more troublesome if formal wire canthopexy is performed. Meticulous attention should be paid to anatomic reduction of the fracture segment. Even when internal fixation is used for operative treatment, placement of a nasal cast to compress the overlying stripped soft tissues in place is very helpful in controlling nasal width and re-creating contour of the soft tissue in the region between the nose and the lacrimal lake on each side.
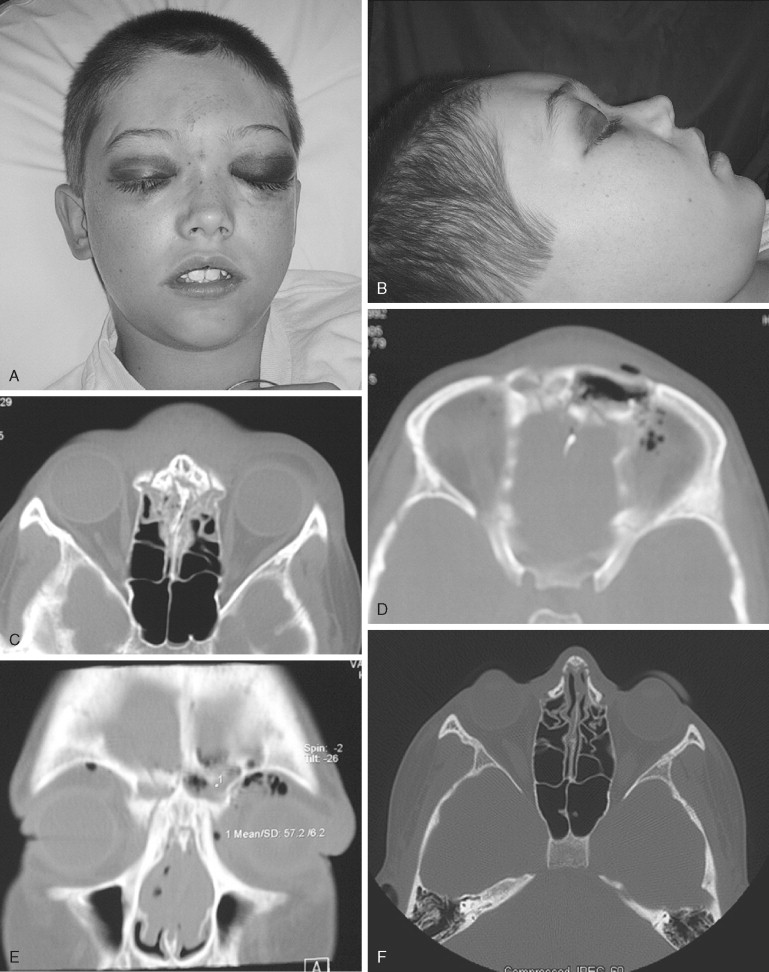
ORBITAL FRACTURES
The importance of good vision in school-age children and its correlation with academic success in the traditional setting cannot be overemphasized; experienced, timely, and appropriate surgical intervention, when required, is critical. Fractures of the orbit—whether blow-in, blow-out, or rim—are relatively common in children as previously described and can occur alone or in combination with other facial fractures. Ophthalmologic consultation is mandatory to rule out globe injury. Medicolegal considerations aside, proper intraocular examination of the globe in the setting of orbital fracture(s) in children requires specialty-level skill and experience for accurate diagnosis. While the importance of CT scanning including axial, coronal, and three-dimensional (3D) reconstructions is universally understood to constitute the gold standard for imaging in maxillofacial trauma, an important study that is often overlooked in the management of orbital fractures is the sagittal view CT scan. The authors have found this to be invaluable for evaluation and treatment of orbital floor injuries.
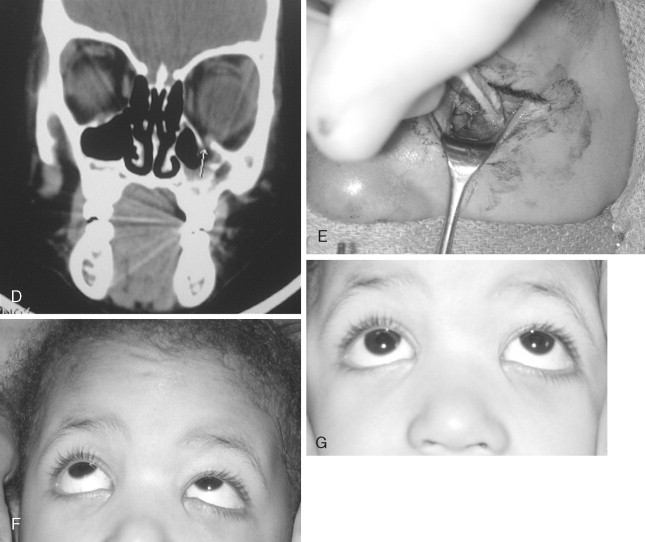
Surgical access to the orbit is no different than that in the adult patient. Overlying lacerations, if present and appropriately positioned, should be used. From an aesthetic standpoint, the transconjunctival approach to the orbit remains particularly appealing. If treatment of the orbital fracture is combined with other upper facial fractures, access to the superior, medial, and lateral walls can be achieved through the coronal incision. Blow-in fractures of the orbit should be very carefully evaluated because intraocular pressure can be increased and cause permanent injury. In addition, sharp fragments of bone protruding into the orbital cavity can further injure the globe and or extraocular muscles. Exploration and reduction of these fractures should proceed as rapidly as possible. Blow-out orbital fractures in children should be managed conservatively and nonoperatively in the case of minimal displacement, excellent globe mobility, and no ophthalmologic indications. Very often, there is little to no late enophthalmos and essentially no functional or aesthetic sequelae. In the setting of significant disruption of the orbital floor and/or inferior orbital rim, exploration and reduction of the fractures becomes necessary. The rare instance of true muscle entrapment should be regarded as a surgical emergency in children ( Figure 20-4 ). Bony entrapment of the inferior rectus muscle can cause avascular necrosis of the muscle tissue within hours of the injury. The resultant scarring of the muscle can lead to permanent visual impairment. Eye muscle repair of this problem post-injury is extremely difficult and has limited success. Management of the late post-injury enophthalmic orbit is also extremely difficult to correct and the results are often disappointing. Correction of this problem in the child is similar to that in the adult patient, with autogenous grafting.
Reconstruction of the skeletally mature orbital floor or walls, after approximately age 7 years, can be achieved through several different methods including autogenous bone, titanium mesh, or implants such as porous polyethylene, much like for an adult. Before this age, autogenous bone still remains the gold standard for orbital reconstruction because of its ability to incorporate into the skeleton. All other materials should be approached with great caution in the immature bony orbit.
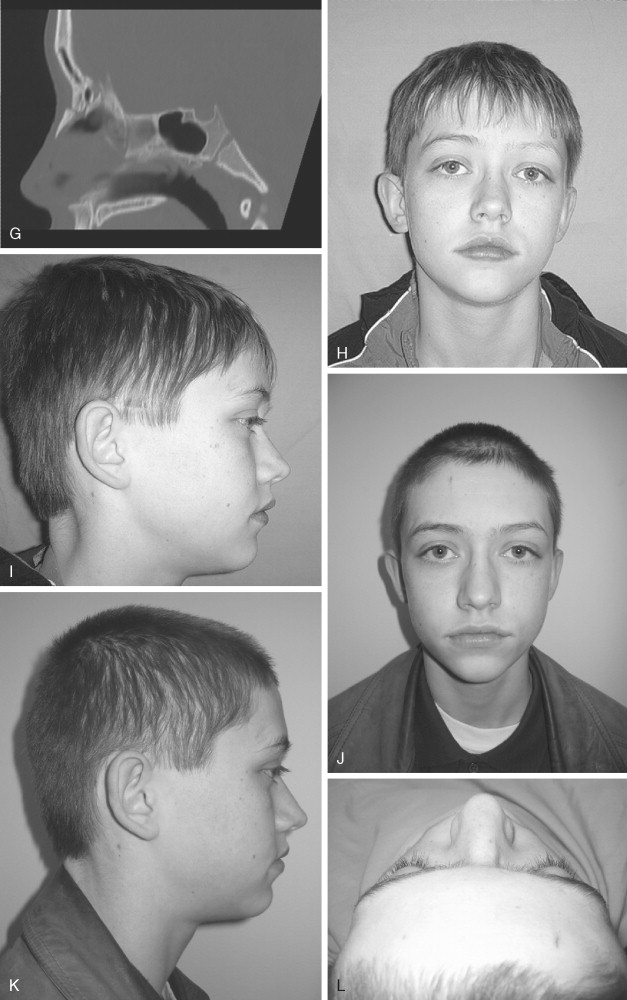
ZYGOMATICOMAXILLARY COMPLEX FRACTURES
Fractures of the malar or zygomaticomaxillary (ZMC) complex are relatively uncommon in children. When they do occur, unless associated with a high-velocity injury, more often they involve subunits rather than the entire complex. Isolated arch fractures among other variations also occur. Secondary to the orbital component, all pediatric patients with these types of fractures must also have an ophthalmologic consultation. Minimally displaced fractures with little or no loss of facial projection and no ophthalmologic concerns should be handled conservatively with nonoperative observation. For significant injuries requiring reduction and fixation, incisions for access to these fractures include the inferior orbital incisions, a superior orbital incision, and transoral vestibular access ( Figure 20-5
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


