This case report introduces a new approach of corticotomy-assisted rapid maxillary expansion for treating a severe maxillary transverse discrepancy in a skeletally mature patient. This approach uses piezo-bone perforation in conjunction with a fixed appliance and an expander. This report describes the treatment of a 14-year-old girl with a severe maxillary transverse discrepancy. She had a straight profile, severe maxillary crowding, a maxillomandibular transverse differential index of 9 mm, and a Class I skeletal relationship. The treatment protocol consisted of surgical intervention with piezo-bone perforation and active orthodontic therapy. Immediately after the piezo-bone perforation on the lateral buccal side of the maxilla, active orthodontic therapy was started with activation of an expander. The expander was reactivated weekly. Treatment duration was 5 months 2 weeks. Proper overbite and overjet, facial balance, and occlusion were achieved. The treatment outcome was stable at the 3-year follow up. This treatment approach considerably reduced the treatment time and gained bony volume. Additionally, it transformed the periodontal biotype in contrast to conventional therapy. This approach is a good alternative for treating a severe maxillary transverse discrepancy in a skeletally mature patient, especially for a patient who does not want surgical rapid palatal expansion.
Highlights
- •
Treatment duration was 5 months, with stable results at 3-year follow-up.
- •
Piezo-bone perforation induces sufficient bone apposition without bone graft.
- •
The thin periodontal biotype was transformed.
Maxillary transverse discrepancy is commonly seen in patients who seek orthodontic treatment. It is frequently defined as a unilateral or bilateral crossbite combined with anterior crowding. Several approaches are available to treat this discrepancy and achieve maxillary expansion including rapid maxillary expansion (RME), slow maxillary expansion (SME), and surgically assisted rapid palatal expansion (SARPE). The choice of treatment depends on the patient’s skeletal maturity, the amount of desired expansion, and the presence of a concomitant sagittal or vertical problem.
RME and SME are successfully used in growing patients, whereas in skeletally mature patients, SARPE is the treatment of choice. Several authors have compared the treatment outcomes and concluded that their effectiveness is similar. However, it has been reported that periodontally undesirable effects, long duration of treatment, and invasiveness are disadvantages of SARPE. Garib and Henriques and Pangrazio-Kulbersh et al demonstrated bone loss after RME with both hyrax and Haas expanders. They found that over 0.50 mm of horizontal buccal bone and attachment level were lost in all teeth analyzed after expansion. For these reasons, most orthodontists are reluctant to use these treatments for patients with a thin periodontium.
Meanwhile, corticotomy was introduced in orthodontics as an alternative treatment option for maxillary transverse discrepancy. Kole first reported the use of corticotomy in orthodontics in 1959, followed by Converse and Horowitz in 1969. Lines also reported maxillary expansion accompanied by corticotomy in 1975.
Wilcko et al reintroduced the concept in 2001 and named the patented technique “accelerated osteogenic orthodontics”; it is also called “periodontally accelerated osteogenic orthodontics.”
However, all of these authors argued that the severity of the maxillary transverse discrepancy should be considered before choosing the technique. They further stated that the treatment is indicated for mild-to-moderate transverse discrepancies. Until now, not many studies have been published on severe maxillary transverse discrepancies and severe crowding treated with a corticotomy.
The aim of this article is to introduce a new approach to corticotomy-assisted RME to overcome the limitation of expansion for a severe maxillary transverse discrepancy in skeletally mature patients. This approach involves the use of piezo-bone perforation with fixed appliances and an expander.
Diagnosis and etiology
The patient was a 14-year-old Moroccan girl with chief complaints of an unsightly dental appearance and a narrow smile with dark corners. Her medical history showed no nasal obstruction or allergies that might have contributed to the malocclusion. The functional examination showed a lingual interposition during swallowing.
The extraoral examination showed a well-balanced and symmetric face. Her profile was straight. Her lips were incompetent at rest and slightly inverted on closure. The maxilla was mildly retruded with an increased lower anterior facial height ( Fig 1 ). No signs or symptoms of a temporomandibular joint disorder were noted.

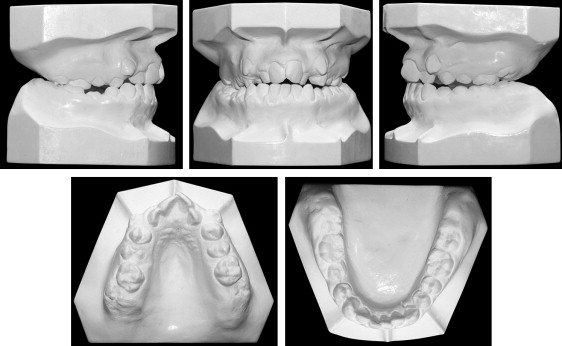
The intraoral examination showed fair oral hygiene with a thin periodontium especially around the canines, mandibular incisors, and maxillary right premolars. The thin, inflamed gingiva around the canines was due to a prominent root and labial ectopic eruption on the mucogingival junction. Pocket depths ranged between 1 and 2 mm. Her maxillary arch had anterior and bilateral crossbites with severe anterior crowding, and the mandibular arch had moderate crowding with a moderate curve of Spee. The molar relationships were Class I on the right and Class II on the left. The canine relationships were Class II on both sides with an overjet of −1 mm and an overbite of 0 mm. The maxillary midline coincided with the facial midline. The mandibular dental midline deviated by 2.0 mm to the right because of the unstable occlusal contacts ( Fig 1 ).
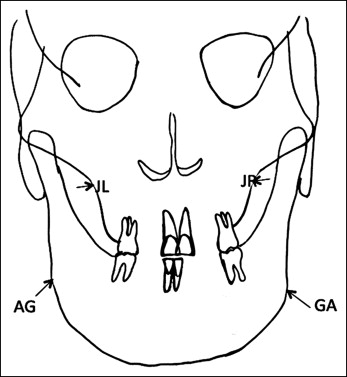
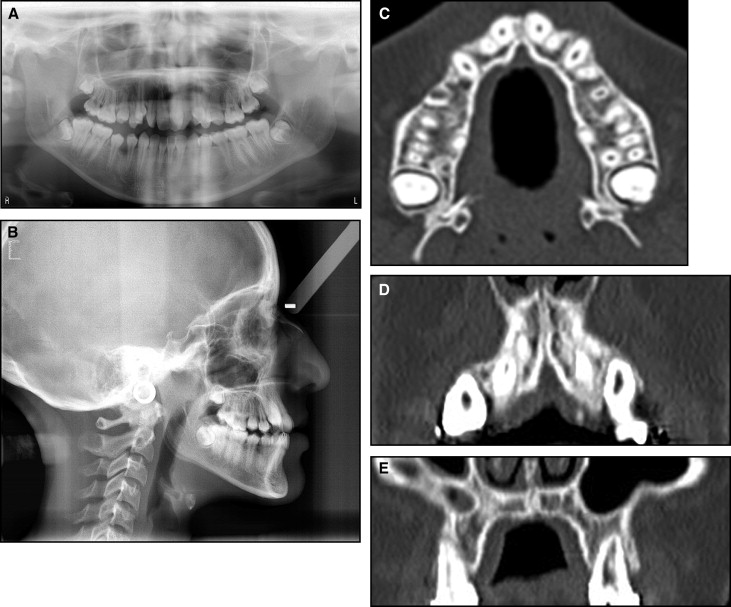
Analysis of the dental casts confirmed the Class II canine relationship ( Fig 2 ). The maxillary arch was symmetrical with 17 mm of crowding and constriction (interfirst premolar width, 33.7 mm; intersecond premolar width, 40.5 mm; interfirst molar width, 45.6 mm) ( Fig 2 ; Table I ). The maxillomandibular differential transverse index was 9 mm ( Fig 3 ). No teeth were missing, including the 4 third molars on the pretreatment panoramic radiograph. The patient had no fillings, carious lesions, or periodontal defects ( Fig 4 , A ). In comparison with the Moroccan norm, a skeletal Class I relationship (ANB angle, 1°) with maxillary retrusion (SNA angle, 76°) was observed. The mandibular plane angle was high (GoGn-SN, 40°). The position of the maxillary incisors was close to the norm (U1-Na, 22°), but the mandibular incisors were lingually inclined (IMPA, 79°), and the interincisal angle was excessive (U1-L1, 140°). The occlusal plane angle was steep (11°) ( Fig 4 , B ; Table II ). The lateral cervical vertebrae on the cephalometric radiograph showed that the patient had passed her growth peak. A computed tomography (CT) scan of the pretreatment axial and coronal slices showed extremely thick alveolar processes in the buccal areas, especially on the maxillary canines and right second premolar ( Fig 4 , C-E ).
| Pretreatment, T0 (14 y) | After RME, T1 (14 y 2 mo) | Posttreatment, T2 (14 y 5 mo) | 3 years retention, T3 (17 y 5 mo) | T1–T0 | T2–T1 | T2–T3 | T2–T0 | T3–T0 | T3–T1 | |
|---|---|---|---|---|---|---|---|---|---|---|
| Maxilla | ||||||||||
| Intercanine width | 35.3 | 36.5 | 35.3 | 35.3 | 1.2 | −1.2 | 0 | 0 | 0 | −1.2 |
| Interfirst premolar width | 33.7 | 44.3 | 43.7 | 43.7 | 10.6 | −0.6 | 0 | 10 | 10 | −0.6 |
| Intersecond premolar width | 40.5 | 49.6 | 49.4 | 48.7 | 9.1 | −0.2 | −0.7 | 8.9 | 8.2 | −0.9 |
| Interfirst molar width | 45.6 | 54 | 53.9 | 53.9 | 8.4 | −0.1 | 0 | 8.3 | 8.3 | −0.1 |
| Intersecond molar width | 55.6 | 59.7 | 59.7 | 59.7 | 4.1 | 0 | 0 | 4.1 | 4.1 | 0 |
| Mandible | ||||||||||
| Intercanine width | 25.7 | 27.9 | 27.6 | 27.6 | 2.1 | −0.3 | 0 | 1.9 | 1.9 | −0.3 |
| Interfirst premolar width | 34.5 | 34.8 | 34.9 | 34.9 | 0.3 | 0.1 | 0 | 0.4 | 0.4 | 0.1 |
| Intersecond premolar width | 40.7 | 40 | 40.5 | 40.1 | −0.7 | 0.5 | −0.4 | −0.2 | −0.6 | 0.1 |
| Interfirst molar width | 47.2 | 46.4 | 46.3 | 46.2 | −0.8 | 0.1 | −0.1 | −0.9 | −1 | −0.2 |
| Intersecond molar width | 48.8 | 49.8 | 49.8 | 49.8 | 1 | 0 | 0 | 1 | 1 | 0 |
| Measurement | Average ∗ | SD | Pretreatment, T0 | Posttreatment, T1 | Three-year retention, T2 |
|---|---|---|---|---|---|
| Skeletal | |||||
| SNA (°) | 81.33 | 3.62 | 76 | 74 | 74 |
| SNB (°) | 78.44 | 3.52 | 75 | 73 | 73 |
| ANB (°) | 2.90 | 2.31 | 1 | 1 | 1 |
| Wits (mm) | −1.33 | 2.55 | −1 | −2 | −2 |
| GoGn-SN (°) | 35.17 | 5.53 | 40 | 40 | 40 |
| Occ-Fr (°) | 8.68 | 4.09 | 11 | 11 | 11 |
| FMA (°) | 21.94 | 5.84 | 30 | 31 | 30 |
| Dental | |||||
| L1-MP (°) | 96.47 | 6.78 | 79 | 90 | 90 |
| U1-NA (°) | 21.71 | 6.21 | 22 | 26 | 24 |
| U1-NA (mm) | 4.46 | 2.35 | 5 | 5 | 5 |
| L1-NB (°) | 29.32 | 5.93 | 16 | 27 | 25 |
| L1-NB (mm) | 6.16 | 2.30 | 3 | 6 | 5 |
| U1-L1 (°) | 124.48 | 9.53 | 140 | 129 | 131 |
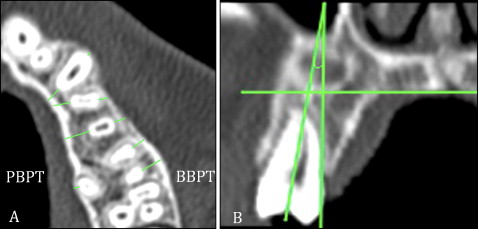
The OsiriX MD software (OsiriX, Geneva, Switzerland) was used to calculate the following parameters: buccal alveolar bone thickness, palatal alveolar bone thickness, and tooth inclination. The alveolar bone thickness measurements were made at the root apex and at the middle of the root levels of the maxillary first molars, premolars, and canines ( Fig 5 , A ). Tooth inclinations were measured on the coronal reconstructions through the angle formed by the long tooth axis and the line perpendicular to the palatal plane for the maxillary first molars and premolars ( Fig 5 , B ).
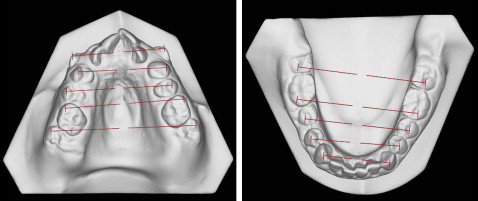
Three-dimensional scanning of the plaster models was performed using the Bibliocast D-Viewer (version 2.0; Bibliocast, Montreuil, France) to assess the amounts of treatment changes in the intercanine, interpremolar, and intermolar widths in both arches ( Fig 6 ). The 3-dimensional superimposition was carried out using surface-to-surface matching (best-fit method) with Rapidform 2002 (INUS Technology, Seoul, South Korea).
Treatment objectives
The treatment objectives were to resolve the maxillary transverse discrepancy by expanding the maxilla, correct the anterior crossbite, obtain ideal overjet and overbite, provide canine guidance in lateral excursions and incisal guidance in protrusive movements, correct the midline discrepancy, obtain Class I dental relationships in the canines and molars, and improve the patient’s appearance.
Treatment alternatives
Because of the complexity of this case, the patient was meticulously assessed with a CT scan, digital models, cephalograms, and a periodontal examination. To assist in her treatment planning, all available treatment options were evaluated before deciding on the most suitable one for the patient. The following 4 options were examined.
The optimal option was SARPE with fixed orthodontic appliances. It was the treatment of choice because of the high maxillomandibular differential transverse index (9 mm). In this option, the palatal suture can be opened widely, resulting in sufficient expansion of the constricted maxillary arch to create space to correct the severe crowding. However, the patient and her parents did not want this option because of the costs, invasiveness, and need for general anesthesia.
The second option relied only on orthodontic treatment with RME and fixed appliances. This option corrects the maxillary constriction first and resolves the crowding later. However, this option can cause detrimental effects on the periodontium, and the treatment outcome may not be stable because of the high maxillomandibular differential transverse index (9 mm), the patient’s skeletal maturation, and the thin periodontium. It was reasonable to avoid compromising her periodontal health and long-term stability. Consequently, this option was abandoned.
The third option also depended only on orthodontic treatment with SME and passive self-ligating appliances. The constricted maxilla could be expanded, and the severe crowding could be corrected. Because the patient was still an adolescent, bone loss would not be expected. However, she requested a shorter treatment time because she was sensitive about her appearance at school and in daily life. Therefore, this option was not chosen. Extraction was excluded in all of these treatment options because of her straight profile, which would have been aggravated by extractions.
The last option was a corticotomy-assisted RME. It was expected to be challenging to obtain significant amounts of expansion in a short period of time with this option. Although expansion is performed rapidly, a corticotomy-assisted RME can maintain periodontal health with less invasiveness to the tissues than SARPE. Corticotomy-assisted RME is not usually indicated for a severe maxillary constriction. Since periodontal health was a chief parameter and the patient wanted to finish the treatment quickly, the corticotomy-assisted RME was considered the most viable treatment modality. A novel approach of corticotomy-assisted RME was proposed to resolve the severe maxillary constriction and crowding while minimizing the detrimental effects on the periodontium. Our protocol combined multiple techniques with slight modifications to meet the requirements of this case. RME was planned to be performed after surgical activation with the corticotomy. Passive self-ligating brackets were recommended to reduce the time to change the archwires. Finally, the corticotomy was used with biomechanical and surgical-periodontal approaches after meticulous evaluation of the case. The patient’s parents and the patient accepted the corticotomy-assisted RME.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


