Although 2-jaw orthognathic surgery is a typical recommendation for the treatment of facial asymmetry, another good treatment alternative is maxillary corticotomy with temporary skeletal anchorage devices followed by mandibular orthognathic surgery. The corticotomy procedure described here can achieve unilateral molar intrusion and occlusal plane canting correction with potentially fewer complications than 2-jaw orthognathic surgery. The approach allows movement of dentoalveolar segments in less time than with conventional dental intrusion using temporary skeletal anchorage devices. A 2-jaw asymmetry with occlusal plane canting might be corrected using maxillary corticotomy and mandibular orthognathics rather than 2-jaw orthognathics. Two patients with facial asymmetry are presented here. In each one, the maxillary cant was corrected over a period of 2 to 3 months with 3.5 mm of intrusion of the unilateral buccal segment. After the preorthognathic cant correction, orthognathic surgery was done to correct the mandibular asymmetry.
Highlights
- •
Maxillary canting correction is achieved by maxillary corticotomy combined with temporary skeletal anchorage devices.
- •
Maxillary corticotomy and 1-jaw surgery is a good treatment option for facial asymmetry.
Facial asymmetry is one reason that patients seek orthognathic surgery combined with orthodontic treatment. Common features of facial asymmetry include a mandibular deviation to the right or left that increases gradually from the upper to the lower face. This is usually associated with a cant of the maxilla and the maxillary occlusal plane. Severt and Proffit reported that the frequencies of facial asymmetry are 5%, 36%, and 74% in the upper, middle, and lower thirds of the face, respectively. In such cases, dramatic improvement of facial balance comes with surgery to the mandible. Correction of the maxillary cant is usually a prerequisite. Consequently, correction typically includes a combination of LeFort I osteotomy and bilateral sagittal split ramus osteotomy.
Case reports have been published demonstrating nonorthognathic correction of the maxillary cant before orthognathic surgery. Posterior bite-blocks or high-pull headgear has been used to intrude the molars conventionally. Both of these methods require significant patient cooperation. With either method, it is difficult to control the direction and quantity of tooth movement. With the advent of temporary skeletal anchorage devices (TSADs), orthodontic molar intrusion and occlusal plane canting correction have been reported, with minimal surgical intervention. Kang et al introduced a rhythmic arch system using TSADs and obtained a considerable amount of canting correction. Jeon et al reported correction of mandibular prognathism with mandibular surgery only, correcting the maxillary asymmetry by intrusion of the maxillary molars unilaterally using TSADs. However, the treatment times were extended, increasing the risk of side effects.
Since Köle suggested clinical applications of corticotomy in 1959, various technical advancements have been reported. One is orthopedic force application against intraosseous anchorage after corticotomy. A heavier force is applied than the orthodontic force because the aim of this technique is not tooth movement through the bone but rather bony block movement by compression osteogenesis. If the cortical layer of the basal and alveolar bone is removed, medullary bone can be bent by traction force.
We have called the combination of corticotomy and orthopedic force application using TSADs speedy surgical orthodontics (SSO). By using this protocol, correction of a significant facial asymmetry can be achieved with single-jaw surgery. Omitting the corticotomy element means slower correction and lacks the correction of the supporting bone that corticotomy allows. This report includes 2 patients who demonstrate the clinical application of correcting an occlusal plane cant with corticotomies and orthopedic force.
Overerupted maxillary molars and premolars are first passively splinted with a prefabricated bondable splint. This splint consists of a 0.036-in stainless steel wire with a power arm extension, soldered to mesh-backed pads. Bonding these splints to the buccal and palatal aspects of the teeth stabilizes the teeth as 1 unit. The corticotomy procedure can be done after the teeth are stabilized.
The corticotomies were performed in 2 stages to ensure a good blood supply. The first was done on the palatal side. The second was done 2 weeks later on the buccal side ( Fig 1 ).
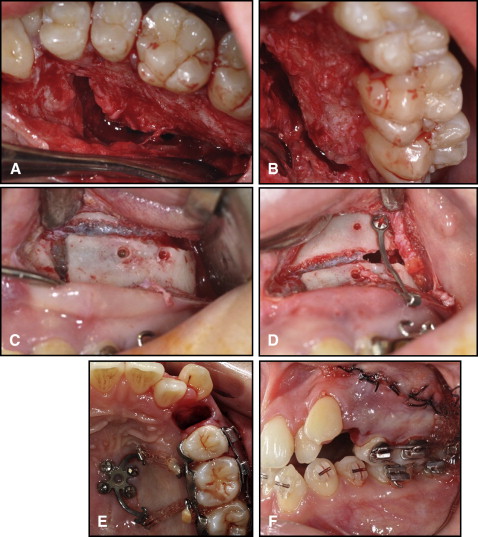
For the palatal corticotomy, a flap was elevated in the regions of the maxillary premolars and molars after a sulcular incision. A vertical corticotomy using piezosurgery and a round bur with a slow-speed hand piece was performed between the first premolar and the second premolar with care not to damage the root apices. A horizontal corticotomy was next, 3 mm above the root apex from the premolars to the distal aspect of the second molar. A second vertical corticotomy was performed distal to the second molar up to the alveolar crest ( Fig 1 , A and B ). The flap was closed, followed by a 2-week healing period.
The buccal corticotomy was combined with placement of the TSADs and extraction of the maxillary first premolar (part of the treatment plan to resolve crowding). The palatal corticotomy outline is similar to that on the buccal aspect ( Fig 1 , C and D ). On the midpalatal area, a miniplate with 2 horizontal arms (Jin Biomed, Bucheon, Korea) that were oriented toward the target teeth was implanted on the midpalatal area for palatal intrusion. Flap surgery was not necessary because the soft tissues on the midpalatal area were thin ( Fig 1 , E ). On the buccal side between the first and second molar areas, we placed an I-shaped titanium C-tube plate, with 2 anchoring holes and a 0.036-in diameter tube-shaped head, to serve as the point of orthodontic force application ( Fig 1 , F ). With elastic chain, 500 g of force was applied to intrude the posterior segment immediately after the perisegmental corticotomy. At the same time, the maxillary canine was retracted into the extraction site ( Fig 1 , F ).
Patient 1
A 15-year-old girl came to the Kyung Hee dental hospital in Seoul, Korea, with the chief complaint of facial asymmetry. She had a straight lateral profile, mesognathic facial type, eye-level canting (right side down), lip-line canting (right side high), chin deviation to the right, and an acceptable display of her maxillary anterior teeth ( Fig 2 , A ). The intraoral photographs showed an Angle Class I malocclusion, severe anterior crowding, an ectopically positioned maxillary left canine, a mandibular dental midline discrepancy to the right, and transverse compensation of the maxillary and mandibular molars ( Fig 2 , B ).

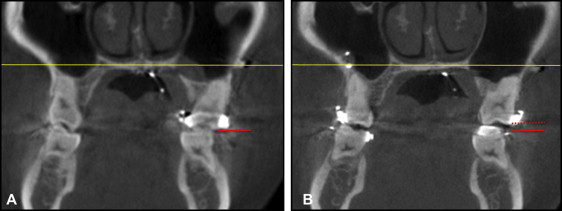
The cephalometric analysis indicated a hyperdivergent skeletal pattern (FMA, 32.8°), normal relationships of the maxilla (SNA, 80.7°) and the mandible (SNB, 77.9°), maxillary occlusal plane cant (left side down), menton deviation to the right side (7.0 mm), and upright maxillary and mandibular incisors (U1-FH, 108.2°; IMPA, 81.9°) ( Fig 3 and Table ). Although her condyle was thin and narrow, especially on right side, there was no clinical symptom of temporomandibular disorder or a centric occlusion-centric relation discrepancy. On the axial cut of the cone-beam computed tomography (CBCT) images (Alphard Vega; Asahi Roentgen, Kyoto, Japan), the vertical height difference of the buccal cusp tips between the maxillary left and right first molars was about 3.5 mm, and both buccal cusp tips had abnormal torque because of the transverse compensation ( Fig 4 , A ). The torque would be evaluated after the cant correction. Accordingly, the diagnosis was a Class I skeletal relationship, steep mandibular plane angle, facial asymmetry, and severe crowding.

| Measurement | Mean | SD | Pretreatment | Posttreatment |
|---|---|---|---|---|
| Skeletal-horizontal | ||||
| SNA (°) | 81.6 | 3.2 | 80.7 | 80.7 |
| SNB (°) | 79.2 | 3.0 | 77.9 | 76.1 |
| ANB (°) | 2.5 | 1.8 | 2.8 | 4.6 |
| Skeletal-vertical | ||||
| PFH/AFH (%) | 66.8 | 4.3 | 59.9 | 58.1 |
| FMA (°) | 25.4 | 4.6 | 32.8 | 36.4 |
| SN-OP (°) | 17.9 | 3.8 | 21.2 | 24.6 |
| SN To PP (°) | 10.2 | 3.2 | 9.8 | 10.0 |
| Dental | ||||
| FH-UI (°) | 116.0 | 5.7 | 108.2 | 116.5 |
| IMPA (°) | 95.9 | 6.4 | 81.9 | 88.9 |
| Interincisal angle (°) | 123.8 | 8.3 | 137.0 | 117.9 |
| FMIA (°) | 59.8 | 7.2 | 65.2 | 54.5 |
| Soft tissue | ||||
| Nasolabial angle (°) | 93.2 | 8.0 | 97.2 | 96.1 |
| UL-E plane (mm) | -0.9 | 2.2 | -1.7 | -0.2 |
| LL-E plane (mm) | 0.6 | 2.3 | -0.7 | 0.7 |
The treatment objectives were correction of the facial asymmetry, elimination of crowding of the maxillary and mandibular dentition, and establishment of a normal occlusion. The canting extended to the orbit, correction of which was not part of the treatment plan. We set a goal to correct the facial asymmetry below the LeFort I level and initially planned 2-jaw surgery. However, the patient wanted to minimize the expense and scope of the surgical intervention. Fortunately, she had a normally positioned maxilla anteroposteriorly and a dental midline coincident with the facial midline. The alternative plan she selected was a bilateral sagittal split ramus osteotomy after SSO maxillary cant correction with a unilateral corticotomy. Because the maxillary incisors were upright and the maxillary left canine was blocked, the plan included unilateral extraction of the left first premolar. Corticotomies on both sides were performed as described, and an orthopedic intrusion force was immediately applied.
In 3 months, intrusion of the maxillary left posterior segment was complete. To prevent extrusion of the opposing teeth, a resin bite-block was added on the left mandibular molars. CBCT scans and superimposition of the cephalograms confirmed 3.5 mm of intrusion of the maxillary left molars ( Fig 4 , B ). The buccal and lingual bonded mesh appliances were removed, and brackets (Quicklear; Forestadent, Pforzheim, Germany) were placed on the maxillary teeth for further leveling and alignment. Cross elastics were used between the TSADs on the maxillary arch and the mandibular molars for transverse decompensation.
After the preoperative orthodontic treatment, the midline of the maxillary dentition coincided with the facial midline, and the maxillary occlusal canting and the transverse decompensation were corrected ( Figs 5 and 6 ). An asymmetric mandibular setback was then performed with bilateral sagittal split ramus osteotomy. Orthodontic treatment was resumed 6 weeks postsurgery and was completed after 5 months. The total active treatment period was 22 months. At debonding, the extraoral photographs showed a distinct improvement of the facial symmetry and a beautiful smile line ( Fig 7 , A ). The single-jaw surgery alone achieved good facial symmetry even in the middle face level. In the maxilla, the facial gingival line showed mild asymmetry because of the gingival height of the maxillary left canine. The maxillary left canine was positioned higher before treatment and moved significantly both downward and in a distal direction after unilateral extraction of the first premolar; this might have been responsible for the difference in crown length. The dental midlines of the maxilla and the mandible coincided with the facial midline. A Class I functional occlusion with ideal overjet and overbite was obtained ( Fig 7 , B ). No significant root resorption was evident in the panoramic radiograph. The posttreatment lateral cephalometric analysis and superimposition showed good inclination of the maxillary and mandibular incisors (U1-FH, 116.5°; IMPA, 88.9°) and a favorable maxillomandibular relationship ( Fig 8 ). The occlusal plane was greater by 3° than before treatment (SN-OP, 21.2° to 24.6°). The treatment results were well maintained at 8 months after debonding ( Fig 9 ).





