Introduction
Pharyngeal airway size is increasingly recognized as an important factor in obstructive sleep apnea. However, few studies have examined the changes of pharyngeal airway form after dental procedures for treating obstructive sleep apnea during growth. The purpose of this study was to evaluate the effect of the Herbst appliance on the 3-dimensional form of the pharyngeal airway using cone-beam computed tomography.
Methods
Twenty-four Class II subjects (ANB, ≥5°; 11 boys; mean age, 11.6 years) who required Herbst therapy with edgewise treatment had cone-beam computed tomography images taken before and after Herbst treatment. Twenty Class I control subjects (9 boys; mean age, 11.5 years) received edgewise treatment only. The volume, depth, and width of the pharyngeal airway were compared between the groups using measurements from 3-dimensional cone-beam computed tomography images of the entire pharyngeal airway.
Results
The increase of the oropharyngeal airway volume in the Herbst group (5000.2 mm 3 ) was significantly greater than that of the control group (2451.6 mm 3 ). Similarly, the increase of the laryngopharyngeal airway volume in the Herbst group (1941.8 mm 3 ) was significantly greater than that of the control group (1060.1 mm 3 ).
Conclusions
The Herbst appliance enlarges the oropharyngeal and laryngopharyngeal airways. These results may provide a useful assessment of obstructive sleep apnea treatment during growth.
Highlights
- •
Herbst therapy led to increases in pharyngeal airway volume in boys with Class II malocclusion.
- •
Depth of the oropharyngeal and laryngopharyngeal airways increased.
- •
Width of the oropharyngeal airway increased.
- •
Herbst appliance therapy might be useful for patients with obstructive sleep apnea.
Upper airway narrowing is implicated in the development of obstructive sleep apnea (OSA). The importance of this obstruction during growth is increasingly recognized. Accordingly, much attention has been paid to the influence of maxillofacial form on respiratory function during growth. Some studies have suggested that a vertical growth pattern, with obstruction of the pharyngeal airway, is associated with mouth breathing. Pharyngeal airway obstruction is expected to improve with forward jaw movement such as that after maxillomandibular advancement surgery or the use of a mandibular advancement oral appliance. Based on computed tomography images, Fairburn et al reported that maxillomandibular advancement surgery appears to enlarge the lateral and anteroposterior pharyngeal airway diameters from the level of the hard palate to the hyoid bone.
The Herbst appliance is a fixed bite-jumping device for treating Class II malocclusion. The active treatment is relatively brief and requires little or no patient cooperation. Because the pharyngeal airway is expanded anteriorly as a secondary effect of the Herbst appliance, improvement of pharyngeal airway obstruction would be expected. Schutz et al reported that pharyngeal airway volume increases when a Herbst appliance and a rapid maxillary expander are used together, resulting in relief of OSA symptoms. However, they did not evaluate the 3-dimensional (3D) airway enlargement effects of the Herbst appliance alone. Also, changes during the posttreatment period were not examined. Hence, there is still no evidence that treatment with the Herbst appliance permanently enlarges the pharyngeal airway.
The purpose of this study was to use cone-beam computed tomography (CBCT) to evaluate the 3D changes of the pharyngeal airway produced by the Herbst appliance.
Material and methods
A total of 44 patients who visited a private orthodontic office (Himeji, Japan) for orthodontic treatment were screened for this longitudinal retrospective study. This study was approved by the ethics committee of the Graduate School of Medical and Dental Sciences of Kagoshima University, Kagoshima, Japan. Because the volume of the airway is influenced by head posture, the craniocervical inclination angles of all subjects were examined to ensure that they were between 90° and 105°. The criteria for selection to the Herbst group included (1) Class II Division 1 malocclusion, with greater than half-step Class II molar and canine relationships; (2) Class II skeletal relationship (ANB, ≥5°); (3) growing children (ages, 9-14 years); (4) no rapid maxillary expansion or treatment with a quad-helix appliance either before or during Herbst treatment; (5) no previous functional appliance treatment for skeletal disharmony; (6) no craniofacial anomalies or other growth disturbances; (7) no impacted teeth; and (8) CBCT data (not routine) that were needed for diagnosis before and after Herbst treatment. The control group subjects were closely matched for sex, age, and FMA angle with the Herbst subjects. The criteria for selection of the control group included (1) Class I malocclusion; (2) Class I skeletal relationship (2° ≤ANB ≤4°); (3) growing children (9-14 years); (4) no use of any adjunctive appliance such as a quad-helix, functional appliance, or rapid palatal expander as part of their orthodontic treatment; (5) no craniofacial anomalies or other growth disturbances; (6) no impacted teeth; and (7) CBCT data (not routine) that were needed for a diagnosis of orthodontic treatment at corresponding times (ie, before and after Herbst treatment). Both groups were treated consecutively with fixed edgewise appliances and had good occlusion—Class I molar and canine relationships and adequate overbite (2-4 mm) and overjet (1-3 mm) at the end of treatment. There was no clear airway difficulty or sleep breathing disorder in any study patient.
The control group had CBCT scans taken before and after fixed appliance therapy, whereas the Herbst appliance group had their CBCT scans taken before Herbst therapy and after fixed appliance treatment. The Herbst group consisted of serial CBCT images of 24 subjects (11 boys, 13 girls) with mean ages before and after treatment of 11.64 ± 0.94 years and 15.14 ± 1.50 years, respectively. No passive retention appliance was used before full orthodontic treatment. The mean treatment time with the Herbst appliance was 12.3 ± 4.2 months. The control group consisted of serial CBCT images of 20 subjects (9 boys, 11 girls) without Herbst appliance treatment. The control CBCT images were taken at 11.54 ± 0.72 years of age (before) and 14.94 ± 0.69 years of age (after) treatment. Using cephalogram images constructed from the CBCT data, we evaluated growth conditions from bone age of the cervical spine. Bone age of the 2 groups was matched both before and after treatment. Also, bone age before treatment in both groups was before the growth spurt; after treatment, it was after the growth spurt in both groups.
Each subject was seated in a chair with his or her Frankfort horizontal plane parallel to the floor. Each subject was asked to hold his or her breath at the end of expiration, without swallowing, because the pharyngeal airway caliber when awake is smallest at this time. This position is stable and has a high reproducibility for measurement. A CBCT scanner (Alphard-3030; Asahi Roentgen Industrial, Kyoto, Japan) was set to maximum 80 kV, maximum 2 mA, and exposure time of 17 seconds. The data were sent directly to a personal computer and stored in DICOM format.
A 3D coordinate system and 3D image were constructed with a medical image analyzing system (Imagnosis VE; Imagnosis, Kobe, Japan). The origin of the 3D coordinate system was the midpoint between the left and right porion points. This origin, and the left and right orbitale points, defined the standard horizontal plane. A frontal plane was constructed through both orbitale points perpendicular to the horizontal plane. The sagittal plane was constructed through both orbitale midpoints perpendicular to the horizontal and frontal planes.
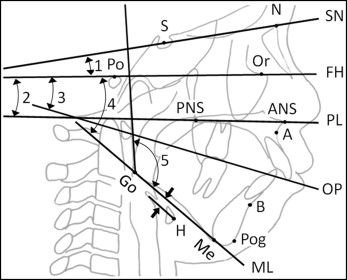
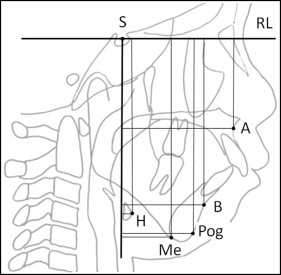
Cephalometric images were reconstructed from the CBCT data to assess growth during treatment using both traditional cephalometric measurements and the vertical and horizontal movements of selected landmarks. The definitions of landmarks, reference planes, and cephalometric angular measurements are shown in Figure 1 . The horizontal (x) and vertical (y) movements of the selected landmarks were described based on coordinates relative to a reference plane parallel to the Frankfort horizontal and passing through sella, with sella as the origin ( Fig 2 ).
To evaluate the pharyngeal airway, the length, cross-section, and volume of the pharyngeal airway were measured ( Figs 3-5 ). Volume rendering software (INTAGE Volume Editor; Cybernet, Tokyo, Japan) was used to create the 3D images manually and to evaluate the pharyngeal airway.

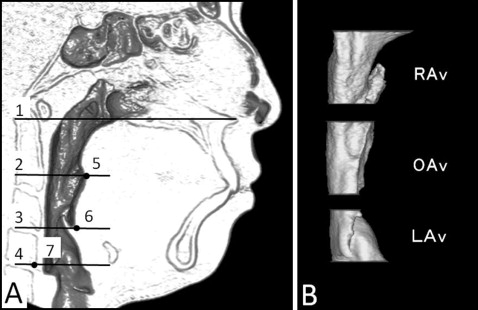
The pharyngeal airway length ( Fig 3 ) was measured from the posterior nasal spine to the upper margin of the hyoid bone (corresponding to the vallecula and epiglottis base, respectively).
For the cross-sectional planes ( Fig 4 , A ), the following planes were used to segment the airway into regions: (1) palatal plane (PL plane), a plane parallel to the hard palate passing through the posterior nasal spine; (2) soft palatal plane (SP plane), a plane parallel to the PL plane passing through the most inferior point on the uvula; (3) base of the epiglottis plane (EB plane), a plane parallel to the PL plane passing through the base of the epiglottis; and (4) C4 pharyngeal plane (C4 plane), a plane parallel to the PL plane passing through the most inferior anterior point of the fourth cervical vertebra.
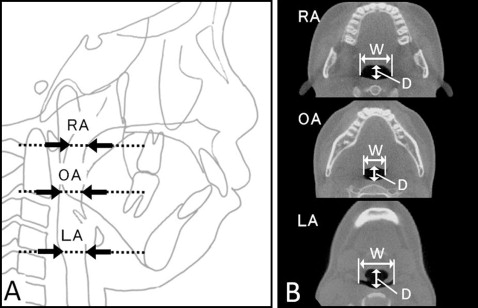
Pharyngeal airway cross-sectional measurements included depth (anteroposterior direction) and width (left-right direction) ( Fig 5 ): (1) retropalatal airway (RA) cross-section was measured parallel to the PL plane at the airway’s narrowest part on the cephalometric image; (2) oropharyngeal airway (OA) cross-section was measured along the PL plane passing through the midpoint of gonion bilaterally; and (3) laryngopharyngeal airway (LA) cross-section was measured along the C4 plane.
Although these cross-sections are not directly perpendicular to the long axis of the pharyngeal airway, the PL plane was used as a reference plane to standardize the plane orientation and minimize errors in identifying the studied cross-sectional planes of the subjects.
The following pharyngeal airway volumes ( Fig 4 , B ) were measured: (1) total pharyngeal airway volume (TAv), airway between the PL plane and the C4 plane; (2) retropalatal airway volume (RAv), airway between the PL plane and the SP plane; (3) oropharyngeal airway volume (OAv), airway between the SP plane and the EB plane; and (4) laryngopharyngeal airway volume (LAv), airway between the EB plane and the C4 plane.
Statistical analysis
For each measurement, a Mann-Whitney U test was used to compare differences between the Herbst and control groups. For all tests, P <0.05 was considered statistically significant.
To calculate the β error, a power analysis was performed (1 − β error = 0.80; α = 0.05, 2-tailed test). Because of slightly undersized samples, the results had a small chance of accepting a false hypothesis.
All measurements were repeated after 1 week by the same investigator (T.I.), and Dahlberg’s formula was used for the calculation of the measurement error. The measurement errors for the cephalometric images were from 0.389° to 0.543°, and 0.421 mm. Method error values of the pharyngeal cross-sections and volumes were from 0.21 to 0.31 mm, and from 0.07 to 0.27 mm 3 , respectively. According to all repeated analyses, the method error was considered negligible.
Results
The cephalometric variables in the Herbst and control groups before treatment are compared in Table I . The SNB angle in the Herbst group was significantly smaller than that in the control group. The ANB and SN-FH angles in the Herbst group were significantly larger than those of the control group. The horizontal cephalometric landmarks describing the positions of the maxilla and the mandible did not differ significantly between the groups. The vertical cephalometric landmarks—A(y) and B(y)—were significantly smaller than those of the control group.
| Before | After | Treatment and growth changes | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Herbst | Control | P | Herbst | Control | P | Herbst | Control | P | |||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | ||||
| Angles (°) | |||||||||||||||
| SNA | 81.48 | 3.13 | 81.40 | 2.85 | 0.931 | 80.25 | 2.49 | 81.35 | 2.98 | 0.189 | −1.23 | 2.60 | −0.05 | 1.88 | 0.098 |
| SNB | 74.60 | 2.76 | 78.10 | 3.01 | 0.000 ∗ | 76.40 | 2.99 | 78.35 | 2.89 | 0.034 ∗ | 1.79 | 2.13 | 0.25 | 1.62 | 0.011 ∗ |
| ANB | 6.88 | 1.84 | 3.30 | 0.80 | 0.001 ∗ | 3.85 | 1.43 | 3.00 | 0.92 | 0.027 ∗ | −3.02 | 1.39 | −0.30 | 0.73 | 0.001 ∗ |
| SN-FH | 9.15 | 2.43 | 7.25 | 2.43 | 0.013 ∗ | 8.46 | 2.32 | 6.95 | 2.46 | 0.043 ∗ | −0.69 | 2.64 | −0.30 | 1.89 | 0.587 |
| FH-PL | 0.15 | 2.92 | 1.63 | 2.19 | 0.069 | 0.38 | 2.86 | 1.40 | 2.58 | 0.222 | 0.23 | 2.19 | −0.23 | 2.27 | 0.504 |
| FH-OP | 9.06 | 2.96 | 10.05 | 1.73 | 0.196 | 8.67 | 2.18 | 8.50 | 2.44 | 0.812 | −0.40 | 3.10 | −1.55 | 2.01 | 0.160 |
| FH-ML | 26.83 | 4.74 | 27.50 | 4.12 | 0.625 | 26.92 | 5.18 | 27.10 | 4.71 | 0.904 | 0.08 | 2.92 | −0.40 | 1.39 | 0.501 |
| Gonial angle | 123.29 | 6.38 | 125.55 | 4.17 | 0.182 | 124.63 | 5.38 | 123.95 | 4.44 | 0.657 | 1.33 | 3.97 | −1.60 | 2.28 | 0.006 ∗ |
| Distances (mm) | |||||||||||||||
| A(x) | 62.02 | 4.21 | 60.92 | 4.49 | 0.409 | 63.32 | 3.43 | 64.22 | 4.23 | 0.444 | 1.31 | 2.46 | 3.30 | 3.42 | 0.030 ∗ |
| B(x) | 51.57 | 4.65 | 53.89 | 5.90 | 0.151 | 56.78 | 4.94 | 56.75 | 6.39 | 0.987 | 5.21 | 2.89 | 2.86 | 4.11 | 0.032 ∗ |
| Pog(x) | 51.25 | 5.25 | 53.30 | 7.03 | 0.275 | 56.85 | 6.04 | 57.10 | 8.03 | 0.907 | 5.60 | 3.59 | 3.80 | 4.25 | 0.136 |
| H(x) | 12.33 | 6.44 | 13.53 | 7.55 | 0.572 | 8.36 | 6.11 | 9.71 | 7.91 | 0.526 | −3.97 | 6.34 | −3.82 | 5.66 | 0.936 |
| A(y) | 46.00 | 2.70 | 47.96 | 3.27 | 0.034 ∗ | 49.76 | 3.24 | 50.59 | 3.14 | 0.396 | 3.76 | 2.58 | 2.63 | 2.50 | 0.147 |
| B(y) | 78.62 | 4.00 | 81.53 | 5.01 | 0.038 ∗ | 85.13 | 5.48 | 85.91 | 5.16 | 0.632 | 6.51 | 3.94 | 4.38 | 3.08 | 0.056 |
| Pog(y) | 90.96 | 4.54 | 93.69 | 6.20 | 0.101 | 98.71 | 5.43 | 99.25 | 6.65 | 0.766 | 7.74 | 3.50 | 5.57 | 2.71 | 0.028 ∗ |
| H(y) | 91.12 | 6.25 | 92.62 | 8.32 | 0.499 | 100.18 | 7.26 | 98.92 | 7.44 | 0.575 | 9.06 | 6.77 | 6.30 | 5.17 | 0.143 |
| H distance | 8.91 | 3.57 | 9.03 | 4.68 | 0.927 | 12.94 | 3.67 | 11.94 | 4.48 | 0.423 | 4.02 | 4.30 | 2.92 | 4.66 | 0.418 |
The cephalometric variables in the Herbst and control groups after treatment are compared in Table I . The SNB angle in the Herbst group was significantly smaller than that of the control group. The ANB angle in the Herbst group was significantly larger than that of the control group.
The treatment and growth changes in each group are also compared in Table I . The change of the ANB angle in the Herbst group was significantly greater than that of the control group. The SNB and gonial angles in the Herbst group increased significantly more than those of the control group. The changes in the horizontal position of Point A(x) of the Herbst group were significantly less than those of the control group. The changes in the horizontal position of Point B(x) of the Herbst group increased significantly more than those of the control group. The change in the vertical position of Pog(y) of the Herbst group also increased more than that of the control group.
Pharyngeal airway sizes in the Herbst and control groups are compared in Table II . No measurements of pharyngeal airway dimensions or volumes differed between the 2 groups before or after treatment. However, the oropharyngeal airway volume of the Herbst group was smaller than that of the control group before treatment. The treatment and growth changes in the TAv, OAv, and LAv; the depths of OA and LA; and the width of OA in the Herbst group increased significantly more than those of the control group.



