Introduction
Ameloblastomas are benign asymptomatic intraosseous lesions that affect the bones of the maxillomandibular complex, interfering both in function and facial esthetic appearance. A 14-year-4-month-old girl was referred by her clinician complaining her anterior teeth were crooked and inclined forward. The lower left mandibular tooth presented with increased pericoronal space compatible with dentigerous cyst.
Methods and Results
The aim of this report is to relate a case of unicystic ameloblastoma with conservative treatment and with indication for orthodontic treatment. The conservative therapy was performed and the lesion had been completely removed. The need for radiographic and clinical follow-up for up to 10 years, initially performed every 6 months during the first 2 years and afterwards annually, in addition to the risk of late recurrence were explained for patient and her guardian.
Conclusion
The histopathologic exam of the surgical tissue provided the final diagnosis of ameloblastoma, as the lesion had not presented in its classical form and in atypical locations, as in this case involving a tooth that had not yet erupted.
Ameloblastomas are benign asymptomatic intraosseous lesions that affect the bones of the maxillomandibular complex. They interfere with both function and facial esthetics. They originate from the epithelium involved with the formation of teeth: enamel, odontogenic rests of Malassez, reduced enamel epithelium, and odontogenic cyst lining. They are locally invasive and infiltrative growths, with frequent recurrences even after radical surgical treatment.
Ameloblastomas are the second most frequent benign odontogenic tumor. They occur in both the maxilla and the mandible, but mainly in the mandible, especially the molars, the mandibular angle, and the ramus. In the maxilla, the molar region is more commonly affected. There is no difference in distribution with regard to sex and race, but age is a factor, with adults (mean age, 37 years) affected more often and children only rarely.
Clinically, an ameloblastoma is a hard mass that can cause bone expansion. They are slow growing and progressive, and the adjacent mucosa generally has an aspect of normality without continuity of solution. They are painless, difficult for the patient to perceive in the initial stages, and, while they develop, cortical absorption occurs because of the compression produced by growth, making them palpable; in most cases, diagnosis is complemented by radiography.
Ameloblastomas have 3 clinical forms that must be recognized and differentiated, because of different treatments and prognoses, and they are divided according to the histopathologic description into solid or multicystic, unicystic, and peripheral. The solid or multicystic form is more aggressive and requires a more radical treatment than the unicystic and peripheral types, with a relatively higher rate of recurrence.
Regarding its epidemiology, multicystic ameloblastomas affect patients between the third and seventh decades of life. Clinically, it is a more aggressive variant, because its capacity to infiltrate the bone trabeculae is more evident, and, therefore, there is greater risk of recurrence of these lesions when they are not efficiently removed. The radiographic aspect is a multilocular radiolucent lesion, described as “soap bubbles” or “honeycomb.”
The unicystic ameloblastoma affects more young patients, generally in the second decade of life; its main site is the posterior region of the mandible. Radiographically, it is a multilocular radiolucent mass, which in most cases surrounds the crown of a tooth that has not yet erupted and is commonly mistaken for a dentigerous cyst. Its slow but relentless growth can cause movement of tooth roots and root resorption. The biologic behavior of this variant tends to be less invasive than multicystic ameloblastomas. They respond more favorably to conservative surgery than do solid or multicystic ameloblastomas.
The peripheral ameloblastoma accounts for only 1% of all cases and is found in the posterior alveolar and gingival mucosa. This lesion has a good prognosis if it is removed at an early stage when it is easily detected clinically, and, because the cortical bone is still preserved, it is a barrier to bone invasion by the peripheral ameloblastoma.
Treatments can be varied, depending on the histologic type and the location site, as resection (marginal or segmental), enucleation, curettage, marsupialization, cryotherapy, or a combination of these techniques. In spite of these treatment modalities identified in the literature, there is still controversy about the therapy, either its clinical presentation or its histopathologic characteristics. Furthermore, radiotherapy either with or without chemotherapy can also be recommended in specific situations: patients who have already been treated surgically more than once, patients with inoperable lesions, or elderly patients who could not withstand conventional surgery.
For this report of a patient with unicystic ameloblastoma, we used a conservative treatment. We also give the indications for orthodontic treatment.
Diagnosis and etiology
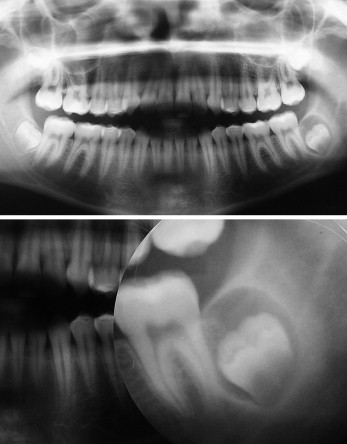
A girl, age 14 years 4 months, was referred for orthodontic evaluation because her anterior teeth were crooked and inclined forward. She had a skeletal and dental Class I malocclusion, with a 4-mm overt and anterior open bite. Radiographically, the germ of the mandibular left third molar showed an increased pericoronal space compatible with a dentigerous cyst ( Fig 1 ). The maxillary incisors were protruded, and the mandibular incisors were well positioned. She had a vertical growth trend and mild gingival recession of the maxillary left lateral incisor. She had an atypical deglutition pattern and a habit of onychophagia.
The patient was referred to an oral surgeon for assessment of the mandibular left third molar and the status of the other third molars. Orthodontic treatment was suggested with a complete fixed appliance, without premolar extraction to allow alignment, leveling, and intercuspation of the maxillary and mandibular teeth. An extraoral appliance with intermaxillary elastics was recommended. Speech therapy assessment was suggested to correct the atypical deglutition habit.
Bands were cemented on the maxillary first molars for placement of an extraoral appliance with cervical pull; the patient was referred for extraction of the mandibular left third molar ( Fig 2 , A and B ). However, when microscopic examination suggested the presence of an ameloblastoma and the need for observation ( Fig 2 , C and D ), without the application of force in the postero-inferior region, orthodontic treatment was interrupted, and the first molar orthodontic bands were removed.
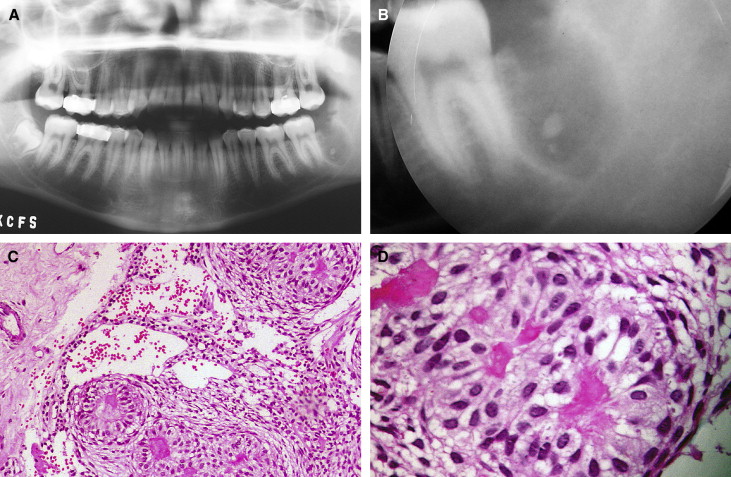
Histologic sections showed proliferations of cohesive columnar and cuboidal epithelial cells, with a clear cytoplasm and vesicular nuclei, in a mixed solid and microcystic pattern. At the periphery of the neoplastic clusters, there was palisading of nuclei. Between the blocks, the mesenchymal component was represented by a myxoid matrix and cells with spindle- or ovoid-shaped nuclei. Hyalin stromata were seen focally ( Fig 2 , C and D ).
Discussion
An ameloblastoma is an odontogenic tumor of the greatest interest in dentistry, because the literature does not agree on the best therapeutic approach. It is necessary to consider histologic type, location in the maxilla, and the possibility of monitoring the patient after therapy. Ideally, all tissue removed when an unerupted tooth is surgically exposed should be microscopically evaluated so that appropriate diagnosis and treatment can follow.
Recognition and distinction of the different forms of ameloblastomas are fundamental, because they are intimately linked to the treatment plan and prognosis. They are classified into 3 types: multicystic intraosseous or solid conventional, unicystic intraosseous, and peripheral. In the solid type, the histopathologic variants are recognized as follicular, plexiform, demoplastic, acanthomatous, basaloid, and granular cell ameloblastomas. However, the biologic behavior of the variants of ameloblastoma is the factor that dictates their capacity for recurrence, expansion, or local invasion. Irrespective of the type of ameloblastoma and its location in the maxilla or the mandible, the most indicated approach would be radical treatment to prevent recurring ameloblastomas from attaching to vital structures.
The multicystic intraosseous ameloblastoma requires a more critical approach, because of its behavior, particularly in the posterior region of the mandible and the maxilla. The association of techniques after enucleation or curettage, to be followed by cryotherapy, is interesting when the bone remainder might resist the new functional condition.
A unicystic intraosseous ameloblastoma deserves separate consideration, because of its distinct clinical, radiographic, and histopathologic characteristics. Three histopathologic variants of unicystic ameloblastoma have been described. In the first type, luminal unicystic ameloblastoma, the tumor is confined to the luminal surface of the cyst, and the lesion has a fibrous cyst wall, with a lining consisting partially or totally of ameloblastic epithelium. In the second variant, intraluminal unicystic ameloblastoma, at least 1 nodule of the ameloblastoma projects from the cystic lining into the lumen of the cyst. These nodules can be relatively small or largely fill the cystic lumen. In the third type, mural unicystic ameloblastoma, the fibrous wall of the cyst is infiltrated by a typical follicular or plexiform ameloblastoma. The extent and depth of ameloblastic proliferation can vary considerably.
According to Gardner, the diagnosis of the unicystic type is based on 2 factors: the lesion must be clinically and radiographically uniloculated, and the microscopic examination must show a single cystic lesion with a covering epithelium of ameloblastic cells. That is, for the lesion to be unicystic, it is necessary to consider all clinical, radiographic, and histopathologic results. However, there is a tendency for all lesions with a unicystic clinical and radiographic aspect to be considered unicystic ameloblastomas; this is a mistake.
The peripheral type of ameloblastoma, also called extraosseous, is defined as one that is confined to the gingiva or alveolar mucosa, and histomorphologically might exhibit any of the same patterns as the intraosseous type, having an indolent biologic behavior with extremely rare recurrences.
Postoperative follow-up is important in the management of ameloblastoma because of recurrence, which depends on factors such as choice of treatment of the primary lesion, extent of the lesion, site of origin, proliferation of residues not removed during surgery, and implantation of neoplastic tissue in other locations during surgery. Recurrence rates of 90% in the mandible and 100% in the maxilla have been reported for multicystic tumors treated only with conservative therapy such as curettage and enucleation. Recurrent lesions appear an average of 14 to 15 months after the initial treatment. They can also appear later (18 months) or as much as 4 to 10 years later.
In light of the important fundamental concepts in the current literature, it is believed that the less invasive therapeutic modalities can result in successful treatments, mainly when allied with the clinical, imaginal, and surgical considerations previously discussed. This agrees with our clinical for this patient.
Extensive resections have been used to treat solid ameloblastomas to prevent possible recurrences. However, these surgeries are invariably associated with serious problems for the patient, such as masticatory dysfunction, mutilation, facial deformity, and abnormal mandibular movements. The rate of recurrence is a crucial factor for coherent planning, but other aspects are also important and must be considered in the therapeutic approach, including emphasizing morbidity and the patient’s quality of life.
For our patient, surgical enucleation of the intraosseous mass was performed in association with a tooth with incomplete rhizogenesis. The lesion had an evident cleavage plane, which favored its entire removal. It came away from the bone tissue easily, and, because the clinical and radiographic diagnostic impression was that of a dentigerous cyst, it became evident only after histopathologic examination that it was a unicystic ameloblastoma. After the result was known, a review of the slide was requested, in which the initial report of unicystic ameloblastoma was confirmed. The patient and her guardians were informed of this diagnosis with regard to the pathology, development, prognosis, and forms of treatment.
The reasons for the conservative therapy were again explained, since the lesion had been completely removed. Radiographic and clinical follow-up are necessary for up to 10 years: every 6 months for the first 2 years and then annually. In addition, the risk of late recurrence, based on the evidence in the literature, was explained to the patient and her parents. At first, the traditional therapy of resection of the site of the lesion was not discarded, but, after histopathologic examination of the tissue and the therapeutic indication based on the evidence in the literature, the less invasive form of therapy and follow-up were chosen. Figure 3 shows the radiographs at the 18-month follow-up.




