This case report describes the treatment of a woman with severe mandibular retrusion and maxillomandibular transverse deficiency. Her malocclusion was characterized by a large overjet, a deep overbite, and a V-shaped dental arch, and she had a skeletal Class II profile. Treatement included combined maxillary and mandibular midline expansion, maxillary downward repositioning, and mandibular ramus lengthening with distraction osteogenesis with implants as orthodontic anchorage. During the postdistraction orthodontic treatment period, some skeletal relapse occurred. Implants provided absolute orthodontic anchorage to overcome the unexpected skeletal changes. Combined orthodontic treatment with implants for anchorage and distraction osteogenesis successfully expanded the maxilla and the mandible and corrected the mandibular deficiency. Two-year follow-up records show a morphologically and functionally stable result.
Distraction osteogenesis (DO) is recognized as a major option in the treatment of maxillofacial deformities with vertical, transverse, anteroposterior mandibular, or maxillary deficiencies in growing and adult patients. Since mandibular DO was first described in 1992 by McCarthy et al, applications of distraction osteogenesis have been developed for various maxillofacial deformities. Mandibular symphyseal distraction osteogenesis (MSDO), mandibular body and ramus lengthening, the rigid external distraction system, maxillary advancement with an internal distraction device, and alveolar distraction osteogenesis have all been developed by using various unique distraction devices. Combining devices has enabled the correction of complex maxillofacial deficiencies. The advantages of DO, when compared with bilateral sagittal split ramus osteotomy (SSRO), are gradual lengthening of the bones with lengthening of surrounding soft tissues such as muscles, tendons, and fibrous connective tissues; gradual advancement or transverse expansion of the mandible with minimal influence on temporomandibular joint (TMJ) conditions ; lengthened alveolar bone providing space for aligning teeth; and reduction of skeletal relapse after application. However, DO is still rapidly developing in orthodontic treatment, and scientific and clinical evidence needs to be integrated.
On the other hand, the use of implants as orthodontic anchorage is becoming a popular, stable, and safe treatment option for various malocclusions. It provides an immobile anchor for tooth movement such as distalization of molars, intrusion of whole dental arches including molars, and simultaneous distalization and intrusion of molars. In addition, in some patients, it can also be used for intermaxillary fixation after orthognathic surgery. Many types of miniscrews and miniplates have been developed for these approaches over the past 10 years and applied to various malocclusions.
In this case report, we demonstrate combined treatment of DO and absolute orthodontic anchorage using implants in an adult Class II patient with a retrognathic profile.
Diagnosis and etiology
The patient was a Japanese woman (aged 39 years 1 month) with a chief complaint of maxillary protrusion. Her medical history was normal. She had a convex facial profile, a gummy smile, and hypertonicity of the mentalis muscle during closing of the lips. She had a severe Class II malocclusion with 12.0 mm of overjet, and she was missing the maxillary right first premolar and a mandibular left first molar. The periodontal parameters were acceptable for orthodontic treatment. The probing depth of all teeth was less than 3.0 mm, and no bleeding on probing was recorded at the initial examination. Functionally, her TMJs had no symptoms; however, anterior guidance was nonexistent.
The facial photographs indicated a convex facial appearance, a protruded upper lip, overexposure of the maxillary incisors, a gummy smile, and a large interlabial gap ( Fig 1 ). The dental casts showed severe maxillary protrusion with large overjet, deep overbite, and transverse deficiency with narrow dental arches ( Fig 2 ). The molar relationship was Angle Class II on both sides, and a lateral crossbite was found in the left second premolar region. Her panoramic radiograph showed that she was missing all third molars except for the mandibular left one, in addition to a maxillary right first premolar and a mandibular left first molar as described above ( Fig 3 ).


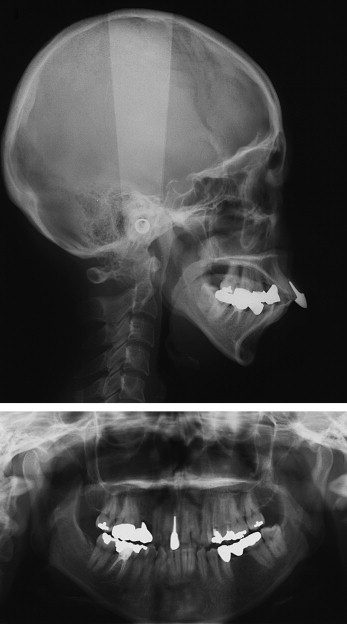
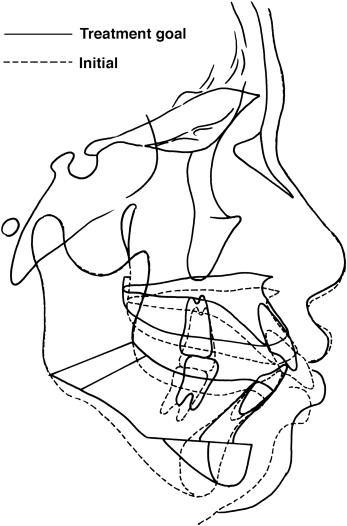
Cephalometric analysis indicated that she had a skeletal Class II jaw deformity ( Fig 4 ). The ANB angle was 8.0°, and the Wits appraisal was 6.3 mm. The SNA angle of 80.1° reflected a normally positioned maxilla, and the SNB angle of 72.1° indicated mandibular deficiency. Her mandibular plane angle to the SN plane (MP-SN) was 49.5°; this was steeper than that typical of Japanese women. In addition to these skeletal problems, she had labially proclined and extruded maxillary incisors and extruded mandibular incisors with a deep curve of Spee. The linear and angular cephalometric measurements are given in the Table. The following problems needed to be resolved: (1) skeletal Class II anteroposterior jaw relationship, (2) steep mandibular plane angle, (3) narrow maxillary and mandibular dental arch, (4) gummy smile with large interlabial gap and tooth exposure, (5) bilateral Angle Class II molar relationships, (6) large overjet, (7) excessive mandibular incisor height and deep overbite, (8) lateral crossbite at the left first premolar, and (9) labial proclination of the maxillary incisors.
Treatment objectives
Because the patient was concerned about her facial esthetics, treatment options were considered to correct the mandibular deficiency. The severe skeletal Class II deformity directed the orthognathic surgery. To solve the problems above, the treatment objectives for this patient were the following: (1) correct the imbalanced Class II anteroposterior jaw relationship; (2) coordinate the widths of the dental arches; (3) reduce the steep mandibular plane angle; (4) reduce the deep overbite; (5) improve the gummy smile, the large interlabial gap, and tooth exposure; (6) correct the molar relationship; (7) reduce the overjet; (8) decrease mandibular incisor height; (9) correct the lateral crossbite on the left side; and (10) improve the inclination of the maxillary incisors.
A 2-dimensional visualization of the treatment goals for the patient on the cephalometric tracing is shown in Figure 4 . Five millimeters of maxillary impaction, 7 mm of advancement of the mandible, 5 mm of advancement of the chin, and height reduction of the symphysis were planned.
The 7 mm of planned mandibular advancement was on the borderline between bilateral SSRO or DO. Without making the space to align and intrude the anterior teeth by MSDO and maxillary midline DO, extraction of the premolars would be needed. By using implants as orthodontic anchorage from the beginning of treatment, tooth-bearing alveolar bone generated by DO could be used as available alveolar bone. In addition, because widening of the dental arches was also needed, we decided to use a combination of MSDO, maxillary midline DO, and mandibular ramus and body DO to achieve the treatment goals in one-time surgical intervention without tooth extractions. The following treatment was planned to achieve these treatment objectives: (1) bilateral mandibular ramus and body DO to simultaneously increase the ramus height and body length, and reduce the mandibular plane angle; (2) MSDO and maxillary midline DO to coordinate the arch widths and partially obtain space to retract the maxillary incisors and intrude the mandibular incisors; (3) impaction of the maxilla to reduce the anterior maxillary incisor height; (4) genioplasty to improve the retruded chin and reduce incisor height; (5) retraction and retroclination of the maxillary incisors to reduce overjet by using implants as orthodontic anchorage; and (6) flattening the deep curve of Spee and intruding the mandibular incisors to reduce mandibular incisor height.
Treatment objectives
Because the patient was concerned about her facial esthetics, treatment options were considered to correct the mandibular deficiency. The severe skeletal Class II deformity directed the orthognathic surgery. To solve the problems above, the treatment objectives for this patient were the following: (1) correct the imbalanced Class II anteroposterior jaw relationship; (2) coordinate the widths of the dental arches; (3) reduce the steep mandibular plane angle; (4) reduce the deep overbite; (5) improve the gummy smile, the large interlabial gap, and tooth exposure; (6) correct the molar relationship; (7) reduce the overjet; (8) decrease mandibular incisor height; (9) correct the lateral crossbite on the left side; and (10) improve the inclination of the maxillary incisors.
A 2-dimensional visualization of the treatment goals for the patient on the cephalometric tracing is shown in Figure 4 . Five millimeters of maxillary impaction, 7 mm of advancement of the mandible, 5 mm of advancement of the chin, and height reduction of the symphysis were planned.
The 7 mm of planned mandibular advancement was on the borderline between bilateral SSRO or DO. Without making the space to align and intrude the anterior teeth by MSDO and maxillary midline DO, extraction of the premolars would be needed. By using implants as orthodontic anchorage from the beginning of treatment, tooth-bearing alveolar bone generated by DO could be used as available alveolar bone. In addition, because widening of the dental arches was also needed, we decided to use a combination of MSDO, maxillary midline DO, and mandibular ramus and body DO to achieve the treatment goals in one-time surgical intervention without tooth extractions. The following treatment was planned to achieve these treatment objectives: (1) bilateral mandibular ramus and body DO to simultaneously increase the ramus height and body length, and reduce the mandibular plane angle; (2) MSDO and maxillary midline DO to coordinate the arch widths and partially obtain space to retract the maxillary incisors and intrude the mandibular incisors; (3) impaction of the maxilla to reduce the anterior maxillary incisor height; (4) genioplasty to improve the retruded chin and reduce incisor height; (5) retraction and retroclination of the maxillary incisors to reduce overjet by using implants as orthodontic anchorage; and (6) flattening the deep curve of Spee and intruding the mandibular incisors to reduce mandibular incisor height.
Treatment alternatives
Because the patient’s main concern was related to facial esthetics, treatment options were considered to correct the mandibular deficiency. Her severe Class II skeletal relationship required orthognathic surgery. Bilateral SSRO and LeFort I osteotomy or a combination of mandibular ramus and body DO, MSDO, and maxillary midline DO were considered as treatment options. DO can provide bone regeneration to increase the available arch length for tooth alignment at the beginning of combined orthodontic and orthognathic surgical treatment, whereas bilateral SSRO cannot provide this effect. In addition, since midline DO can enlarge the oral cavity, we selected DO as the primary option in her treatment.
Treatment progress
Fixed prostheses for the maxillary right first premolar and mandibular left first molar were removed. Fixed appliances (0.022 × 0.028-in preadjusted edgewise) were placed, and segmented passive wires (0.019 × 0.026-in heat-treated heavy wires) were set in each quadrant of both dental arches. In the treatment plan, all DO procedures were to be performed before orthodontic tooth movement because the space created by bone regeneration was needed to align and level the dental arch. Bilateral osteotomy at the angle of the mandible, mandibular symphyseal osteotomy with genioplasty, and maxillary midline osteotomy with LeFort I osteotomy were performed with an intraoral approach. The anterior part of the maxilla was impacted and wired to the piriform edge. Intraoral distraction devices were placed, spanning the osteotomized sites at the mandibular angles and symphysis ( Fig 5 ). Bone-borne intraoral devices (Leibinger, Freiburg, Germany) were placed at the mandibular angle, and a bone- and tooth-borne distraction device (Leibinger) was fixed to the symphyseal osteotomy site. Both arches were fixed on the right and left with a resin-made occlusal splint. This distracted the maxillary midline as the mandibular distraction device was activated. Similarly, intermaxillary fixation transferred the distraction force from the distractor placed on the angle of the mandible to the maxillary bones, thereby inducing downward movement of the posterior maxilla. Wiring beside the anterior nasal spine was fixed to maintain the level of the anterior maxilla during distraction.


Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


