Introduction
In this study, we examined the influence of field of view (FOV) and voxel size on the diagnostic efficacy of cone-beam computed tomography (CBCT) scans to detect erosions in the temporomandibular joint (TMJ).
Methods
The sample consisted of 16 TMJs containing natural or artificially created erosions and 16 normal TMJs. CBCT scans were obtained with 3 imaging protocols differing in the FOV and the size of the reconstructed voxels. Two oral and maxillofacial radiologists scored the scans for the presence or absence of erosions. Diagnostic efficacies of the 3 imaging protocols were compared by using receiver operating curve analysis. For each TMJ imaging protocol, we used thermoluminescent dosimetry chips to measure the absorbed dose at specific organ and tissue sites. Effective doses for each examination were calculated.
Results
Areas under the receiver operating characteristic curves were 0.77 ± 0.05 for the 6-in FOV, 0.70 ± 0.08 for the 9-in FOV, and 0.66 ± 0.05 for the 12-in FOV. The diagnostic efficacy of the 6-in FOV, determined by the area under the curve, was significantly higher than that of the 12-in FOV ( P ≤0.05). Effective doses for bilateral TMJ evaluation were 558 μSv for the 6-in FOV, 548 μSv for the 9-in FOV, and 916 μSv for the 12-in FOV.
Conclusions
The diagnostic efficacy of CBCT scans for the evaluation of erosive changes in the TMJ is highest for the 6-in FOV and lowest for the 12-in FOV.
Radiographic examination is an essential component of the diagnostic evaluation of temporomandibular joint (TMJ) disease. It is well established that clinical examination alone is not reliable for diagnosis of TMJ disorders (TMD). Radiographic examination is used to detect osseous abnormalities, assess their severity, and evaluate the condyle-fossa relationship. Osseous abnormalities associated with degenerative arthritis of the TMJ include loss of articular cortication, erosions, sclerosis, flattening of the articular surfaces, and osteophyte formation. Additionally, other bony abnormalities caused by neoplastic and developmental disorders or infections can also manifest in the TMJ. Currently, the modalities used to evaluate TMJ bony changes include panoramic radiography, conventional (linear or complex motion) tomography and computed tomography (CT) with helical or multi-slice CT or cone-beam CT (CBCT). Additionally, some panoramic units allow acquisition of TMJ-specific views. The diagnostic efficacies of these various techniques are different. For example, panoramic radiography has poor reliability and low sensitivity for detection of TMJ osseous changes compared with CT. A systematic review examined the performance of various imaging techniques used for detection of TMJ erosions and osteophytes, and the authors proposed axially corrected sagittal tomography as the modality of choice for this purpose. Over the past few years, CBCT has been used widely to evaluate the maxillofacial skeleton for a variety of diagnostic tasks, including TMJ evaluation. CBCT provides several advantages over panoramic radiography and conventional tomography: it allows visualization of the bony components in all 3 planes of space and provides excellent visualization of osseous changes in the TMJ. Furthermore, the image volume can be reconstructed along the long axis of the condylar head to enable reliable assessment of the condyle-fossa relationship. In direct comparative analyses for the detection of condylar cortical erosions, CBCT provides superior reliability and greater accuracy than corrected tomography and TMJ panoramic projections. Current guidelines developed by the Research Diagnostic Criteria for Temporomandibular Disorders also recommend CT as the modality of choice for evaluation of TMJ osseous changes, for both research and clinical settings. From the point of view of radiation dose, CBCT is preferable to helical or multi-slice CT. Because of its superior diagnostic efficacy and growing availability, CBCT is likely to become the modality of choice for evaluation of TMJ osseous components.
Frequently, TMJ evaluation is part of a comprehensive radiologic analysis of the craniofacial structures. For example, an important component of assessment of facial asymmetry is the evaluation of TMJ morphology. Furthermore, TMJ status is also an important factor during craniofacial skeletal assessment for orthodontic treatment planning and progress, where manipulation of the occlusal relationships could alter the loading and usage of the joint. In general, for these diagnostic tasks, patients are imaged by using a full field of view (FOV) CBCT unit. Full FOV units such as the CB MercuRay (Hitachi Medical, Twinsburgh, Ohio), NewTom (AFP Imaging, Elmsford, NY), i-Cat (Imaging Sciences International, Hatsfield, Pa), and Kodak 9500 (Carestream Dental, Atlanta, Ga) allow collimation of the FOV. For example, the CB MercuRay and the NewTom units have 3 acquisition FOVs: diameters of 6, 9, and 12 in. In these units, images obtained with smaller FOVs have smaller a voxel size and, thus, a higher image resolution. Typically, for craniofacial assessment, patients are imaged with a 12-in FOV, yielding a voxel size of 0.4 mm. In our collective clinical experience with 2 units (CB MercuRay and NewTom), we have found that osseous changes in the TMJs are better depicted in smaller FOV examinations compared with larger FOV scans. However, our observations have not been substantiated by rigorous scientific study; thus, we lack evidence to suggest that the diagnostic efficacy of the smaller FOV scan is superior to that of the larger FOV scans. This information is particularly important when patients are imaged with a full FOV scan, which could be diagnostically inadequate for critical assessment of osseous changes in the TMJ. Here, we present the findings from an in-vitro comparison of the diagnostic efficacy of 3 FOVs for evaluation of osseous erosions in the TMJ.
Material and methods
Sixteen dentate or partially dentate dry human skulls were used for this study. Osseous defects on the mandibular condylar heads were documented. Of the 32 TMJs, 3 had naturally occurring erosions. To simulate early erosive changes, we created a defect on the condylar head, approximately 1 to 1.5 mm in depth, using a dental hand piece and a round bur ( Fig 1 ). These defects were created on the lateral, central, and medial poles of the condyle or in a combination of the 3 sites. These defects were created on 16 randomly selected condylar heads, yielding an incidence rate of 50%.
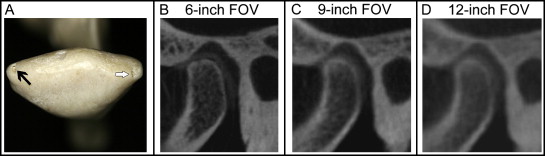
Metallic springs and screws on the skulls were removed. A small piece of latex was placed on the condylar head to separate the condyle and the glenoid fossa. The maxillary and mandibular teeth were positioned into occlusion and held in place with a rubber band. Two water-filled latex balloons were placed in the cranial vault of each skull to simulate intracranial soft-tissue absorption. Two acrylic plastic plates with a combined thickness of a half inch were placed between the x-ray source and the skull to simulate soft-tissue absorption. The skulls were imaged on a Hitachi CB MercuRay CBCT scanner with exposure parameters of 120 kV and 150 mAs. Each skull was imaged with 12-, 9-, and two 6-in FOVs ( Fig 1 ). The voxel sizes for these FOVs were 0.4, 0.3, and 0.2 mm, respectively. For the 9- and 12-in scans, the skulls were positioned to encompass the craniofacial skeleton. For the 6-in scans, each TMJ was imaged individually with the TMJ in the center of the image field. The images were acquired and reconstructed by using the Dental CT software (Hitachi Medical).
Two board-certified oral and maxillofacial radiologists (A.G. and S.M.) independently analyzed the CBCT examinations. The radiologists were blinded to the results of the gross morphologic evaluations and to the status of the artificially induced lesions. To simulate actual practice, the radiologists evaluated the entire DICOM data set for each examination, using CB Works software (Hitachi Medical). The examiners were allowed to manipulate image brightness, contrast, and magnification, and use the secondary reconstruction tools in the software program.
Before image analyses, the examiners were calibrated using a set of 4 examinations from each FOV of the experimental data. They were asked to record the presence or absence of erosions on a 5-point scale: 1, definitely present; 2, probably present; 3, uncertain if present; 4, probably not present; and 5, definitely not present. The examiners scored the images from the 6-, 9- and 12-in FOVs on separate sessions, at least 2 weeks apart. The order of examinations was varied between the sessions. To ensure intraexaminer reliability, the examinations were viewed twice, with at least 6 weeks between examinations of the same FOV.
We used thermoluminescent dosimeter (TLD) chips to measure absorbed doses at selected anatomic sites of a head and neck phantom (RANDO, The Phantom Laboratory, Salem, NY) as listed in Table I . Precalibrated TLD chips (TLD 100, 3 × 3 × 1 mm) (Landauer, Glenwood, Ill) were obtained and analyzed. The time between exposure and TLD reading was less than 48 hours. Doses were measured for the 6-in FOV (left and right TMJs separately), 9-in FOV, and 12-in FOV. For each FOV, the phantom was positioned as described above and scanned consecutively 3 times to provide a sufficiently high radiation dose that could be reliably measured by the dosimeters. The measured dose for each dosimeter was divided by 3 to yield the absorbed dose per scan.
| Location of the TLD | Tissue or organ | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Bone marrow | Thyroid | Esophagus | Skin | Bone surface | Salivary glands | Brain | Lymphatic nodes | Muscle | Extrathoracic airway | Oral mucosa | |
| Estimated fraction of tissue irradiated (%) | 16.5 | 100 | 10 | 5 | 16.5 | 100 | 100 | 5 | 5 | 100 | 100 |
| Calvarium anterior | • | • | |||||||||
| Calvarium left | • | • | |||||||||
| Calvarium right | • | • | |||||||||
| Calvarium posterior | • | • | |||||||||
| Center cervical spine | • | • | • | • | • | ||||||
| Right mandibular body | • | • | • | • | • | • | |||||
| Left mandibular body | • | • | • | • | • | • | |||||
| Right ramus | • | • | • | • | • | • | |||||
| Left ramus | • | • | • | • | • | • | |||||
| Thyroid surface | • | ||||||||||
| Midline thyroid | • | • | |||||||||
| Esophageal space | • | • | • | • | |||||||
| Right lens of eye | • | ||||||||||
| Left lens of eye | • | ||||||||||
| Right cheek | • | • | |||||||||
| Left back of neck | • | ||||||||||
| Right parotid | • | • | • | • | • | ||||||
| Left parotid | • | • | • | • | • | ||||||
| Right submandibular gland | • | • | • | • | • | ||||||
| Left submandibular gland | • | • | • | • | • | ||||||
| Sublingual gland | • | • | • | • | • | ||||||
| Midbrain | • | ||||||||||
| Pituitary fossa | • | ||||||||||
| Right orbit | • | ||||||||||
| Left orbit | • | ||||||||||
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


