Introduction
Although chincups are the preferred treatment for growing children with mandibular prognathism, the mechanism by which chincups improve this condition remains unclear. The aim of this study was to use geometric morphometrics to evaluate changes in the shape of the mandible of prognathic children treated with a chincup.
Methods
Geometric morphometrics were used to evaluate the short-term mandibular shape changes in 50 prognathic children treated with chincups compared with 40 untreated matched controls. Twenty-one 2-dimensional mandibular landmarks from cephalograms taken before and after 36 months of treatment or observation were analyzed by Procrustes superimposition and thin plate spline.
Results
Permutation tests of the treated patients showed highly significant differences in the mandibular shapes before and after treatment, and compared with the control group after the observation period. The thin plate spline grid deformations indicated more rectangular mandibular configuration, forward condyle orientation, condyle neck compression, gonial area compression, and symphysis narrowing.
Conclusions
Early chincup treatment widely modifies the mandibular shape of prognathic children to improve Class III malocclusion.
Mandibular prognathism is responsible for about 20% of skeletal Class III malocclusions and originates from imbalances in mandibular size, form, and position with respect to the maxilla or the cranial base. Malocclusions are not self-correcting and actually worsen during growth and development, because of excessive forward mandibular growth. Early treatment is recommended, since the morphologic pattern of the prognathic face associated with excessive forward mandibular growth is most likely established early in life.
The chincup is the preferred orthopedic appliance for growing children with mandibular prognathism and a normal maxilla. Studies evaluating the skeletal and dental effects of chincups by conventional cephalometric analyses indicate that they improve Class III malocclusions by redirecting mandibular growth backward or downward, repositioning the mandible backward, closing the gonial angle, retarding mandibular growth, remodeling the mandible and temporomandibular joint, and retroclining the mandibular incisors. Nevertheless, the mechanisms by which this treatment improves prognathism remain unclear. One hypothesis is that the chincup directly applies orthopedic forces that modify the mandibular shape, thereby improving skeletal Class III malocclusion.
Conventional cephalometrics measure linear distances or angles but do not relate distance or angle changes to whole form changes, leading to certain limitations for shape assessment. Geometric morphometric methods, including Procrustes superimposition and thin plate spline (TPS), are being increasingly used in orthodontics to study shape changes. Only a few clinical studies have used these methods to determine changes in mandibular shape after orthopedic functional treatment with the Twin-block, Fränkel, and Teuscher appliances; after maxillary protraction combined with chincup appliances ; or after removable mandibular retractor appliances. Only 1 investigation attempted to evaluate changes in mandibular shape after chincup treatment, but it was a pilot study with only few clinical cases.
To elucidate the short-term treatment response mechanisms of the mandible after early chincup treatment, we performed a retrospective longitudinal study using geometric morphometrics to evaluate mandibular shape changes in treated and untreated prognathic children.
Material and methods
A group of 50 consecutive children (25 boys, 25 girls) with skeletal Class III malocclusions due to mandibular prognathism treated solely with chincups, with mean ages of 8.5 ± 0.5 years at the first observation (immediately before treatment) and 11.4 ± 0.6 years at the second observation (after treatment), were recruited from the Orthodontic Clinic of the School of Dentistry, University Complutense, Madrid, Spain. Because chincup device usage was indispensable, restrictive criteria were applied; the children were chosen from a sample of 110 treated patients only if they had mandibular symphysis narrowing (pretreatment symphysis-pogonion distance > posttreatment symphysis-pogonion distance) as a sure sign of cooperation. Forty untreated children (20 boys, 20 girls), with mean ages of 8.6 ± 0.4 years at the first observation and 11.7 ± 0.5 years at the second observation, matched by age, skeletal maturity, sex, and observation period, with skeletal Class III malocclusions caused by mandibular prognathism and similar pretreatment dentoskeletal morphologies, comprised the control group. The availability of a sample of children with untreated skeletal Class III malocclusion was because many parents refused chincup treatment at the first observation (after orthodontic diagnosis and treatment planning) but came for a second visit at a later age.
Parents gave written informed consent for their children to participate in the study, which was approved by the ethics committee of University Complutense.
Inclusion criteria for both groups included diagnosis of skeletal Class III malocclusion (ANB angle, <0°; Wits appraisal, <−2 mm) caused by mandibular prognathism (SNB angle, >82°) with a normal maxilla (SNA angle, 82° ± 2°), permanent first molar relationship of at least a half cusp Class III, anterior crossbite or edge-to-edge incisal relationship, accentuated mesial-step relationship of the deciduous second molars, and white race. Exclusion criteria included congenitally missing, supernumerary, or extracted teeth; craniofacial anomalies; temporomandibular joint dysfunction; and previous or current orthopedic or orthodontic treatment.
The treated children were given an occipital chincup (Dentaurum, Ispringen, Germany) by the same operator (J.A.A.) using the same treatment protocol. Force (about 300 g per chin side) applied to the chin center was oriented along a line from gnathion to sella turcica, so that the vector force was in the direction of the condyle. The patients were instructed to wear the chincup for 14 hours daily. All children started and finished treatment or observation before the pubertal growth spurt and had cervical stage 1 (CS1) at the beginning and cervical stage 3 (CS3) at the end of the study, according to the cervical vertebral maturation method.
Lateral cephalograms were obtained with the teeth in centric occlusion in all subjects before (T1) and after (T2) a mean 36 months of chincup treatment (treatment group) or observation (control group). The same x-ray device (Orthotomograph-10, Trophy OPX/105, Trophy Radiologie, Marne la Vallée, France; 90 kV, 10-15 mA), technician, focus-median (150 cm), and film median (10 cm) plane distances were used. Film magnifications were standardized to 8%. At T1, conventional cephalometrics were used to evaluate the malocclusion type and dentoskeletal morphology ( Table ).
| Cephalometric measurement | Control group n = 40 |
Treated group n = 50 |
t test | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Cranial base | |||||
| S-N (mm) | 65.1 | 1.7 | 64.5 | 1.2 | NS |
| N-S-Ba (°) | 129.5 | 2.3 | 130.3 | 2.5 | NS |
| Po-PtV (mm) | −37.3 | 2.5 | −36.6 | 1.1 | NS |
| FH/Ba-N (°) | 28.0 | 1.9 | 27.7 | 1.3 | NS |
| Maxillary skeletal | |||||
| SNA (°) | 81.0 | 0.9 | 80.8 | 0.7 | NS |
| Co-Pt A (mm) | 75.9 | 2.6 | 74.8 | 2.2 | NS |
| ANS-PNS (mm) | 48.1 | 2.4 | 47.3 | 1.8 | NS |
| Mandibular skeletal | |||||
| SNB (°) | 82.6 | 0.5 | 82.8 | 0.7 | NS |
| Co-Gn (mm) | 103.8 | 4.9 | 102.4 | 3.8 | NS |
| Symphysis-pogonion (mm) | 14.8 | 1.0 | 14.3 | 0.6 | NS |
| Facial angle (°) | 89.8 | 3.7 | 90.9 | 2.7 | NS |
| Maxillary/mandibular | |||||
| ANB (°) | −1.4 | 0.7 | −1.5 | 0.5 | NS |
| Wits (mm) | −6.5 | 2.2 | −7.5 | 2.1 | NS |
| Maxillomandibular difference (mm) | 27.9 | 3.0 | 27.6 | 3.5 | NS |
| Vertical skeletal | |||||
| N-ANS (mm) | 47.0 | 3.3 | 46.7 | 2.4 | NS |
| S-Go (mm) | 62.9 | 4.1 | 63.9 | 3.3 | NS |
| N-Me (mm) | 104.6 | 7.0 | 104.9 | 5.8 | NS |
| (S-Go/N-Me) × 100 (%) | 60.4 | 3.9 | 60.9 | 3.2 | NS |
| FH to palatal plane (°) | 1.0 | 1.2 | −0.4 | 1.9 | NS |
| Ar-Go-Me (°) | 130.9 | 6.1 | 132.7 | 5.1 | NS |
| Dental | |||||
| Molar relationship (mm) | −4.3 | 1.7 | −4.5 | 2.1 | NS |
| Overjet (mm) | −1.3 | 0.8 | −1.8 | 0.8 | NS |
| Overbite (mm) | 1.0 | 1.3 | 0.9 | 1.5 | NS |
| Interincisal angle (°) | 140.4 | 7.1 | 145.2 | 8.8 | NS |
| U1 to S-N (°) | 97.9 | 7.6 | 97.4 | 6.8 | NS |
| L1 to mandibular plane (°) | 86.9 | 6.8 | 84.3 | 7.5 | NS |
To asses errors in cephalometric tracing and digitizing, 25 randomly selected lateral cephalograms were retraced and redigitized after an interval of 10 days. Errors according to Dahlberg’s formula varied between 0.15 and 0.56 mm, and 0.21° and 0.54°.
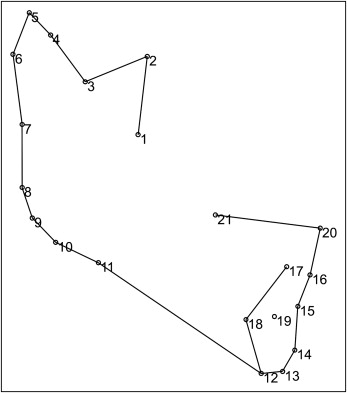
Cephalograms were imported into tpsDIG software (tpsSeries, J. F. Rohlf, Department of Ecology and Evolution, State University of New York at Stony Brook; free download at: http://life.bio.sunysb.edu/morph/ ) to digitize 21 landmarks (2-dimensional) representing mandibular morphology ( Fig 1 ). All measurements and landmark localizations were performed by a blinded examiner (J.A.A.). Measurement errors were evaluated by multivariate analysis of variance (MANOVA) by using repeated data recordings of 10 randomly selected subjects on 4 different days. No significant differences were found between the repeated samples (Wilks lambda = 0.00; F = 1.69; df 1,2 = 138, 6, 47; P = 0.2), indicating that the measurement errors were smaller than the sample variations.

Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


