Complications with orthognathic surgery can, and do, happen to virtually all practitioners involved in the treatment of patients with dentofacial deformities. A thorough understanding and appreciation of the nature of the deformity, the biologic basis for the planned procedure, the probability of specific operative and postoperative problems, and how to avoid and manage them constitutes the core of knowledge required to treat these patients successfully. In this chapter complications with orthognathic surgery are divided into two sections: Part I presents complications pertaining to mandibular procedures and Part II discusses complications with maxillary and double-jaw surgeries. In both sections complications are discussed relative to the type of surgery performed and the point at which the complication can be identified. Complications can occur with even the simplest of surgical procedures and during all phases of treatment. Appreciation of these problems provides the surgeon with the tools to maximize the surgical predictability and avoid potentially untoward results.
PART I: PREVENTION OF COMPLICATIONS WITH ORTHOGNATHIC SURGERY
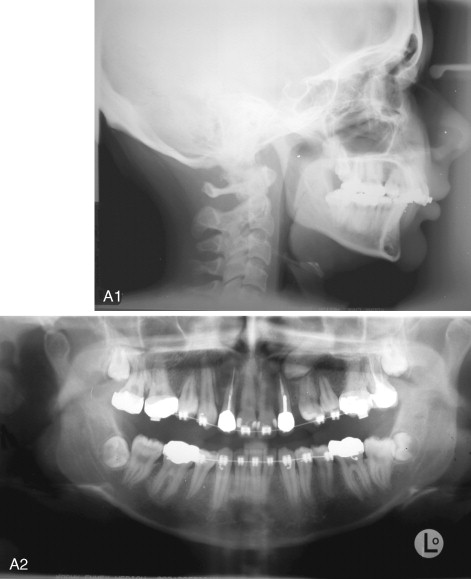
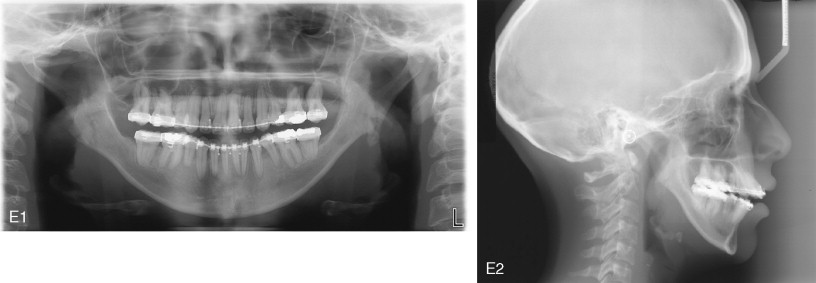
The majority of patients undergoing orthognathic surgery are American Society of Anesthesiology (ASA) status I or II and generally in good health. However, several factors are important in determining the anesthetic risks and potential complications of this surgery. In addition to overall health, evaluation of the airway is essential in these patients. Patients with maxillary and mandibular deformities, especially mandibular hypoplasia, can be difficult to intubate. Failure to manage the airway is the most significant cause of morbidity and mortality, and this is especially significant in patients with potentially difficult airways. Several bedside methods of airway assessment include maximal mouth opening, Mallampati classification, ratio of the patient’s height to thyromental distance (RHTMD), and body mass index (BMI). Mallampati class 3 or 4 and RHTMD of greater than 23.5 are both predictive of difficulty with laryngoscopy and intubation. Planning for a fiberoptic nasal intubation often is prudent in such cases.
BMI has been increasing at a rapid rate in the general population. Today more patients undergoing elective surgery are obese. This is especially relevant in the subgroup of patients undergoing orthognathic surgery for correction of obstructive sleep apnea. In addition to a difficult airway, perioperative complications in the obese patient include infection, deep vein thrombosis, cardiac events, urologic issues, positioning-related palsies, and delayed extubation. Adequate patient padding and application of pneumatic compression stockings should be routine, especially in the obese patient.
Factors that impair healing include diabetes mellitus and smoking status. Alpha et al found a 66% prevalence of postoperative infections in diabetic patients undergoing maxillary and/or mandibular osteotomies, despite adequately controlled glucose levels. Hyperglycemia is associated with impaired immune function and poor wound healing. Fasting blood glucose levels and glycosylated hemoglobin values should be normalized before surgery. Smoking impairs the healing process and increases morbidity associated with most surgical procedures. With regard to musculoskeletal surgery, smoking has been recently shown to delay the chondrogenic phase of fracture healing. Preoperative smoking cessation at least 3 weeks before surgery can reduce the incidence of impaired wound healing.
Psychological assessment before surgery should be done. Although this does not necessarily mean that all patients must undergo a psychological evaluation, surgeon awareness of psychological issues influencing patient motivation for orthognathic surgery and postoperative satisfaction are important. The majority of patients are motivated by functional and esthetic concerns. Family or close friends who are supportive of the surgery, realistic expectations, and a comprehensive understanding of the surgical course, including the risks and benefits, are important factors in ensuring patient satisfaction with the surgery.
MANDIBULAR SURGERY
PREOPERATIVE PHASE
The preoperative phase consists of diagnosis and treatment planning as well as any necessary presurgical orthodontics. Regardless of the type of mandibular surgery, certain basic preoperative orthodontic principles must be applied to reduce the chances for relapse and unacceptable results.
1.
Eliminate Dental Compensations
Dental compensations, to varying degrees, are present in the majority of patients undergoing orthognathic surgery. Decisions regarding dental extractions required to eliminate these compensations should be made at the beginning of treatment. Failure to remove dental compensations can contribute to compromised functional and esthetic results.
The primary goals of presurgical orthodontics are to place the teeth over basal bone, maximize the surgical correction, and ensure dental stability. Surgical relapse, in varying degrees, may occur after mandibular surgery. Removal of dental compensations orthodontically can help counterbalance orthodontic and surgical relapse. Incisor position is heavily influenced by the decision to extract teeth. Liberal extraction practices were largely halted with the teachings of Angle early in the twentieth century. This trend was somewhat reversed mid-century, with studies indicating improved orthodontic results when certain cases were combined with extraction therapy. The pendulum has swung back to nonextraction orthodontic treatment in recent decades, and this trend has occurred in surgical patients as well. Serial surveys of orthodontic diagnosis and treatment have indicated that the percentage of cases treated with extraction therapy has decreased from 34.9% in 1986 to 20% in 2002.
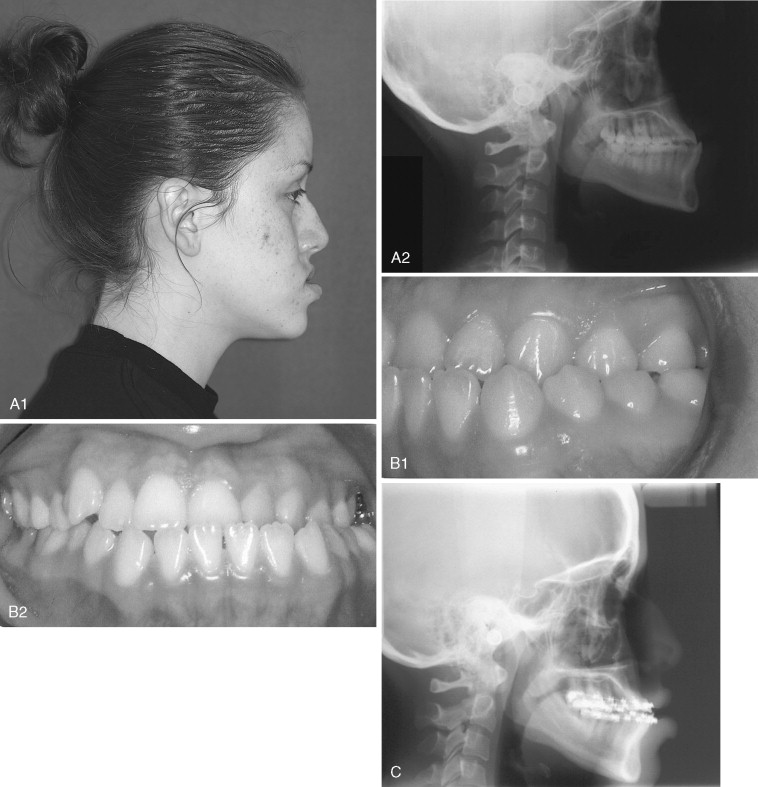
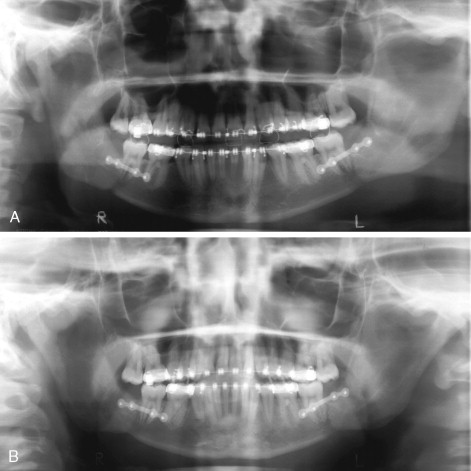
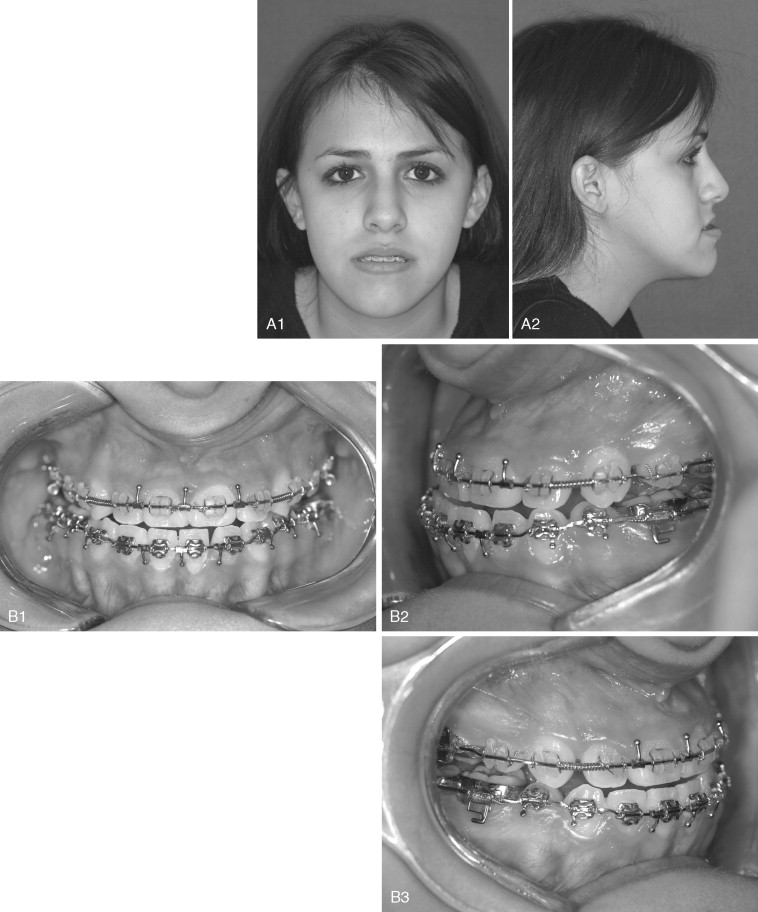
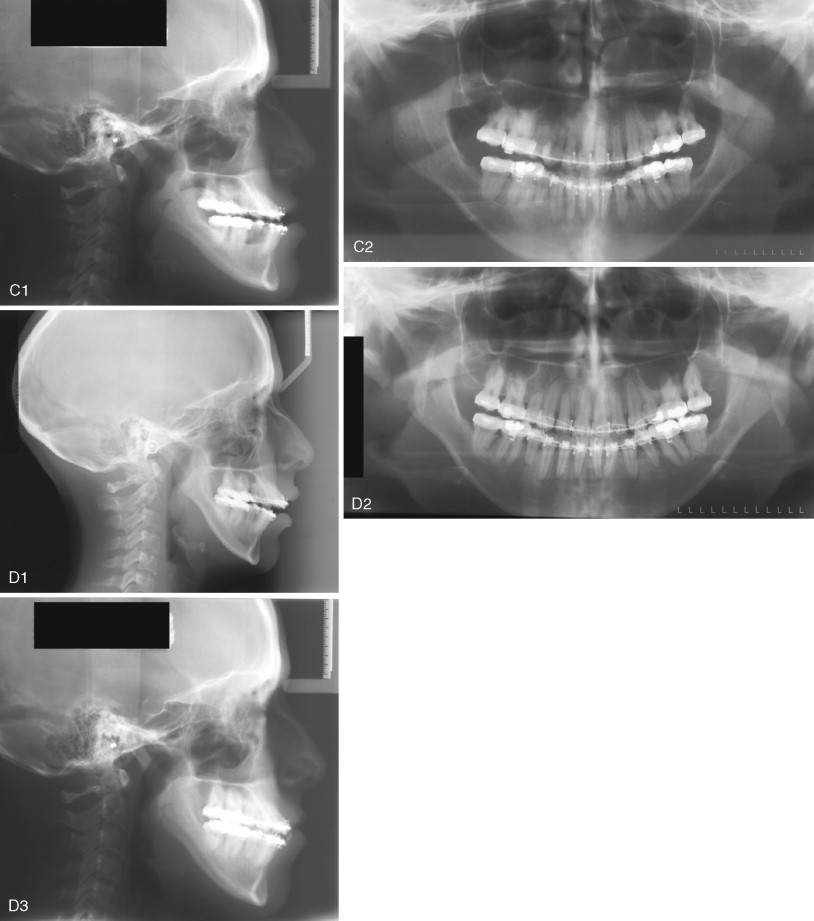
In the patient with mandibular deficiency and a class II division 1 malocclusion, dental compensations often include flared lower incisors. Proper position of the lower incisors (90 to 93 degrees to the mandibular plane) is the presurgical orthodontic goal. Preoperative orthodontics should be directed toward uprighting the lower incisors and accentuating the class II malocclusion before mandibular advancement. This can be achieved with appropriate extractions, if necessary, and class III elastics. Failure to remove these compensations before surgery reduces the magnitude of mandibular advancement and compromises the esthetic result if an advancement genioplasty is also needed ( Figure 20-1 ). The greater the proclination of the mandibular incisors, the smaller the magnitude of mandibular advancement that can be surgically achieved. Additionally, lower incisor flaring increases the Holdaway ratio to greater than 1 : 1 and an advancement genioplasty, although necessary for proper esthetics, cannot be achieved without making the labiomental fold excessively deep ( Figure 20-2 ).
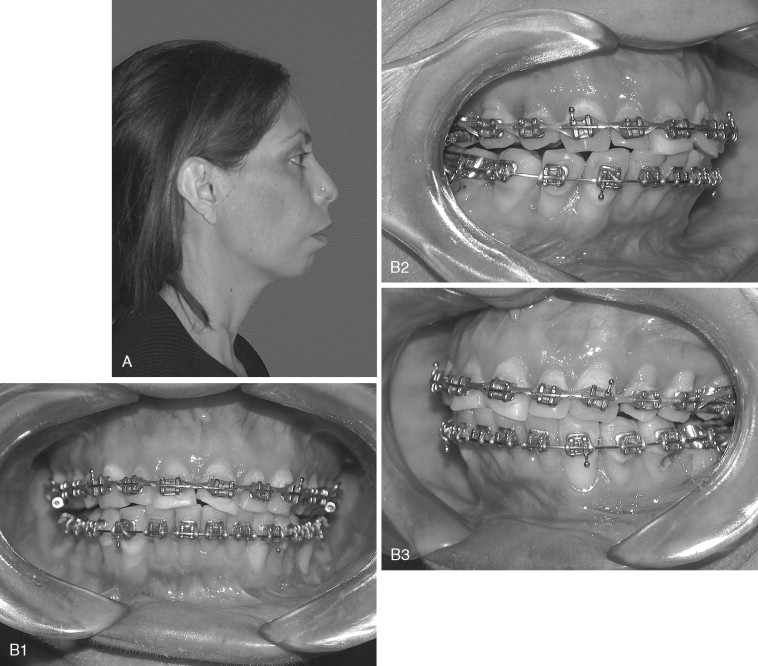

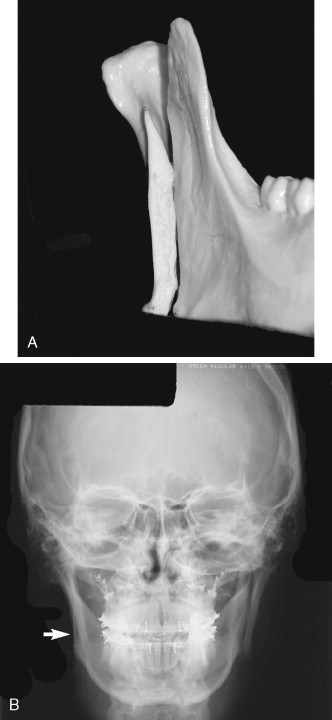
In the patient with mandibular prognathism who is planned for mandibular setback, dental compensations are removed by the opposite presurgical orthodontic mechanics. Dental compensations in the class III patient commonly include flaring of the maxillary incisors and retrusion of the mandibular incisors. Extractions may be necessary in the maxillary arch to position the maxillary incisors properly (120 degrees to the Frankfort plane or 102 to 104 degrees to Sella-nasion). Proper position of the dentition also may include preoperative class II elastics. Failure to remove compensations in the class III patient can reduce the amount of mandibular setback and maxillary advancement that can be surgically achieved ( Figure 20-3 ).
In patients with an accentuated curve of Spee and an accompanying class II division 1 deep bite malocclusion, leveling of the occlusal plane is best done after mandibular advancement. The mandibular incisors should be left in the preorthodontic position, and attempts to level the occlusal plane before surgery should be avoided. In such patients increased lower facial length is needed and esthetic results will be superior if the leveling is accomplished after surgery. The surgical-orthodontic setup is placed in a “tripod” position with contact of the terminal molars and incisors. Postoperative leveling in these cases usually proceeds relatively quickly.
2.
Failure to Manage Transverse Discrepancies Properly
Management of transverse discrepancies in children and adolescents by conventional orthodontic therapy often is successful. In adult patients (older than 16 to 18 years) with transverse maxillary deficiency, orthopedic expansion primarily consists of alveolar or dental tipping with little or no basal skeletal movement. Orthodontic treatment of skeletal transverse maxillary deficiencies should be reserved for discrepancies of less than approximately 5 mm. In these cases buccal orthodontic movement of the maxillary molars and lingual tipping of the mandibular molars can lead to a stable and predictable result. However, periodontal status and thickness of the alveolar buccal bone at the molar level may limit such maneuvers. Orthodontic or orthopedic maxillary expansion greater than 5 mm in adults may be unstable and could potentially lead to gingival recession, buccal bone resorption, root fenestration, and/or resorption.
Relapse of the expansion can lead to an anterior open bite because the effective length of the maxillary molars is increased, resulting in clockwise (posterior) autorotation of the mandible. Handelman et al noted this in several cases they analyzed after surgical mandibular advancement. They found what clinically appeared to be horizontal mandibular relapse, but it was in fact from orthodontic relapse of transverse maxillary expansion resulting in clockwise rotation of the mandible.
3.
Identify and Manage Tooth Size Discrepancies
A tooth size discrepancy, as determined by Bolton’s analysis, is common in surgical patients. In the class II patient with mandibular deficiency, failure to manage tooth size discrepancies may prevent the surgeon from achieving a class I cuspid occlusion and proper anterior coupling with adequate overjet and overbite ( Figure 20-4 ). Tooth size discrepancies are best determined from models. When a tooth size discrepancy is identified a decision should be made regarding the method and timing of treatment. The authors recommend treating tooth size discrepancies before surgery because this allows the surgeon to achieve a better fit of the anterior occlusion, especially in the cuspid regions. This can be preoperatively corrected in a number of ways, including stripping the mandibular incisors, creating spaces distal to the maxillary lateral incisors, or removing a mandibular incisor, depending on the magnitude of the discrepancy. In the patient undergoing mandibular advancement, spaces distal to the maxillary lateral incisors will allow a greater degree of mandibular advancement and assist the orthodontist in finishing the case if relapse occurs.
4.
Ensure Proper Leveling and Root Divergence in Segmental Cases
Preoperative orthodontics in cases of segmental mandibular surgery may include leveling of the individual segments. Proper leveling of the teeth adjacent to the osteotomy should been achieved, especially on the segment to be mobilized. For example, if a deep bite deformity exists and surgical intrusion of the anterior mandibular segment is planned, a rainbow curve of Spee must be leveled such that when the segment is moved inferiorly the cuspids are not buried below the level of the occlusal plane. This situation will lead to both orthodontic and periodontal problems. With segmental surgery, adequate space between the proposed tooth roots must exist. Inadequate interdental space increases the likelihood of damage to adjacent tooth roots.
5.
Prepare the Patient Psychologically for Surgery
Patients can be dissatisfied with the outcome of treatment despite a surgical success when a discrepancy exists between the expected and actual impact of treatment on the patient’s life. Flanary et al found that effective, continuous communication among the patient, surgeon, and orthodontist was among the most important factors in patient satisfaction with the surgical results. Nagamine et al found 22% of their 65 patients who had surgical correction of mandibular prognathism were dissatisfied with their results. Among the primary reasons for dissatisfaction were forward relapse of the mandible and paresthesia of the lower lip.
With the advent of video imaging, patients have been able to visualize treatment results more clearly. Some studies have indicated that video image predictors were clinically acceptable in cases of isolated mandibular surgery. However, with bimaxillary surgery video imaging may not be as accurate as initially hoped.
INTRAOPERATIVE PHASE
Intraoperative complications are often attributable to improper surgical technique and/or failure to appreciate the patient’s anatomy; however, unanticipated intraoperative complications also can occur. Intraoperative complications are discussed below for the following mandibular procedures and, when applicable, are divided into the following categories: (1) unfavorable osteotomy split, (2) nerve injury, (3) bleeding, (4) proximal segment malpositioning, and (5) miscellaneous technical difficulties.
1.
Sagittal Ramus Osteotomy
The sagittal ramus osteotomy is among the most frequently performed surgical procedures in the mandibular ramus. It is used both for mandibular advancement and mandibular setback. The intraoral sagittal osteotomy was first described by Schuchart and was modified and popularized by Trauner and Obwegeser. Obwegeser carried the medial osteotomy to the posterior border of the mandible and the vertical limb to the region of the antegonial notch. DalPont modified the osteotomy to extend further forward into the body of the mandible, and Hunsuck limited the extent of the medial cut to the retrolingular fovea. Epker further modified the technique by limiting the soft tissue dissection. Despite its frequent use, the sagittal ramus osteotomy is a technically difficult procedure. A number of authors have presented their experience with intraoperative complications with this procedure.
Unfavorable Osteotomy Split.
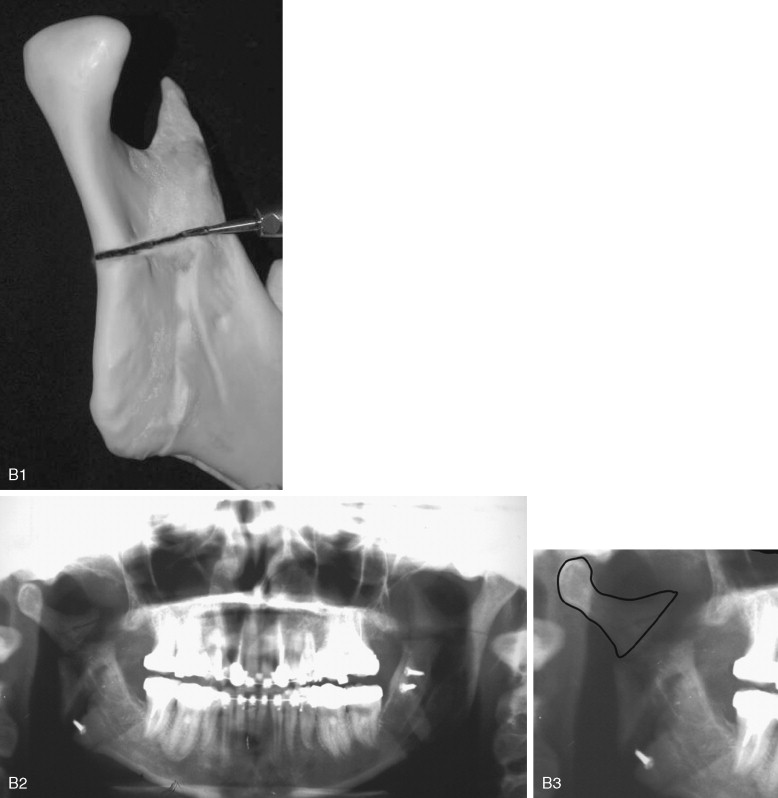
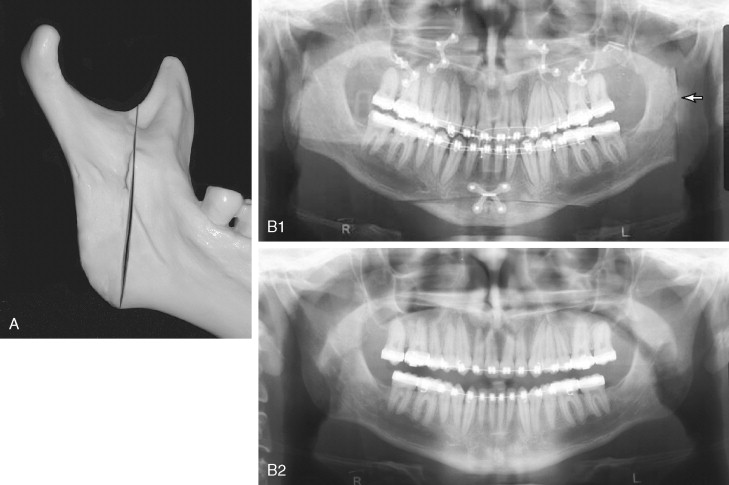
One of the most common problems associated with the sagittal split ramus osteotomy (SSRO) is unfavorable fracture of either the proximal or distal segment: incidence rates as high as 18% have been reported for these types of fractures. Once this so-called “bad split” occurs, a decision must be made regarding its treatment. One can either correct the bad split and complete the operation or abort the procedure and allow the patient to heal. It is the better part of valor to stop the operation, with a plan to reoperate after the bone has healed, if good bone contact most likely cannot be achieved ( Figure 20-5 ). This decision must be made on a case-by-case basis. Reoperating on a well-healed mandible is far easier than trying to valiantly complete the procedure and end with a nonunion from poor bone contact.
Proximal segment fracture, also known as a buccal plate fracture, is the most frequent type of unfavorable split. Several contributing factors have been cited: presence of an impacted third molar, recent removal of a third molar, age of the patient, and extent of the surgeon’s experience. In an analysis of 1256 patients who underwent sagittal osteotomy, Precious et al found that fracture of the proximal segment was more common than fracture of the distal segment (70% versus 30%). The authors did not observe any relation between proximal segment fractures and the presence of third molars, but they did note such a relation with distal segment fractures when the third molars were present.
Behrman and later Turvey reported a 3% incidence of proximal segment fracture during SSRO, and MacIntosh found a 6.6% incidence of such fractures.
Mehra et al found that fracture of the distal segment occurred more often in younger patients with impacted third molars, whereas fracture of the proximal segment was seen more often in older patients without third molars. In a group of 70 patients, Reyneke et al found three fractures of the distal segment and one fracture of the proximal segment. They observed that the presence of the third molars in young patients (younger than 20 years) was correlated with a higher rate of unfavorable fractures. The role of impacted third molars in unfavorable splits is controversial. Some believe feel that removal of third molars at least 6 months before SSRO is important in reducing the risk for adverse fractures, whereas others believe that third molars do not predispose the patient to such problems. The direction of mandibular movement, degree of impaction of the third molar, and experience of the surgeon are factors to be considered in the decision to remove third molars preoperatively. Removal of the third molars at the time of orthognathic surgery helps reduce costs and avoids an additional surgical procedure.
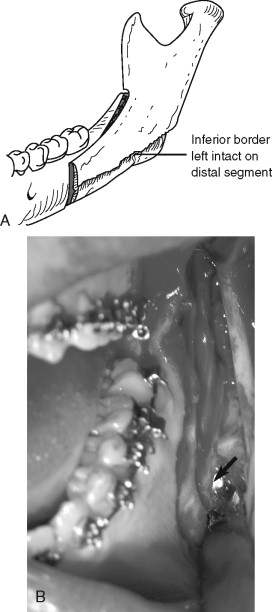
Fracture of the buccal plate most often occurs when the inferior border of the mandible is incompletely transected ( Figure 20-6, A ). In this situation, the thin buccal plate is the area of least resistance and can be fractured by the force used to split the mandible (see Figure 20-6, B ). Once a buccal plate fracture occurs, the task of completing the split is made technically difficult because the fracture leaves the buccal plate shortened and with less bone to pry against (see Figure 20-6, C ). Mehra et al did not describe their technique for completing the osteotomy after proximal segment fracture, but these authors stabilized the free proximal segment with a bone plate and monocortical screws.
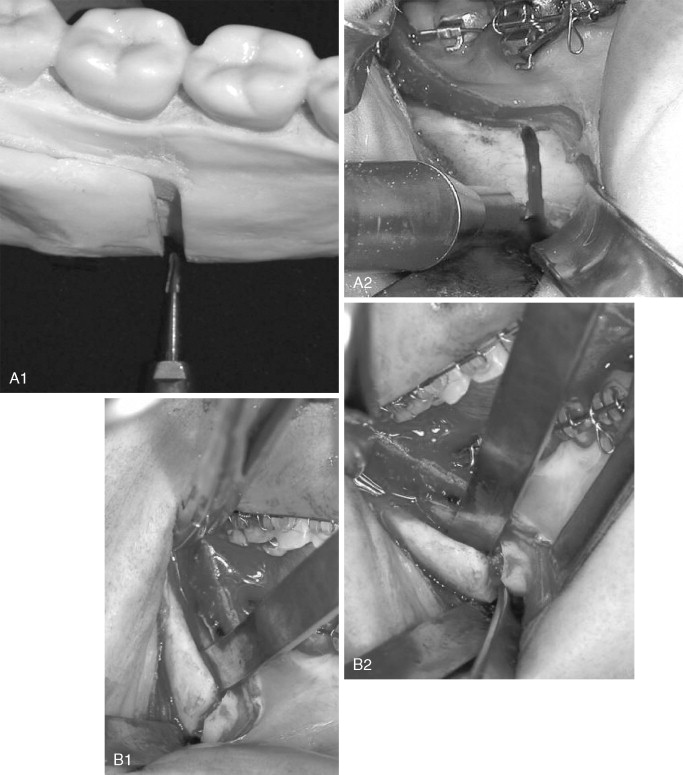
In response to a “low” fracture of the buccal plate during SSRO, the authors recommend that the buccal plate be secured with a monocortical plate immediately after it becomes fractured; the split should then be completed in the usual way (see Figure 20-6, D ). This technique is simple and quick, facilitates completion of the split, and may reduce damage to the inferior alveolar nerve that can occur when osteotomes are blindly used to finish the split.
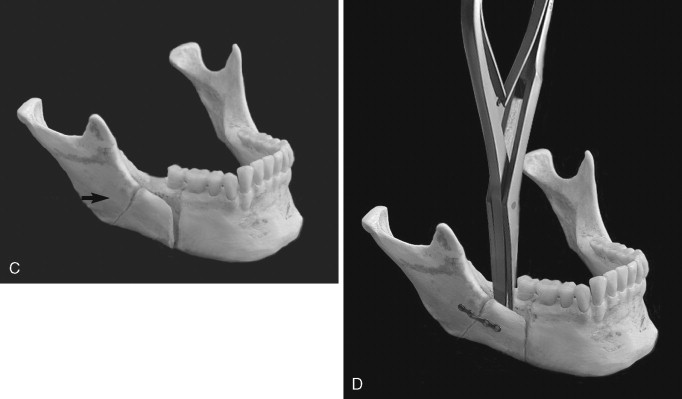
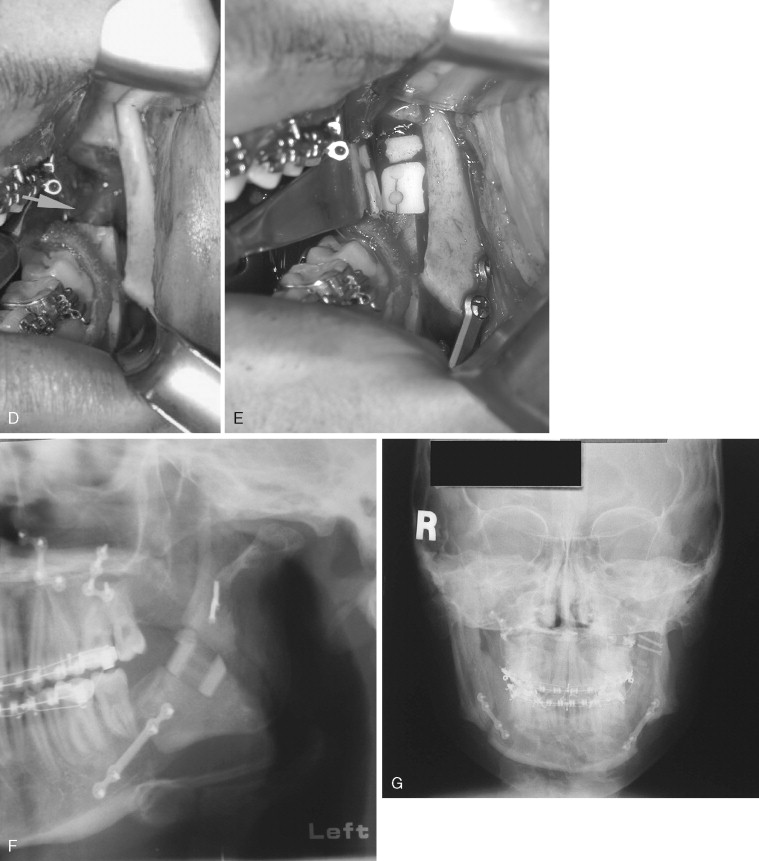
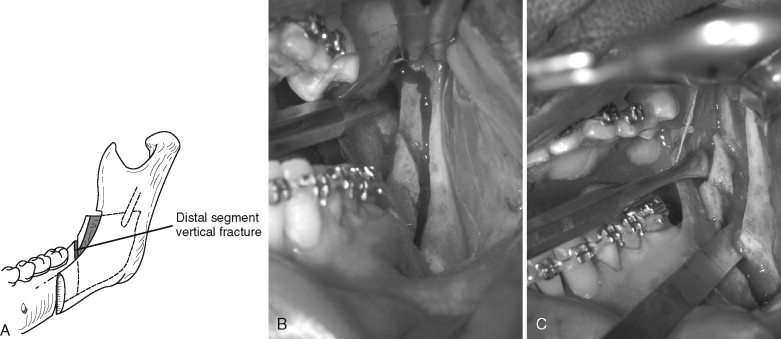
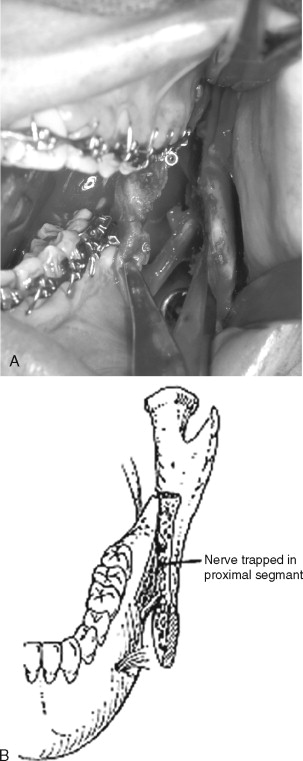
When a high buccal plate fracture occurs near the mandibular condyle, plating the segment as described above may be difficult. Patterson and Bagby discussed fracture of the proximal segment and noted that completion of the split can be extremely difficult. To complete the split, the authors recommended lateral retraction of the remaining proximal segment and vertical osteotomy of the distal segment. Although this procedure may limit the amount of advancement and may place the lingual nerve at risk from stretching or retraction of the medial tissues, the authors have found it useful in salvaging high buccal plate fractures ( Figure 20-7 ).
Fracture of the coronoid process of the mandible during SSRO has been reported and is likely caused by placement of the horizontal osteotomy too high where the ramus is thin. If an osteotome is used, it can penetrate the lateral ramus. Coronoid process fractures can be avoided by ensuring that the horizontal cut is not carried too far laterally and is made just above the lingula where the mandible is relatively thick. If the horizontal osteotomy is made in the thin part of the ramus, made too deeply, and carried to the posterior border of the mandible, a through-and-through osteotomy can occur, resulting in a free condyle–ramus segment ( Figure 20-8 ). This is among the most difficult types of unfavorable fractures to salvage. If possible, it must be corrected with an osteosynthesis plate, and the SSRO can be either be completed properly or aborted.
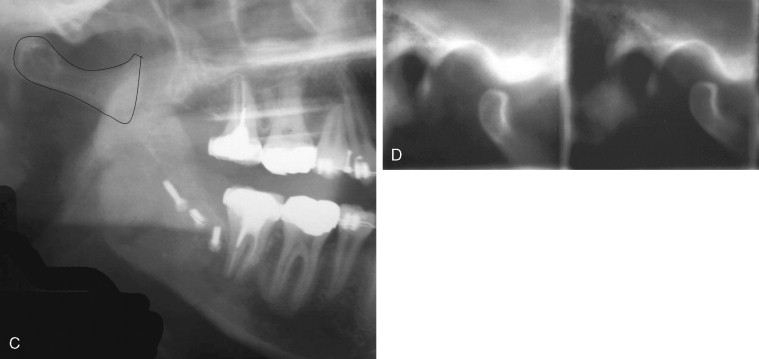
Although fracture of the buccal plate is the most common type of unfavorable fracture with the sagittal ramus osteotomy, several other types of “bad splits” also can be seen. Fracture of the distal segment during the sagittal osteotomy has been reported as an intraoperative complication. This can be encountered when the distal segment is weakened, such as when an impacted third molar is present or the patient is edentulous in the molar area, causing thinning of the mandible in this region ( Figure 20-9 ). Care must be taken if using the Smith spreader (Walter Lorenz Surgical, Jacksonville, Fla.) in applying force to the distal segment in such cases.
Occasionally, if the inferior border of the mandible is not transected completely and the osteotomy is split, the inferior border, which should be on the proximal segment, remains on the distal segment ( Figure 20-10 ).
Nerve Injury.
Injury to the inferior alveolar nerve can occur at many points during the sagittal ramus osteotomy. The nerve may be stretched or avulsed during the medial dissection; cut during the osteotomy with the burr, saw, or chisel; torn during separation of the proximal and distal segments; or injured during stabilization of the proximal segment ( Figure 20-11 ). The area of damage and incidence of nerve injury during the sagittal osteotomy are difficult to estimate from the literature. Aside from transection of the nerve, some have concluded that aggressive retraction of the medial tissues is among the prime causes of neurosensory dysfunction. Intraoperative management of a transected inferior alveolar nerve involves immediate microsurgical repair with a tension-free direct anastomosis.
White et al did not report any instances of direct damage to the inferior alveolar or lingual nerves, yet they noted 14 of the 32 surgical sites demonstrated paresthesia of the lower lip, and two patients exhibited unilateral lingual paresthesia. Behrman found that 24% of surgeons reported paresthesia of the inferior alveolar nerve in their patients but found that only two surgeons reported actually injuring the nerve. MacIntosh did not discuss the percentage of direct nerve injuries but noted that “inferior alveolar nerve transection occurred only rarely when the ramus was sectioned properly.” Turvey found nerve injury was the intraoperative complication that occurred with the greatest frequency (3.5%), and actual nerve transection occurred up to 5.5% of the time. When nerve transection occurred, it was anterior to or in the third molar region in all instances. Van Merkesteyn et al found a visible lesion of the inferior alveolar nerve in seven of the 124 sagittal ramus osteotomies in their series. Raveh et al recommended using chisels to initiate the split but not completing it until the nerve was completely visualized. They found four lacerations of 206 nerves with this technique.
The inferior alveolar nerve can be directly damaged with the burr, saw blade, or screws or excessively compressed during stabilization of the proximal segment, especially with bicortical rigid fixation. Several authors have found a greater incidence of neurosensory deficits with bicortical versus monocortical fixation.
Bleeding.
Significant bleeding is seldom encountered with the sagittal ramus osteotomy today because of greater operator experience and improved hypotensive anesthetic techniques. The incidence of major intraoperative hemorrhage has decreased from 38% in 1972 to 1% in 2005. The largest vessels in proximity are the maxillary artery and its branches (masseteric and inferior alveolar), retromandibular vein, and facial artery and vein. Behrman reported the maxillary, inferior alveolar, and facial arteries were the most common sources of hemorrhage during SSRO. Bleeding was most often encountered when dissecting or using a rotary instrument on the medial ramus during the horizontal osteotomy. In his report two patients required ligation of the external carotid artery, which did not appreciably slow the bleeding. In Turvey’s series in 1985, the incidence of troublesome hemorrhage was 1.2%. The inferior alveolar and facial arteries were the sources. Van Merkesteyn et al reported difficulty with bleeding from the inferior alveolar and facial arteries in two cases. Acebal-Bianco et al reported laceration of the facial artery in two cases of SSRO at the vertical limb of the osteotomy. The facial artery courses just beneath the inferior border of the mandible in the area of the antegonial notch. This is where the vertical aspect of the SSRO is made. Damage to the facial artery occurs from violation of the periosteum with an instrument or from the proximal segment itself after the split is completed. In most cases, control of the hemorrhage may be accomplished with packing or direct ligation of the artery.
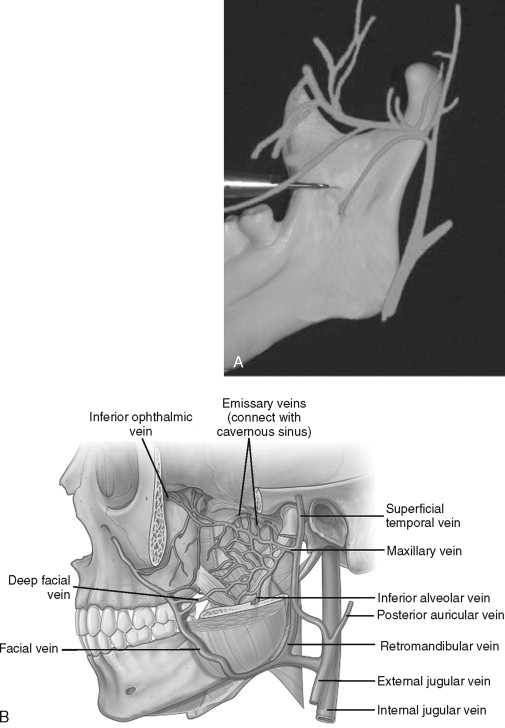
Today, fewer reports of damage to the maxillary artery exist than in the past. The maxillary artery, which courses medial to the neck of the mandibular condyle and gives rise to the masseteric and inferior alveolar arteries, is readily avoided with careful subperiosteal dissection on the medial surface of the mandible and proper placement of the horizontal osteotomy ( Figure 20-12, A ). Silva et al reported intraoperative laceration of a branch of the maxillary artery during SSRO that resulted in a pseudoaneurysm. Limiting the posterior and superior extent of the medial dissection also is advised. Teltzrow et al, in their report of 1264 patients, found the retro mandibular vein was the most common source of severe hemorrhage during SSRO (see Figure 20-12, B ).
Proximal Segment Malpositioning.
Proximal segment position after mandibular surgery has been shown to significantly influence postoperative mandibular stability, temporomandibular joint function, masticatory efficiency, and facial aesthetics. Counterclockwise rotation and condylar distraction are the most frequent positional changes of the proximal segment, although clockwise rotation of the segment also can occur. The effect of condylar position on mandibular stability is discussed in the section on postoperative complications. The incidence of proximal segment malpositioning is difficult to estimate from the literature, but reports range from 1% to as high as 75%.
Schendel and Epker found that control of the proximal segment was the most significant aspect in stability and prevention of relapse after SSRO for mandibular advancement. Proximal segment rotation was more common when wire fixation was used for stabilization. Jonhsson et al described an increase in the obtuseness of the gonial angle in 75% of the 57 patients who underwent sagittal ramus osteotomies and suggested that proximal segment rotation may be a source of this problem. Van Merkesteyn et al described proximal segment malposition in three of their 124 cases. Many techniques are used for proximal segment stabilization, each with advantages and disadvantages. The method of choice should be tailored for each patient and depends on the patient’s anatomy, direction and magnitude of mandibular movement, passive adaptation versus flaring of the proximal segment, and other technical variables as well as the patient’s medical history.
Devices have been designed to duplicate the presurgical position of the proximal segment. Gerressen et al reported no functional differences in patients who underwent mandibular advancement or setback with or without a condylar positioning device and a greater incidence of temporomandibular joint (TMJ) dysfunction in the mandibular advancement group in whom the proximal segment positioning device was used. The authors concluded that using proximal positioning devices was not worth the inconvenience.
Minor Technical Difficulties.
Minor technical difficulties include herniation of the buccal fat pad and difficulty with closure of the incision. Herniation of the buccal fat pad occurs from tearing of the periosteum on the lateral aspect of the ramus and often is the result of using a sharp anterior border stripper. This can be avoided by using an anterior border stripper with rounded tips, limiting the amount of lateral dissection, and ensuring the dissection is maintained in the subperiosteal plane.
Incision closure can be difficult if the incision is placed too high in the attached gingiva. This can be especially troublesome when an acrylic splint is used. When an erupted third molar is removed in conjunction with the sagittal osteotomy, the incision should be modified to include the extraction site.
MacIntosh has described breaking a burr while performing the horizontal limb of the sagittal osteotomy. This is a rather common occurrence and is caused by excessive torquing of the rotary instrument while the burr is engaged in the bone. When this happens the broken piece generally can be removed with a skin hook either before or after the split is completed.
2.
Vertical Subcondylar Ramus Osteotomy
Correction of mandibular prognathism using the vertical ramus osteotomy, also known as the vertical subsigmoid osteotomy, is one of the simplest osteotomies to perform and is therefore quite popular. Although the surgical approach was first described extraorally, the intraoral approach is most often performed today. The vertical ramus osteotomy of the mandible was first described by Caldwell and Letterman in 1954 as a means to set the mandible back. It was performed from an extraoral approach until 1964 when Moose described an intraoral technique performed from the lingual aspect of the mandible. In 1968 Wistanley described performing the intraoral vertical osteotomy from the lateral aspect of the mandible. With the development of improved instrumentation the vertical ramus osteotomy has become a popular procedure for mandibular setback. The primary advantages of this procedure are its surgical simplicity and speed and the lower rate of postoperative neurosensory disturbance. However, intraoperative complications with the vertical ramus osteotomy have been reported.
Unfavorable Osteotomy.
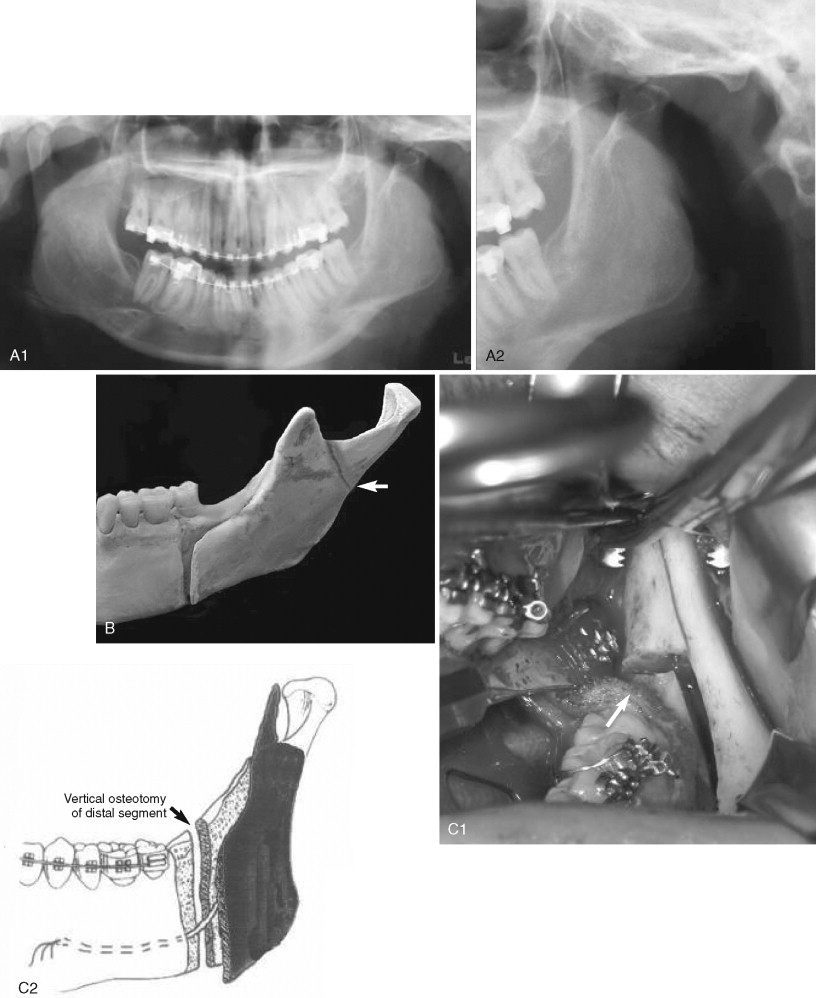
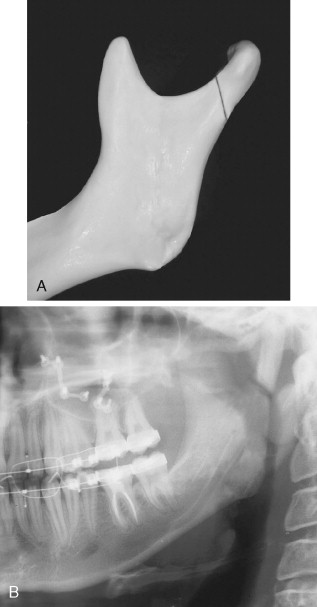
The intraoral vertical ramus osteotomy (IVRO) is commonly performed for mandibular setback and has specific instrumentation that makes the procedure technically straightforward. The intraoral blade (Stryker, Kalamazoo, Mich.) and the Bauer and Lavasseur-Merrill lighted retractors (Walter Lorenz) are helpful in executing the procedure correctly. The Bauer retractors are placed in the sigmoid notch, whereas the Lavasseur-Merrill retractor lies along the posterior border of the mandible. It has a bend in it such that when the intraoral saw blade is placed on the retractor, the osteotomy is located approximately 7 mm forward of the posterior border of the mandible. This reduces the chance of making a subcondylar osteotomy (osteotomy too close to the posterior border) or damaging the inferior alveolar nerve (osteotomy close to or through the lingula). An inadvertent subcondylar osteotomy extends from the sigmoid notch to the posterior ramus (an oblique subcondylar osteotomy), making the proximal segment into a subcondylar segment of varying size ( Figure 20-13 ). This complication is more likely in the prognathic patient with a high mandibular plane angle and an obtuse ill-defined gonial angle. Tuinzing and Greebe found this complication in one of 150 cases operated by the intraoral approach but did not discuss the postoperative sequelae. Van Merkesteyn et al noted this in one of 34 sites of vertical ramus osteotomies and likewise did not discuss the consequences.
The less-experienced operator likes to check the osteotomy position visually and often must remove the saw blade to do so. If the saw blade is not reinserted back into the osteotomy properly, a second osteotomy can be inadvertently made. If both osteotomies are completed a free segment of bone may result. This usually is not a complication, and some authors have advocated removing such a segment for large setbacks.
Nerve Injury.
The percentage of nerve injury after IVRO ranges from 0% to 14%. Fortunately, neurosensory disturbance (NSD) after IVRO is rare, presenting a marked advantage over the SSRO for mandibular setback. NSD associated with IVRO ranges from 0% to 35%, whereas NSD with SSRO ranges from 9% to 86.5% objectively and 100% subjectively.
Damage to the inferior alveolar nerve with the vertical ramus osteotomy may occur during two phases of surgery. The first is with the saw if the osteotomy is placed too close to the mandibular foramen ( Figure 20-14 ), and the second is from accidental medial displacement of the proximal segment compressing or tearing the nerve.
Hall and McKenna found a 36% rate of inferior alveolar nerve paresthesia after IVRO and surmised that actual nerve transection occurred in two of the 89 patients. As previously noted, custom retractors have been developed to assist in proper placement of the osteotomy. Radiographic identification of the position of the lingula and careful surgical technique are the best preventions for this complication. The authors’ practice is to identify the lingual on the medial aspect of the ramus before making the IVRO. Da Fontoura et al noted that the mandibular foramen is rarely less than 7 mm from the posterior border of the mandible. Some authors have recommended identifying the “antilingula,” which has been thought to represent the lateral ramus equivalent of the inferior alveolar foramen and have recommended making the osteotomy behind this landmark. However, Hogan and Ellis have concluded that the antilingula corresponds to areas of masseter muscle insertion and is not an anatomic correlate of the lingula.
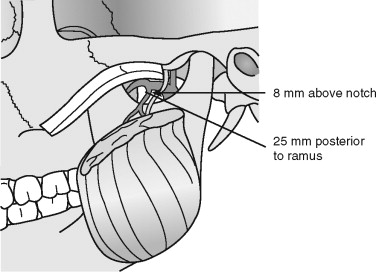
Bleeding.
Intraoperative hemorrhage has been reported with IVRO and usually is the result of transection of the inferior alveolar, masseteric, or maxillary arteries. In 1973 Astrand reported profuse bleeding in 11 of 55 patients who underwent oblique sliding osteotomies but did not discuss the source. In 1985 Tuinzing and Greebe reported three cases of damage to the maxillary artery, all of which were controlled with tamponade (packing). Quinn and Wedell reported one case in which ligation of the external carotid artery was ultimately required for control of bleeding. Ueki et al observed that bleeding with IVRO usually is minimal; however, when it happens, significant bleeding appears more likely than with the sagittal ramus osteotomy. With IVRO the superior aspect of the osteotomy is located at the sigmoid notch, which has a close relation to the masseteric and internal maxillary arteries ( Figure 20-15 ). Hwang et al estimated that the masseteric artery is approximately 26 mm from the anterior border of the ramus and 8 mm above the sigmoid notch. Care should be taken to retract and protect soft tissues during the procedure by placing a retractor within the notch. The maxillary artery lies just deep to the mandibular ramus at the level of the condylar neck and also can be damaged. If either of these arteries is torn, the osteotomy should be completed for adequate access to the torn vessel.
Proximal Segment Malpositioning.
Bell has cited difficulty with proximal segment control as the major disadvantage of the IVRO. Controversy exists regarding stabilizing the proximal segment with this procedure; however, many authors suggest no fixation or nonrigid fixation to obtain the advantage of functional positioning of the proximal segment. This functional positioning is thought to have a beneficial effect on the TMJ, especially in those patients who have preoperative TMJ dysfunction. Detachment of the masseter and a portion of the temporalis muscles are necessary to carry out the IVRO. Excessive stripping of the lateral pterygoid muscle should be avoided to prevent potential proximal segment necrosis and severe condylar sag.
After the osteotomy is completed the proximal segment must be lateralized ( Figure 20-16 ). Because of pull from the lateral pterygoid muscle, the segment may be displaced anteromedially, anteriorly toward the articular eminence, medially or inferiorly. Several problems can result if malposition of the proximal segment is not recognized. If the segment is displaced anteromedially, the inferior alveolar neurovascular bundle may be torn as it enters the lingula. If the osteotomy is incomplete or if the segment is displaced posteriorly, the mandible may not be able to be set back properly. Tuinzing and Greebe reported five cases in which the proximal segment was displaced medially during the vertical ramus osteotomy. Medial displacement resulted in a condition similar to Eagle’s syndrome in one of these five patients and necessitated surgical removal of the displaced condyle. In another of their patients the condyle was displaced posteriorly (probably because of inadequate stripping of the medial pterygoid muscle) and presented as a palpable and visual facial deformity at the angle of the mandible. Van Merkesteyn et al found proximal segment displacement in 8.8% of their vertical ramus osteotomies. They did not state in which direction the displacement occurred but noted that two patients required surgical repositioning of the condyle. Quinn and Wedell reported one case in which anterior displacement of the proximal segment ultimately required removal of the condyle with total joint replacement.
When the proximal segment is not secured in position, the remaining soft tissue attachments are relied on to maintain proper condylar position. Hall and MacKenna recommend leaving a portion of the medial pterygoid muscle attached to the proximal segment near the mandibular angle to minimize the chance for condylar sag. Walker believes that even if condylar sag is noted, normal masticatory function will seat the condyle.
Minor Technical Difficulties.
Minor technical difficulties include those already discussed with the sagittal ramus osteotomy technique as well as inability to reposition the distal segment in the planned amount. This can be problematic with large mandibular setbacks. Tuinzing and Greebe recommend removing a wedge-shaped piece of bone from the sigmoid notch in large setbacks. They note that this may be technically difficult, and damage to the maxillary artery may be encountered. Braun and Sotereanos reported one case in which a unilateral styloidectomy was necessary to complete the mandibular setback. They recommend evaluating the styloid processes in patients who are to undergo mandibular setback procedures with the vertical ramus osteotomy. Hall and McKenna modified their technique such that the osteotomy curves forward just beneath the lingula and with simultaneous coronoidotomies have found no difficulty in repositioning the mandible up to 12 mm posteriorly.
3.
Inverted L and C Osteotomies
Both the inverted L and the C osteotomies are used for correction of difficult and more unusual mandibular dysplasias. The technique of intraoral inverted L osteotomy for mandibular advancement is technically straightforward and has a low morbidity rate. This method also has been adopted in attempt to reduce the frequency of postsurgical NSDs. Some authors prefer the inverted L osteotomy (with bone grafts) for significant mandibular advancement and/or significant lengthening of posterior facial height. It also has been described for correction of open bite deformities. The intraoperative complications with these procedures are similar to those already described with the vertical ramus osteotomy. The literature is dated on this issue because of the infrequent use of these procedures.
Mandibular Body and Symphysis Surgery.
Surgical procedures in the mandibular body and symphysis consist of the subapical osteotomies (anterior, posterior, or total), mandibular body osteotomy, and mandibular symphyseal osteotomy (genioplasty).
Subapical Osteotomies.
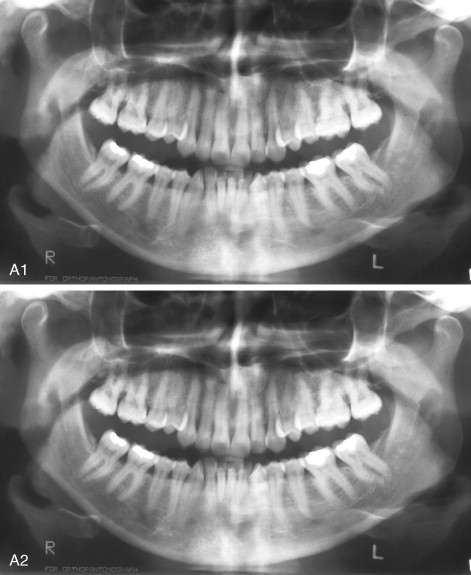
Subapical osteotomies are indicated for movement of dentoalveolar segments while maintaining an intact inferior border of the mandible. The subapical osteotomy generally refers to an osteotomy of the anterior mandible and typically is used for leveling or setting back an anterior segment. The anterior segment usually consists of the cuspids and incisors. The horizontal aspect of the osteotomy should be made at least 5 mm beneath the apices of the teeth to maintain tooth vitality. This also provides an area for stabilization of the segment. These cases often involve interdental osteotomies and thus adequate root divergence is necessary. Inadequate interdental space can contribute to root damage ( Figure 20-17 ). The thickness of the buccal cortex can be significant, and the tooth roots generally are not visible through the buccal cortex as they can be in the maxilla. Root divergence is best assessed from properly angulated periapical radiographs. Sher, in his 1984 survey of complications with subapical surgery, found that most surgeons recommend using fine osteotomes rather than saws for interdental cuts. The buccal cortex is cut with a burr or saw blade and the remainder of the osteotomy is completed with a fine osteotome. If an extraction and interdental ostectomy are planned, care must be taken at the inferior aspect of the osteotomy where adjacent tooth roots may converge toward the surgical site. Additionally, proper leveling of the anterior segment before surgery must be accomplished to avoid placing the most proximal teeth (usually the cuspids) beneath the level of the mandibular occlusal plane.
The total mandibular subapical osteotomy involves movement of the entire mandibular dento-alveolus and primarily is used to treat dentoalveolar retrusion when pogonion position and projection are normal. As with the anterior subapical osteotomy, the horizontal osteotomy should be made at least 5 mm beneath the root apices. Individuals with dentoalveolar retrusion generally are brachycephalic with vertical deficiency of the mandible. In such cases maintaining an adequate stable inferior border segment can be difficult, and a fracture of the inferior border of the mandible can occur if less than 9 mm is between the root apices and the inferior border of the mandible. If this situation occurs, it generally can be treated with a titanium bone plate much as for a mandible fracture. The mobilized dentoalveolar segment is then stabilized in the normal fashion.
Nerve Injury.
The total alveolar subapical osteotomy can involve considerable manipulation of the inferior alveolar nerve, especially if decortication is required. Hwang et al found the mental nerve was located approximately 4.5 mm inferior to the mental foramen before its exit. If decortication of the inferior alveolar nerve is not planned, the osteotomy should be at least 6 mm beneath the mental foramen.
Bleeding.
Hemorrhage has not been reported as a significant intraoperative complication with mandibular body surgery. The most likely cause of excess intraoperative bleeding is severance of the inferior alveolar artery, which usually can be adequately controlled with packing and other direct measures.
Malpositioning of the Mobilized Segment.
Several factors may contribute to improper positioning of the mobilized segment during mandibular subapical or body osteotomies. Inadequate trimming is the most common problem encountered, especially if the subapical segment is intruded. In such cases trimming of the intact mandible on the inferior or lingual surfaces may be necessary to allow stable repositioning of the mobilized segment. When bone trimming is required it often is on the lingual aspect of the mandible. Visualization may be difficult and the mobilized segment may be excessively manipulated, causing stripping or tearing of the soft tissue pedicle. Furthermore, the amount of bone removed may be inadequate, which may result in malpositioning of the mobilized segment, especially if a thin flexible acrylic splint is used. Accurate model surgery, judicious duplication of the model surgery intraoperatively, and the use of a thick, nonflexible acrylic splint can help prevent this problem.
Sher noted that inadequate stabilization of the mobilized segment was cited by some surgeons as a difficulty with segmental surgery. With rigid fixation this generally is not a problem.
Minor Technical Difficulties.
Among the most taxing aspects of segmental mandibular surgery is trimming bony interferences while maintaining the soft tissue pedicle on the mobilized segment. This technical difficulty has important ramifications. Small segments in the mandible depend on the soft tissue pedicle and/or the inferior alveolar artery as the primary sources of blood supply. Thus stretching or tearing these tissues may compromise postoperative healing, with a wide spectrum of sequelae. As previously discussed, removing all bony interferences is essential so that the mobilized segment can be placed passively into proper position without stripping the vascular pedicles. Sher recommended leaving the crestal bone intact until all of the interdental osteotomies have been completed to avoid tearing the gingival pedicle. The crestal gingiva should be carefully manipulated so it is not torn or crushed between the segments.
4.
Mandibular Symphyseal Osteotomy (Genioplasty)
The bony genioplasty is among the most commonly performed surgical procedures in orthognathic surgery. It generally is a safe and quick procedure with few intraoperative complications. Lindquist and Obeid encountered no intraoperative complications in 31 patients who underwent genioplasties.
Unfavorable Osteotomy.
The horizontal osteotomy of the mandibular symphysis is a relatively simple and straightforward surgical procedure. The midline is marked and the osteotomy usually is performed with either a reciprocating or oscillating saw. The use of osteotomes generally is not necessary, nor is it recommended. Goracy reported fracture of the mandibular body and ramus during mobilization of the symphyseal segment while performing a genioplasty. This was most likely attributable to an incomplete osteotomy of the symphysis and the use of excessive force and torque with an osteotome in attempting to downfracture the genial segment. Osteotomes should be reserved for checking completion of the osteotomy, and bone cutting should be performed with saws or burrs.
Care must be taken when performing the osteotomy to ensure that the bone cut is at least 5 mm below the apices of the mandibular teeth. This may be difficult in the brachycephalic patient in whom the anterior mandibular height is less than normal. Measurement of the length and position of the teeth is best accomplished from periapical radiographs. Care must also be taken to ensure that the bones cut are symmetrical. Advancement of the mobilized segment also must be symmetric unless an asymmetric move is planned. Failure to appreciate intraoperative asymmetries can result in postoperative asymmetry of the chin ( Figure 20-18 ). Many methods are used to ensure intraoperative symmetry, including marking the skin, making a wide incision, and vertically scoring the anterior mandible. Davis described a simple technique of skin marking to assist in maintaining symmetry of the chin during a genioplasty.
Nerve Injury.
The mental nerve is the most likely nerve injured during the genioplasty. It courses approximately 4.5 to 5.5 mm beneath the mental foramen and is located in the region of the second premolar. The mental nerve exits the foramen and travels upward to the lower lip, where it lies just beneath the mucosa. The mental nerve may be cut during the soft tissue incision if the incision, which generally is made through the bellies of the mentalis muscles in the lower lip, is carried too far laterally. The nerve may be excessively stretched or avulsed from the mental foramen during the initial dissection or with retractors during the osteotomy. It also may be cut during the osteotomy itself ( Figure 20-19 ). This usually can be avoided if the anatomy of the mental nerve is appreciated as it courses inferiorly within the bony canal before its exit from the mental foramen.
Bleeding.
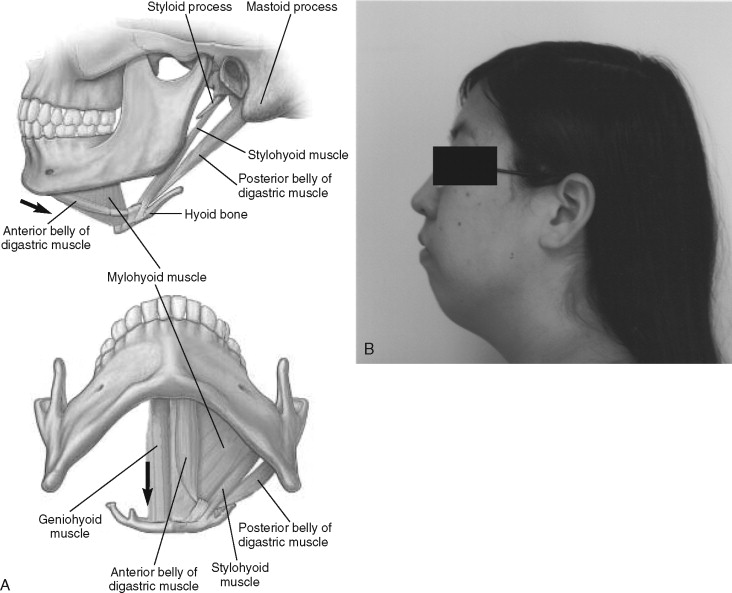
Damage to the lingual soft tissues with the saw during the osteotomy may cause intraoperative bleeding. If the saw is placed deep to the lingual cortex, damage to the genioglossus and geniohyoid muscles and laceration of the sublingual or submental arteries can occur. This can be avoided by noting the width of the symphysis on the preoperative lateral cephalometric radiograph and taking care not to allow the saw to penetrate too far beyond this depth. Lindquist and Obeid noted that when excess bleeding did occur, it usually was from severing the submental or mylohyoid arteries with the saw blade. The submental artery branches off the facial artery between 4 and 7 mm in front of the mandibular angle. It runs just beneath the inferior border of the mandible (approximately 7 mm) and courses deep to the anterior digastric muscle. The sublingual artery arises at the anterior margin of the hyoglossus and runs forward between the genioglossus and mylohyoid muscles to the sublingual gland. One branch courses behind the alveolar process of the mandible in the substance of the sublingual gland and anastomoses with its contralateral counterpart; another pierces the mylohyoid muscle and anastomoses with the submental branch of the external maxillary artery. Excess bleeding usually can be controlled with packing and local measures. However, reports of severe bleeding from laceration of the sublingual artery exist.
Malpositioning of Mobilized Segment.
The chin segment typically is stabilized with monocortical plates and screws or bicortical screws. Incorrect intraoperative positioning of the mobilized symphyseal segment can result in chin asymmetries.
Minor Technical Difficulties.
The genioplasty generally is performed bimanually, with one hand directing the saw and the other hand palpating the skin adjacent to the saw blade to ensure that the osteotomy completely transects the thick inferior border of the mandible laterally. Palpation of the skin in this area should be done gently, and pushing the skin firmly or poor control of the saw blade can result in perforation of the skin with the saw blade. If skin perforation is seen the laceration should be repaired with 5-0 nylon suture. Despite repair, scarring in this area can lead to an indentation and a visible or pigmented scar, especially in patients with thin tissues ( Figure 20-20 ). Treatment of such defects involves injection of soft tissue fillers.

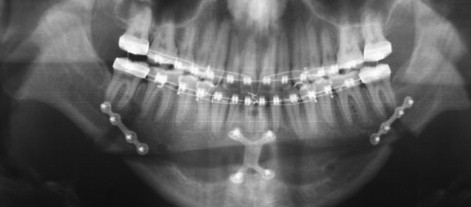
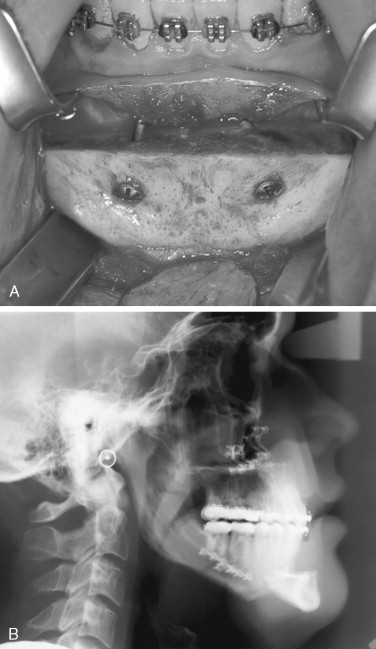
The genioplasty usually is performed after completion and stabilization of the mandibular osteotomies. If bone plates are used for stabilization of the SSRO segments, care must be taken to ensure that the genioplasty cut is in front of or beneath the hardware. The plates can be transected with the reciprocating saw, and if this goes unnoticed the proximal segment will be unstable ( Figure 20-21 ).
Incision closure may be difficult if the soft tissue incision is placed too high in the vestibule. This can result in scar bands and periodontal problems. Closure of the incision should include reapproximation of the mentalis musculature. The closure must be symmetric. The bandage should be placed symmetrically for support of the mentalis muscles and with a minimal amount of pressure.
POSTOPERATIVE PHASE OF MANDIBULAR OSTEOTOMIES
Postoperative complications generally can be divided into those seen early (within the first 3 weeks of surgery) and late (later than 3 months) postoperatively.
Early Postoperative Phase (Within 3 Weeks of Surgery)
Excessive Swelling.
The primary concern with excessive postoperative swelling after orthognathic surgery is potential airway compromise. Postoperative swelling is expected after any type of surgical procedure. Its intensity is related to many factors, such as surgical trauma, length of the surgical procedure, individual patient characteristics, and postoperative medications. Isolated mandibular surgery rarely causes massive swelling, but if this occurs it can lead to airway compromise. Gentle management of soft tissues, short surgical times, and appropriate postoperative medications generally control the edema under normal circumstances. In cases of significant postoperative swelling, release of maxillomandibular fixation (MMF), oropharyngeal suction, intubation, and ultimately tracheostomy may be considered.
Intraoperative maneuvers such as reinforced silicone low-pressure, high-volume endotracheal tubes and oxymetazoline for nasal vasoconstriction may be applied to reduce postoperative upper airway secretions and edema. Assessment of the amount of airway edema is an important extubation criterion. In cases in which significant postoperative edema can be expected, extubation is best postponed. Postoperative head-up position and an oxygen mask also may be helpful in the early postoperative period.
Fortunately, life-threatening events related to uncontrolled edema are rare after orthognathic surgery; however, cases of severe postoperative swelling have been reported.
An unusual cause of postoperative swelling with potential airway compromise is angioedema. This condition typically presents with diffuse edematous, painless, and nonpitting swelling of the soft tissues and is primarily manifested on the lips, periorbital area, extremities, and abdominal viscera. It can be hereditary or caused by allergic or idiopathic triggers. Proper diagnosis and treatment are essential because this condition can rapidly lead to life-threatening airway obstruction. Differentiation of severe traumatic edema from angioedema is imperative for appropriate treatment. Traumatic edema is isolated to the operated regions, which may include the airway, but the extremities and abdominal viscera are spared. Urticaria is not present. As previously noted, angioedema manifests in areas distant from the surgical site and may include urticaria.
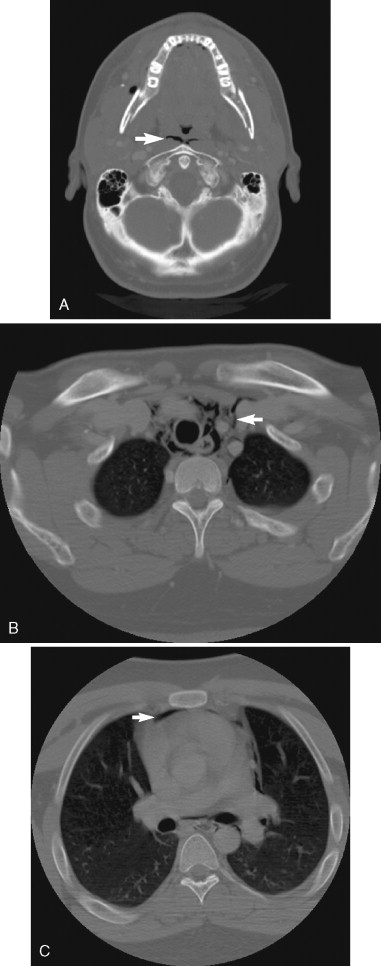
Acute angioedema is caused by either mast cell–mediated or non-mast cell–mediated mechanisms and may or may not include urticaria. Acute angioedema in the postsurgical setting is most likely a reaction to medications or contact allergens, such as latex. Airway involvement is signaled by hoarseness, difficulty controlling secretions, and odynophagia. Intermaxillary fixation should be removed and a fiberoptic nasopharyngoscopy should be performed. If laryngeal edema is present subcutaneous epinephrine (0.3 mg) can be administered and the patient should either be reintubated or a tracheostomy should be performed. After the airway is secured, corticosteroids (0.5 to 1.0 mg/kg/day) should be given, and treatment with H 1 and H 2 antagonists may be added. Serial magnetic resonance imaging or computed tomographic imaging studies should be performed to assess airway swelling and compromise, regardless of the cause ( Figure 20-22 ).
Hemorrhage and Hematoma.
Life-threatening bleeding events after orthognathic surgery are for the most part rare. The incidence of serious postoperative bleeding varies in the literature from 1% to 12.5%. Profuse postoperative hemorrhage associated with orthognathic surgery often is a consequence of an unresolved or an improperly managed intraoperative problem. With mandibular surgery it mainly is the result of damage to the facial, inferior alveolar, or internal maxillary arteries or the retromandibular vein. If such a vessel tear is not adequately repaired, profuse bleeding or extensive hematoma may arise in the early postoperative period.
The majority of hematomas are considered minor. However, a large hematoma in the floor of the mouth may obstruct the airway. Teltzrow et al reported four patients who underwent SSRO and required reoperation for treatment of massive hematomas. These hematomas were most likely related to the retromandibular vein. Lanigan reported problematic bleeding from the inferior alveolar artery. Submental artery bleeding after genioplasty may result in a hematoma on the floor of the mouth with potential airway compromise. Such a case is discussed in the genioplasty section below.
In general, minor postoperative bleeding can be controlled with local measures such as occlusive suturing and/or compression. However, when major bleeding occurs, early identification of the source of bleeding with vessel ligation is the preferred approach. When this maneuver cannot be achieved, ligation of the external carotid artery and embolization have been described as an alternative approach. Because of the rich collateral blood supply of the maxillofacial region, external carotid artery ligation may not conclusively stop the hemorrhage and may need to be combined with embolization.
Postoperative Nausea and Vomiting and Dehydration.
Perioperative complications after orthognathic surgery can be grouped into those that affect hospital stay, ability to heal, or overall patient satisfaction. Factors that may prolong hospital stay are postoperative nausea and vomiting (PONV) and BMI.
Despite all the advances in surgical technique and the development of short-acting, reliable anesthetic drugs and sophisticated monitoring equipment, PONV remains one of the most common and distressing complications after virtually all types of surgery. Although PONV usually is not a life-threatening event, persistent cases can result in adverse consequences such as dehydration, esophageal rupture, wound dehiscence, bleeding, hematoma, aspiration of gastric contents, and ultimately death.
PONV events are of special concern among orthognathic patients. Lip numbness, orofacial swelling, and an altered diet (full liquids) after surgery, worsened by jaw immobilization, may rapidly cause dehydration.
Many studies have found a high prevalence of PONV among ophthalmologic (80%), otolaryngologic (70%), and abdominal (40% to 77%) surgeries. However, few studies have reported such prevalence after oral and maxillofacial surgeries.
Perrott et al found PONV to be the most common postoperative complication in oral and maxillofacial surgery. Silva et al were the first to investigate the prevalence of PONV in patients undergoing orthognathic surgery. The authors studied 514 patients and reported a 40% prevalence of PONV. The main risk factors observed were female gender, predisposing PONV factors (history of motion sickness, prior PONV, vertigo, and migraine headaches), surgical site, procedure duration, volatile general anesthetic use, postoperative opioid use, and high postoperative pain level.
Administration of antiemetic drugs for the prevention or treatment of PONV is an important tool that should be properly used. No consensus regarding the optimal prophylactic antiemetic regimen currently exists. The use of more than one prophylactic antiemetic drug, acting at different receptor sites, has been suggested to be more effective than the use of a single drug. However, antiemetic prophylaxis alone is not the only preventive factor to be considered. The literature has suggested that, in high-risk patients, a multimodal approach (volatile anesthetic avoidance and antiemetic administration) has demonstrated the best results.
Infection.
The rate of infection after orthognathic surgery has been reported in the literature as ranging from 3.4% to as high as 60%. The great disparity in these infection rates is from a variety of factors, such as the patient’s overall medical status, the surgical site, extent of the surgical procedure, amount of hardware used, surgical technique, the use of prophylactic antibiotics, presence of third molars, the patient’s oral hygiene, and the criteria used to define infection. Hardware removal, however, is a more consistent predictor for postoperative wound infection. Studies have reported the incidence of hardware removal after SSRO to range from 6.5% to 16%.
Postoperative infections in orthognathic surgery are more commonly seen after mandibular sagittal ramus osteotomies. Spaey et al found that 92% of the postoperative infections in their series occurred after SSRO, 6% after maxillary osteotomies, and 2% after genioplasties.
Prevention of postoperative infections after orthognathic surgery involves factors such as the patient’s immunocompetence and age, experience of the surgeon, duration of the procedure, and tissue handling. Antibiotic prophylaxis has been proposed in attempt to prevent postoperative infections. However, its efficacy is still controversial and has long been a topic of research. Most protocols maintain patients on intravenous antibiotics while in the hospital and may or may not discharge patients with antibiotics. Recent studies investigating the use of prophylactic antibiotics in orthognathic surgery concluded that routine use of postoperative antibiotics is unnecessary. However, some tout the benefits of such use.
In 1991 Heit et al conducted a survey of antibiotic use in orthognathic surgery. They observed that penicillin and cephalosporin were the drugs most commonly used. They also noted that no consistent protocols existed for the method and duration of antibiotic administration. The authors administer 1 million units of penicillin before induction and administer intravenous antibiotics during the hospital stay (less than 24 hours) every 4 to 6 hours. In patients with penicillin allergies, we use clindamycin. We generally do not discharge patients with oral antibiotics unless bone grafting was done or the patient has an increased risk of infection. If any wound healing disturbance is observed at the first postoperative visit (day 10), patients are placed on clindamycin for 10 days if not allergic.
Smoking habits can potentially increase the risk of postoperative infection. Delayed wound healing, wound dehiscence, postoperative infections, and excess scarring occur more frequently in smokers. Jones and Triplett, evaluating patients after bone grafting and dental implant placement, noted that 80% of the patients who had intraoral wound dehiscence and/or infection were active smokers, whereas nonsmokers had only a 10% prevalence of wound healing complications. Hollinger et al, using an animal wound model, concluded that nicotine administration hindered bone regeneration for up to 4 weeks. Nicotine also is associated with delayed revascularization of cancellous bone grafts, a smaller percentage of total revascularization within the graft, and a higher percentage of bone graft necrosis.
However, despite theses findings, no studies have quantified a statistical relation between smoking habits and postoperative infections after orthognathic surgery.
Neurologic Dysfunction.
Several cranial nerves are at risk during mandibular orthognathic surgery, including the inferior alveolar and lingual branches of V 3 and VII. Depending on the type of injury and patient’s age, such nerve dysfunction may last from several weeks to many months. Fortunately, most of these injuries are temporary, but permanent damage also can occur.
Inferior Alveolar Nerve.
Inferior alveolar nerve (IAN) injury is the most frequent neurologic complication after SSRO and genioplasty. Regardless of the anatomic variability and the surgeon’s technical skills, almost all patients will have some sort of IAN dysfunction after mandibular osteotomy. The neurologic complications reported usually include hypoesthesia, paresthesia, and anesthesia of sensory nerves in the area of the osteotomy.
The incidence of NSD varies from 0% to 94% depending on the method of testing, surgical procedure, and follow-up period. Westermark et al observed an incidence of NSD of 39% after SSRO, 19% after external vertical ramus osteotomy, 12% after genioplasty, and 6% after (IVRO). Because of the nature of the surgical technique, the IVRO is among the least traumatic osteotomies to the IAN. The main advantage of the IVRO over the SSRO is the comparatively low incidence of NSDs, ranging from 0% to 35%. Neurologic dysfunction after sagittal ramus osteotomy ranges from 10% to 85%. Phillips et al observed that patients who report greater discomfort with altered sensation after bilateral sagittal split osteotomy (BSSO) tend to report positive symptoms such as paresthesias and pain and also are more likely to report problems with facial function.
As previously discussed, injuries to the IAN during SSRO and genioplasty may be caused in several ways, such as partial or total tearing of the nerve during sawing, drilling, splitting or chiseling; adherence of the nerve to the proximal segment after splitting; stretching of the nerve during segment mobilization; and direct manipulation of the nerve. The age of the patient at the time of surgery, amount of the mandibular movement, and type of fixation also may affect neurosensory recovery. Osteosynthesis may induce injuries to the IAN by compression of the nerve during fixation or direct injury to the nerve. Many studies have found increased NSD when more than one of these factors occurred together. Acebal-Bianco et al and Lindquist and Obeid noted a higher incidence of NSD in patients undergoing BSSO with genioplasty than in those undergoing an isolated BSSO.
Clinical experience often shows that, despite perfectly splitting the mandible without any visible damage to the IAN, most patients have some degree of numbness in the lower lip and chin at the first postoperative visit. Westermark et al, Jones and Wolford, and Jaaskelainen et al have speculated that soft tissue dissection on the medial aspect of the mandibular ramus may stretch or compress the IAN bundle. Therefore immediate postoperative NSDs are multifactorial and can occur even with apparent absence of direct nerve damage. Despite a high incidence of early postoperative IAN paresthesia after SSRO, Al-Bishri et al reported less than 12% prevalence of a neurosensory deficit 1 year after surgery.
The literature has reported the incidence of IAN injury after IVRO to be less than 1%. Van Merkesteyn et al found that 40% of patients undergoing SSRO reported NSD, whereas only 9% of patients reported such disturbances after IVRO.
As previously discussed, nerve injury during the IVRO could occur if the osteotomy is too close to the mandibular foramen. This can be a concern, particularly in patients with very narrow mandibular rami. Accidental medial displacement of the proximal segment after completion of the osteotomy also could contribute to nerve injury.
No consensus exists regarding the best treatment approach for this common postoperative complication. The patient’s age, the degree of nerve injury (neuropraxis, neurotmesis, or axonotmesis), and the time elapsing from the injury to the beginning of treatment are the main factors for postoperative numbness.
Lingual Nerve.
NSDs of the lingual nerve have been reported but are rare after mandibular surgery. Bouwman et al evaluated the use of transbuccal positional screws for stabilization of bony segments after bilateral SSRO in 700 consecutive cases and observed a 0.6% incidence of lingual nerve dysesthesia from bicortical screw fixation.
Dissection and retraction of the lingual soft tissues as well as overdrilling and placement of excessively long bicortical screws seem to be the most common causes for lingual nerve injuries. Overpenetration when drilling or placing bicortical screws to stabilize sagittal ramus osteotomies can cause damage or impingement of the lingual nerve. Fortunately this is an uncommon event. With the use of monocortical plates and screws for fixation of SSRO, the risk of lingual nerve damage from overdrilling and overscrewing are rare.
Lingual nerve injury may impair taste. Gent et al reported the possibility of lingual taste diminution attributable to chorda tympani nerve damage when the lingual nerve was injured. The authors observed approximately 30% diminution of taste intensity in such situations. Taste returned to normal within 6 months without any treatment.
Facial Nerve.
Facial nerve palsy or weakness after orthognathic surgery is a rare but serious complication. Damage to the mandibular marginal branch of the facial nerve is well documented after extraoral surgical approaches to the mandibular ramus. After the introduction of intraoral approaches for mandibular ramus osteotomies (IVRO and BSSO), risks for facial nerve damage have been significantly reduced. However, although rare, cases have been reported. The incidence of cranial nerve VII injury after IVRO is approximately 0.38%. The mechanism of nerve injury after IVRO is believed to be caused by compression from the Merrill-Lavasseur retractor behind the posterior border of the mandibular ramus.
The majority of facial nerve injuries reported after intraoral procedures have been associated with the SSRO for mandibular setback. Behrman reported four cases (0.67%) of unilateral injury to the facial nerve in an estimated 600 patients after SSRO. Compression of the facial nerve after SSRO may be caused by several mechanisms, including compression from massive postoperative hematomas at the surgical site causing pressure and necrosis of the nerve, styloid process fracture with posterior displacement, and direct pressure from the mandibular distal segment in cases of large mandibular setbacks. Direct damage to the facial nerve from imprudent use of osteotomes also has been reported. Compressive injuries generally are temporary but do result in both functional and esthetic impairment. Tearing or rupture of the marginal mandibular nerve may be the result of trauma from an osteotome or saw during SSRO or by a sharp tip of bone protruding from a mandibular proximal segment. Such injuries may cause permanent nerve dysfunction.
The initial symptoms may be seen immediately or within a few days of surgery and last for several months. If any chance of nerve transection exists, an electrodiagnostic test should be performed. If the initial and subsequent testing is consistent with nerve transection, immediate surgical exploration and repair are indicated. If nerve disruption is ruled out, spontaneous recovery may be expected. Physical therapies such as heat, facial massage, and facial exercises performed twice daily have been recommended in such cases. Administration of vitamin B 12 and steroids also may be helpful in promoting early recovery. Whether such maneuvers decrease the severity of the injury is still unknown.
Mandibular Dysfunction.
Mandibular dysfunction, including hypomobility, reduction in bite force, and TMJ dysfunction, is commonly seen at the first postoperative visit. The surgical techniques, including the amount of soft tissue dissection, the magnitude of the advancement and other technical and biomechanical factors, no doubt play a significant role in postoperative mandibular function.
Hypomobility and bite force reduction are expected in the early postoperative phase but TMJ pain generally is not seen. Mandibular hypomobility is generally caused by surgical trauma to the mucosa, interstitial connective tissue, muscles, and enveloping periosteum as well as muscular atrophy if MMF is used. Postoperative physical therapy and jaw exercises usually resolve this situation within the first 2 months after surgery. Fortunately, after the introduction of plates and screws for mandibular fixation, the length of MMF was greatly decreased or in many cases abolished. With longer periods of MMF, degenerative changes in the TMJ and temporary atrophy of the masticatory muscles are seen.
Changes in the TMJ before and after orthognathic surgery have been investigated. The literature has shown that most patients improve their TMJ disorders after surgical jaw repositioning. However, some patients have experienced worsening of temporomandibular dysfunction symptoms. Pain, tenderness, and limitation of mouth opening are more commonly seen postoperatively in individuals who exhibited these findings before surgery.
Because the proximal segment is subjectively positioned during surgery, care must be taken to not seat the condyle forcibly into the fossa. Posterior displacement of the condyle has been cited as a causative factor in the development of TMJ disorders in patients who were asymptomatic preoperatively.
Forward projection of the mandible during the early postoperative phase, resembling surgical relapse, may be seen if forceful manipulation of the condyle causes intracapsular edema. This situation usually resolves quickly without treatment.
Reduction of bite force is always observed in the early postoperative phase after mandibular orthognathic surgery. The bite force usually remains reduced for approximately 6 weeks after surgery, after which time it gradually improves for up to 2 years. Although several studies of class III patients after mandibular setback with SSRO have demonstrated a gradual improvement of bite force, occlusal contact area and masticatory efficiency bite force and occlusal contact still remained below that of the control group.
Relapse
1.
Sagittal Ramus Osteotomy.
Relapse after mandibular sagittal ramus osteotomy has been the topic of study for years. Until recently, relapse was the single most common complication associated with this procedure; however, with the introduction of rigid internal fixation, more predictable results have been obtained. A variety of measures have been taken to prevent skeletal relapse, including overcorrection, increased splint thickness in the molar region, prolonged periods of intermaxillary fixation, cervical collars, suprahyoid myotomies, and various methods of fixation.
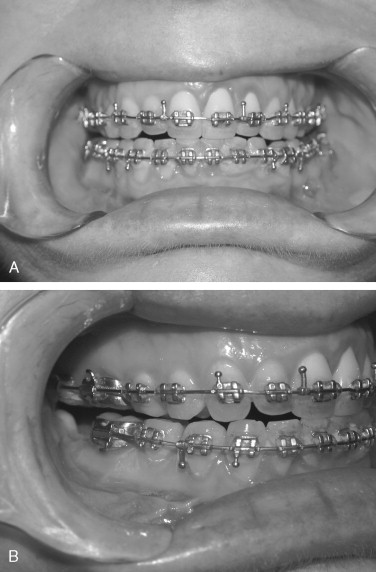
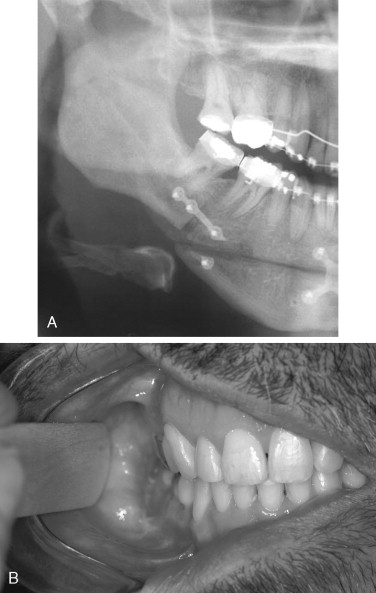
Mandibular relapse may be caused by postoperative skeletal and/or dental changes. Relapse during the first weeks after surgery is mainly caused by, hardware failure, failure to properly seat the condyle or inadequate mobilization (muscle stripping) of the mandible. Such problems may manifest as mandibular shifting with various types of malocclusion. With unilateral hardware malfunction or condylar sag, the mandible will deviate to the affected side. Bilateral condylar sag or excess muscle pull (as from the suprahyoid muscles) may cause a postoperative anterior open bite.
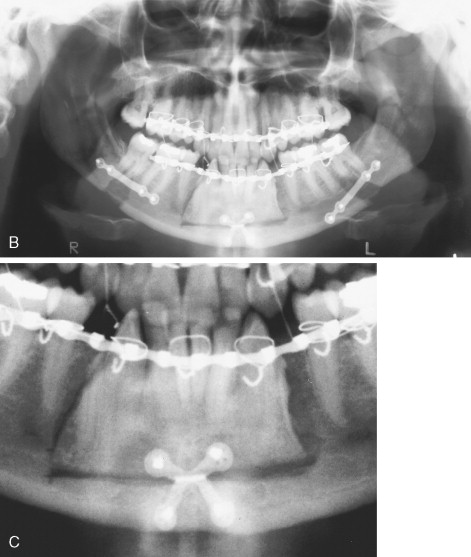
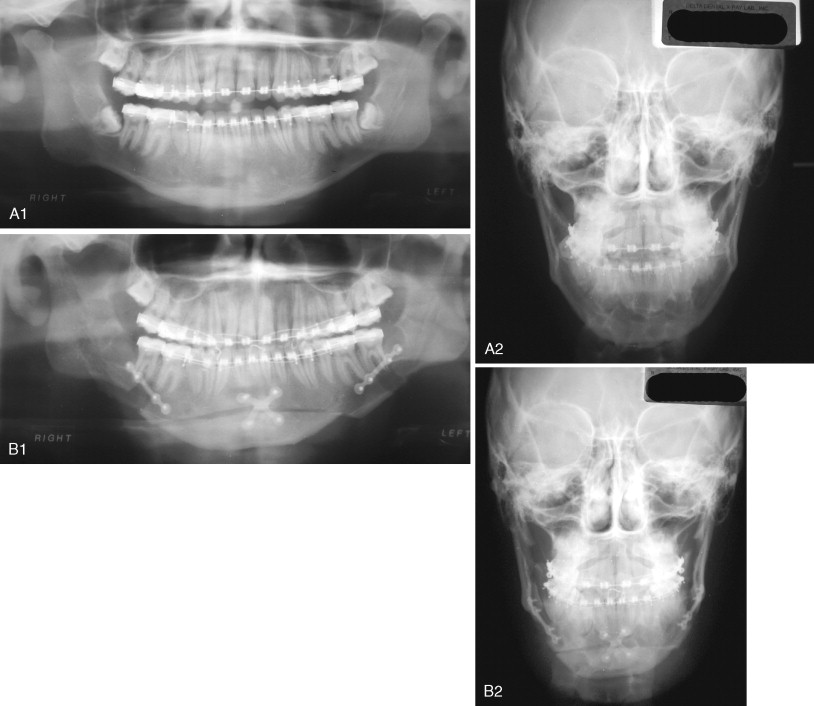
At the first postoperative visit evaluation of the occlusion is important to detect any obvious malocclusion or centric relation–centric occlusion discrepancies. Malocclusion caused by bent or broken hardware has been reported and presents with sagittal relapse toward the affected side with a possible open bite if the problem occurs bilaterally ( Figure 20-23 ). These patients may require a second surgical procedure to position the proximal segment correctly. In cases in which the hardware was bent or broken, more stable rigid internal fixation should be placed. Resorbable hardware has been used to stabilize SSRO and also can fracture. In such cases the resorbable hardware should be removed and the proximal and distal segments stabilized with titanium plates or bicortical screws.
2.
Intraoral Vertical Ramus Osteotomy.
Two to 3 weeks of MMF typically is used in patients who undergo IVRO for mandibular setback. After removal of MMF, guiding elastics are placed to help control the occlusion during healing. Elastics with a large class III vector, placed during the early postoperative phase, can cause the mandible to move posteriorly, producing a class II malocclusion ( Figure 20-24 ). Condylar sag to varying degrees may aggravate this posterior drift of the mandible as the condyles become seated in the glenoid fossae, and an open bite can result. Vertical or triangular elastics are recommended after IVRO.
Such early relapse after IVRO for mandibular setback can manifest as posterior movement and clockwise rotation of the distal segment during intermaxillary fixation with retroinclination and extrusion of the incisor teeth. Factors influencing this include proximal segment rotation and whether an open bite was corrected with the IVRO.
In addition to the above problems that can be seen in the early postoperative period after mandibular orthognathic surgery, some problems are unique to the IVRO. A prominent and palpable tip of the mandibular angle has been seen in these patients.
3.
Mandibular Symphyseal Osteotomy (Genioplasty).
In general, complications after genioplasty are not common. The most common problem observed after genioplasty is neurologic dysfunction, especially if the procedure is performed in conjunction with SSRO. The patient’s age, adjunctive mandibular procedures, soft tissue handling, and surgeon’s experience may influence the rate of postoperative NSD. Patients undergoing a genioplasty combined with SSRO have an increased rate of neurosensory deficit (greater than 40%). Gentle soft tissue dissection and proper osteotomy design, as well as taking care to avoid the mental nerve as it loops inferiorly beneath the foramen, are the most important surgical steps in preventing permanent NSDs. Ritter et al and Ousterhout stated that a distance of at least 6 mm below the mental foramen should be preserved to avoid nerve damage during mandibular symphyseal osteotomies.
Chin asymmetries may be seen early postoperatively and if noted should be corrected, either in the clinic or the operating room, depending on the patient and treatment needed. This complication can be minimized or avoided with proper planning and by using reference bone marks intraoperatively.
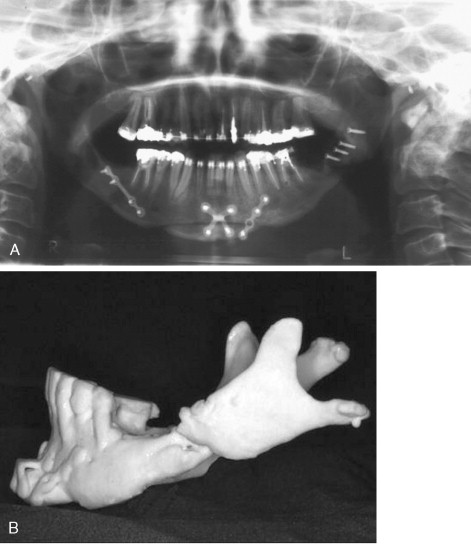
The chin segment, if insufficiently stabilized, may be displaced by pull from the suprahyoid musculature ( Figure 20-25 ). This must be corrected as soon as it is identified. With large advancements, especially in cases in which the suprahyoid muscles appear tight preoperatively, bicortical screw fixation will reduce the chances of segment mobility or displacement ( Figure 20-26 ).

Mandibular symphyseal osteotomy is a versatile surgical procedure with predictable results. Despite the stability provided by rigid internal fixation, skeletal relapse may still occur. Shaughnessy et al, evaluating long-term stability after genioplasties for chin advancement, observed an 8% rate of skeletal relapse after 3 years. The authors believed that such relapses were primarily attributable to bone remodeling. If a chin plate is used to stabilize the genial segment, bone remodeling beneath the bend in the plate may predispose patients with thin, soft tissues to plate palpability. In such cases bicortical screws may be a better choice for fixation.
With vertical reductions or large chin setbacks, care should be taken to contour the inferior border of the mobilized segment and stable mandible to remove any bony prominences. This region can be easily palpated by the patient and may be annoying postoperatively.
Bilateral or unilateral uneven mentalis muscle contraction can be seen postoperatively. This phenomenon is characterized by small involuntary muscle contractions that are clinically manifested by an unsightly contraction of the mental skin during animation ( Figure 20-27 ). This may be attributable to placement of the suture too deeply when reapproximating the mentalis muscles during closure. The best treatment for this complication consists of injection of 10 to 20 units of botulinum toxin A. In cases of persistent muscle hyperactivity, Botox reapplication should be performed.
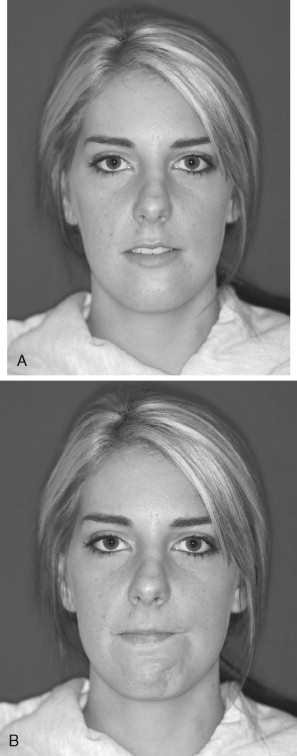
Postoperative periodontal complications may be seen and can be caused by preexisting lack of attached gingival tissue and/or improper incision design (see Figure 20-1, B ). Postoperative hematoma and infection also have been reported and can lead to scar band formation. Large hematomas after genioplasty are likely the result of damage to a branch of the submental artery ( Figure 20-28 ). In such cases control of the bleeding and evacuation of the hematoma must be done in a controlled situation in the operating room. The airway is best secured with a fiberoptic intubation and the wound reopened. The source of bleeding must be identified, which may require mobilizing the genial segment (see Figure 20-28, B ). Fixation of the genial segment is removed and the segment retracted downward. The hematoma can be evacuated (see Figure 20-28, C ) and the bleeding source, generally in the sublingual tissues, can be identified and controlled. The mobilized segment is then resecured into position.

Chin ptosis, not necessarily seen in the very early postoperative phase, has been attributed to inadequate mentalis muscle reattachment. Chin ptosis becomes more apparent as the healing process proceeds. With large chin advancements or with downgrafting, interpositional grafts should be planned to avoid nonunion or postoperative chin displacement. Late postoperative infections can be seen with alloplastic chin implants but are uncommon after bony surgery of the chin. Figure 20-29 demonstrates a late postoperative infection (after more than 2 years) of a Medpore chin implant that had been placed transorally. The implant required removal with excision of the cutaneous fistula.
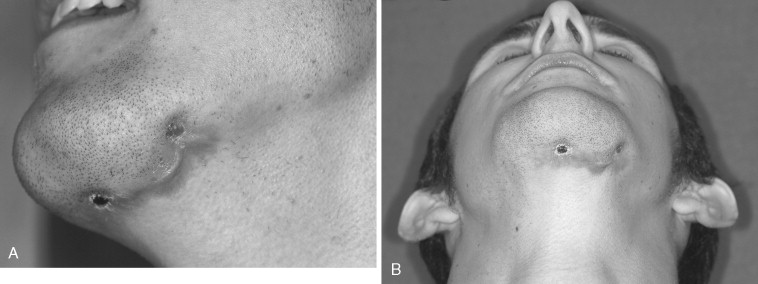
Late Postoperative Phase
Postoperative complications after mandibular surgery seen in the late phase of treatment include long-term neurologic dysfunction, TMJ dysfunction, dental and periodontal problems, late relapse either from growth or condylar remodeling/resorption, and loss of gonial angle projection.
Neurologic Dysfunction.
Because of the low incidence of NSD after IVRO, long-term disturbance usually is not common. For this reason this section focuses on long-term NSD after the sagittal ramus osteotomies and genioplasty. The incidence of long-term neurologic dysfunction after SSRO ranges from 5% to as high as 70%.
Early postoperative paresthesia after SSRO is expected, and the incidence is likely close to 100%. However, only a small percentage of these patients demonstrates persistent loss of sensation. MacIntosh reported an 85% incidence of immediate postoperative paresthesia and a persistent NSD in 9% of patients 1 year after surgery. He also noted that it was most commonly seen in patients older than 40 years. Westermark et al and Gianni et al observed a rate of approximately 14% of NSD 1 year after surgery. Tactile sensitivity recovers along a topographic distribution, with the greatest sensory loss in the most distal areas, such as the vermilion border and chin midline. Thermal sensitivity appears to be preserved even in patients with long-term neurosensory deficits.
Many factors can lead to or predispose patients to long-term postoperative paresthesia. The degree of nerve damage intraoperatively, the influence of concomitant genioplasties, patient age at the time of surgery, and surgeon experience have been cited as risk factors for long-lasting NSD.
Most patients spontaneously recover from NSD within 6 months (85%), although some cases may persist for more than 1 year or become permanent. Even in patients with long-term neurosensory defects, the majority of individuals adapt and few describe these alterations as disabling.
TMJ Dysfunction.
Symptoms of temporomandibular dysfunction (TMD) include pain in the preauricular area, TM joint, or muscles of mastication; limitation or deviation in mandibular range of motion; and TMJ sounds (clicking, popping, crepitus) during mandibular function. Symptoms also may include headache, neck ache, face ache, and earache.
The exact effect of orthognathic surgery on the TMJ has not been fully determined. Some studies have reported improvement, deterioration, or no change at all in TMJ symptoms after orthognathic surgery. However, in patients with preoperative symptoms, most studies have demonstrated a favorable effect of orthognathic surgery on TMJ dysfunction, possibly because of improved occlusal stability or reduced emotional stress.
In 2002, Dervis et al noted improvement in TMJ symptoms after orthognathic surgery; however, they did not observe a relation between the severity of TMJ symptoms and the patient’s dentofacial disharmony.
TMD, commonly seen in the orthognathic patient population, should be documented preoperatively to establish a baseline for later comparison. Westermark et al found a 43% incidence of subjective TMD symptoms in a large group of patients before orthognathic surgery and a 28% incidence of TMD 2 years postoperatively. They found that individuals with mandibular retrognathia did not improve as much as patients with mandibular prognathia, and the SSRO was less effective in improving TMD symptoms than was the IVRO. Patients with mandibular hypoplasia, especially those with high mandibular plane angles, have been shown to have a higher incidence of TMJ dysfunction than do patients with mandibular prognathism. Individuals with an open bite component to their deformity are thought to be at greater risk for postoperative TMD and may be predisposed to idiopathic condylar resorption.
Radiographic evidence of TMJ remodeling after orthognathic surgery is not uncommon and is not necessarily correlated with symptomatic TMD.
Dental and Periodontal Problems.
Dental and periodontal problems after SSRO and genioplasty often are related to poor incision placement with scar contracture. When the incisions are placed too close to the attached gingiva, tension on the attached tissue can predispose the patient to gingival recession. A tight scar band in the lateral ramus area can heal such that a crevice is formed between the molars and the scar, making hygiene difficult. This also can be seen in cases of mandibular setback if the proximal segment is not trimmed so that it is flush with the distal segment.
Late Relapse.
Late relapse after healing can be the result of one or several factors, including postoperative growth, orthodontic relapse, or TMJ remodeling and/or resorption. Regarding isolated mandibular surgery, late postoperative growth is a risk associated with mandibular setback, especially in male patients, who may demonstrate continued mandibular growth well into their 20s. Skeletal maturity and facial growth have been assessed by serial cephalometric radiographs, hand-wrist films, and skeletal scintigraphy (technetium 99).
Orthodontic relapse, especially in patients who have undergone orthodontic maxillary expansion, may contribute to relapse and manifest as an anterior open bite. Transverse collapse of the expanded maxillary dentition results in a cusp-to-cusp occlusion. Identification of such patients before surgery is ideal so that dental compensations can be removed preoperatively. The best way to determine if transverse collapse has occurred is to compare the starting dental study models with those taken after the orthodontics has been completed.
Idiopathic Condylar Resorption.
Condylar remodeling, periodically seen after mandibular surgery, can be a natural response to forceful seating of the condyle during surgery. Such remodeling can continue for several years after surgery.
Idiopathic condylar resorption (ICR), a condition without a known etiology, can occur in isolation or after mandibular and/or maxillary surgery. Loss of condylar height results in mandibular retrognathia and an anterior open bite. Features of ICR usually are seen in female patients between the ages of 15 and 35 years (usually more frequent in teenage girls) and include the following: it usually is symmetric and bilateral; it results in progressive resorption of the condyles, with a gradual loss of mandibular projection and posterior ramal height; it has no inciting factor; although joint noise may be present, TMJ function is largely preserved; and it is a self-limiting process once the condyles have resorbed to the level of the sigmoid notch. Two main theories regarding the etiology have been discussed and include hormone-mediated synovial hyperplasia with resulting condylar resorption and avascular necrosis with resulting condylysis. Some believe that ICR is more commonly seen in female patients with high mandibular plane angles and class II open bite malocclusions who have an abnormal response to condylar loading. Forced condylar positioning during surgery may lead to late condylar remodeling and thus late postoperative relapse.
Once ICR is identified several approaches have been advocated. Splint therapy generally is recommended with a view toward “unloading” the TMJs and also as a way to monitor progression of the disease. Definitive treatment should be postponed until relative certainty exists that the condylysis has “burned out” and the occlusion has been stable for at least 1 year before treatment. Technetium 99 methylene diphosphate quantitative condylar bone scintigraphy can be used to ascertain whether any activity is left in the condyles. If the 99 Tc scan is positive, definitive occlusal correction should be deferred. Other options for treatment of this disorder include bilateral TMJ resection and reconstruction and distraction osteogenesis. With the latter, ensuring that the resorptive process is finished is important.
When the patient’s functional status or psychological situation is such that postponing surgery is not an option, postoperative relapse may be expected if the TMJs are left intact and only occlusal correction is performed. The amount of such relapse is unpredictable. The real etiology and pathogenesis of condylar resorption after orthognathic surgery still remains unclear.
Loss of Gonial Projection
Proximal Segment Rotation.
Varying degrees of proximal segment rotation have been observed after BSSO. More commonly seen in the era of wire fixation, clockwise rotation of the proximal segment results in loss of gonial angle projection and accentuation of the antegonial notch. Some degree of remodeling of the proximal segment is part of the healing process. However, care should be taken during stabilization of the proximal segment with the SSRO to ensure that superior rotation is avoided. In cases in which insufficient bone contact is achieved intraoperatively, or if stabilization of the proximal segment is inadequate, proximal segment rotation can occur postoperatively ( Figure 20-30 ). This is more common with semirigid fixation (monocortical screws and plates) than with bicortical rigid internal fixation. In cases in which the degree of proximal segment rotation is minor, treatment may not be necessary. If the patient has esthetic concerns, an alloplastic ramus implant to augment the mandibular angle and fill in the antegonial notch may be successful treatment. In more severe cases, however, reoperation may be required for adequate proximal segment repositioning with possible bone grafting.
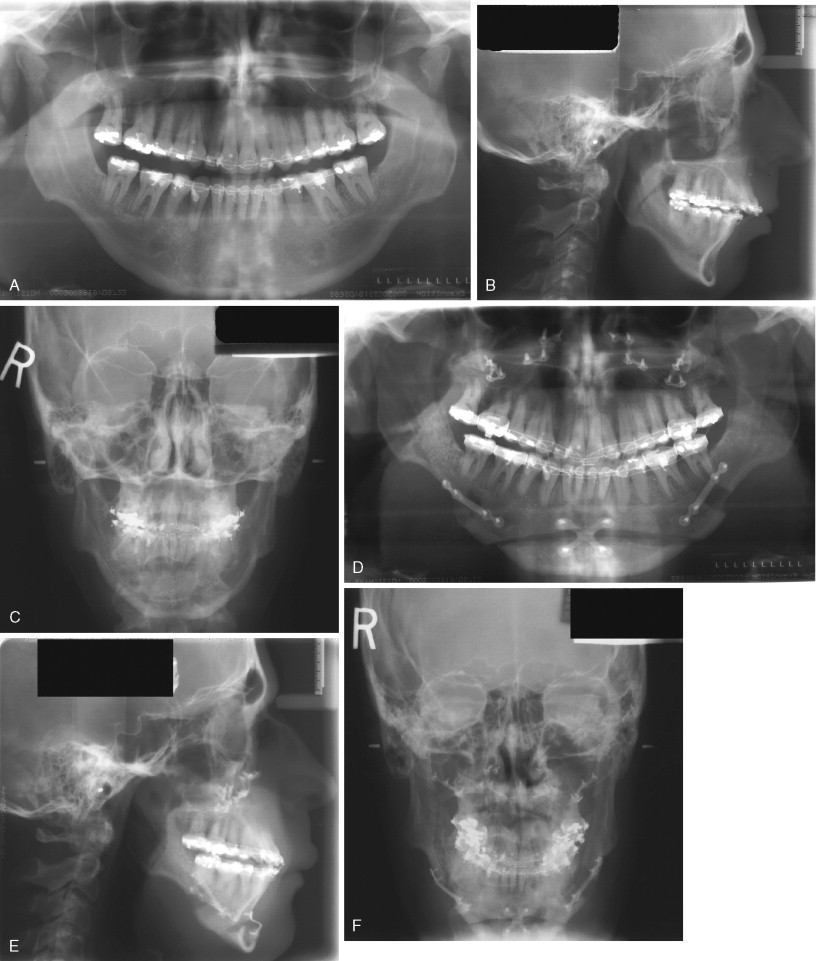

The best advice regarding complications is to try to prevent them. Recommendations from the authors’ experience in this regard are summarized in Table 20-1 .
| Complications | Avoidance | |
|---|---|---|
| Preoperatively |
|
|
| Intraoperatively |
|
|
| Postoperatively |
|
|
MANDIBULAR SURGERY
PREOPERATIVE PHASE
The preoperative phase consists of diagnosis and treatment planning as well as any necessary presurgical orthodontics. Regardless of the type of mandibular surgery, certain basic preoperative orthodontic principles must be applied to reduce the chances for relapse and unacceptable results.
1.
Eliminate Dental Compensations
Dental compensations, to varying degrees, are present in the majority of patients undergoing orthognathic surgery. Decisions regarding dental extractions required to eliminate these compensations should be made at the beginning of treatment. Failure to remove dental compensations can contribute to compromised functional and esthetic results.
The primary goals of presurgical orthodontics are to place the teeth over basal bone, maximize the surgical correction, and ensure dental stability. Surgical relapse, in varying degrees, may occur after mandibular surgery. Removal of dental compensations orthodontically can help counterbalance orthodontic and surgical relapse. Incisor position is heavily influenced by the decision to extract teeth. Liberal extraction practices were largely halted with the teachings of Angle early in the twentieth century. This trend was somewhat reversed mid-century, with studies indicating improved orthodontic results when certain cases were combined with extraction therapy. The pendulum has swung back to nonextraction orthodontic treatment in recent decades, and this trend has occurred in surgical patients as well. Serial surveys of orthodontic diagnosis and treatment have indicated that the percentage of cases treated with extraction therapy has decreased from 34.9% in 1986 to 20% in 2002.
In the patient with mandibular deficiency and a class II division 1 malocclusion, dental compensations often include flared lower incisors. Proper position of the lower incisors (90 to 93 degrees to the mandibular plane) is the presurgical orthodontic goal. Preoperative orthodontics should be directed toward uprighting the lower incisors and accentuating the class II malocclusion before mandibular advancement. This can be achieved with appropriate extractions, if necessary, and class III elastics. Failure to remove these compensations before surgery reduces the magnitude of mandibular advancement and compromises the esthetic result if an advancement genioplasty is also needed ( Figure 20-1 ). The greater the proclination of the mandibular incisors, the smaller the magnitude of mandibular advancement that can be surgically achieved. Additionally, lower incisor flaring increases the Holdaway ratio to greater than 1 : 1 and an advancement genioplasty, although necessary for proper esthetics, cannot be achieved without making the labiomental fold excessively deep ( Figure 20-2 ).
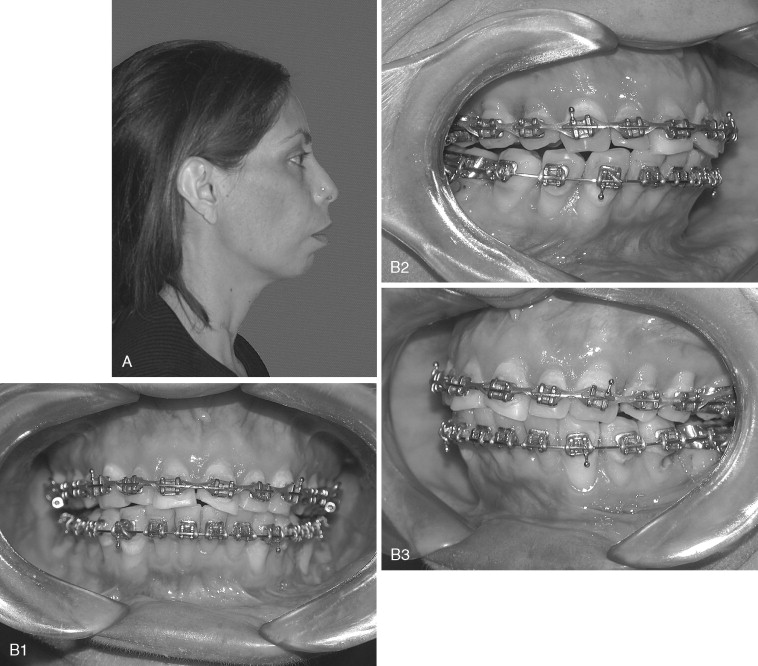

In the patient with mandibular prognathism who is planned for mandibular setback, dental compensations are removed by the opposite presurgical orthodontic mechanics. Dental compensations in the class III patient commonly include flaring of the maxillary incisors and retrusion of the mandibular incisors. Extractions may be necessary in the maxillary arch to position the maxillary incisors properly (120 degrees to the Frankfort plane or 102 to 104 degrees to Sella-nasion). Proper position of the dentition also may include preoperative class II elastics. Failure to remove compensations in the class III patient can reduce the amount of mandibular setback and maxillary advancement that can be surgically achieved ( Figure 20-3 ).
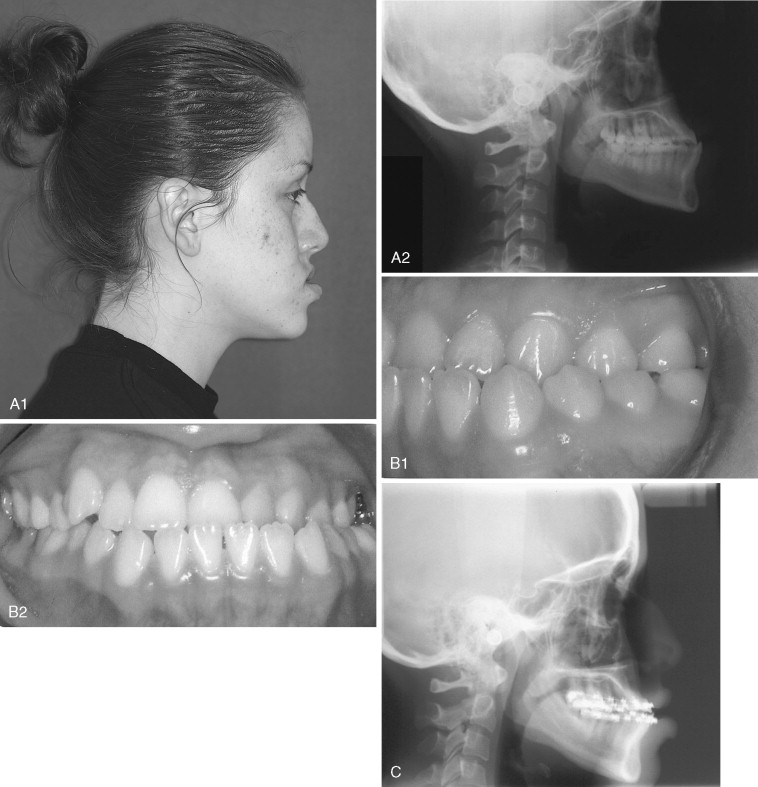
In patients with an accentuated curve of Spee and an accompanying class II division 1 deep bite malocclusion, leveling of the occlusal plane is best done after mandibular advancement. The mandibular incisors should be left in the preorthodontic position, and attempts to level the occlusal plane before surgery should be avoided. In such patients increased lower facial length is needed and esthetic results will be superior if the leveling is accomplished after surgery. The surgical-orthodontic setup is placed in a “tripod” position with contact of the terminal molars and incisors. Postoperative leveling in these cases usually proceeds relatively quickly.
2.
Failure to Manage Transverse Discrepancies Properly
Management of transverse discrepancies in children and adolescents by conventional orthodontic therapy often is successful. In adult patients (older than 16 to 18 years) with transverse maxillary deficiency, orthopedic expansion primarily consists of alveolar or dental tipping with little or no basal skeletal movement. Orthodontic treatment of skeletal transverse maxillary deficiencies should be reserved for discrepancies of less than approximately 5 mm. In these cases buccal orthodontic movement of the maxillary molars and lingual tipping of the mandibular molars can lead to a stable and predictable result. However, periodontal status and thickness of the alveolar buccal bone at the molar level may limit such maneuvers. Orthodontic or orthopedic maxillary expansion greater than 5 mm in adults may be unstable and could potentially lead to gingival recession, buccal bone resorption, root fenestration, and/or resorption.
Relapse of the expansion can lead to an anterior open bite because the effective length of the maxillary molars is increased, resulting in clockwise (posterior) autorotation of the mandible. Handelman et al noted this in several cases they analyzed after surgical mandibular advancement. They found what clinically appeared to be horizontal mandibular relapse, but it was in fact from orthodontic relapse of transverse maxillary expansion resulting in clockwise rotation of the mandible.
3.
Identify and Manage Tooth Size Discrepancies
A tooth size discrepancy, as determined by Bolton’s analysis, is common in surgical patients. In the class II patient with mandibular deficiency, failure to manage tooth size discrepancies may prevent the surgeon from achieving a class I cuspid occlusion and proper anterior coupling with adequate overjet and overbite ( Figure 20-4 ). Tooth size discrepancies are best determined from models. When a tooth size discrepancy is identified a decision should be made regarding the method and timing of treatment. The authors recommend treating tooth size discrepancies before surgery because this allows the surgeon to achieve a better fit of the anterior occlusion, especially in the cuspid regions. This can be preoperatively corrected in a number of ways, including stripping the mandibular incisors, creating spaces distal to the maxillary lateral incisors, or removing a mandibular incisor, depending on the magnitude of the discrepancy. In the patient undergoing mandibular advancement, spaces distal to the maxillary lateral incisors will allow a greater degree of mandibular advancement and assist the orthodontist in finishing the case if relapse occurs.
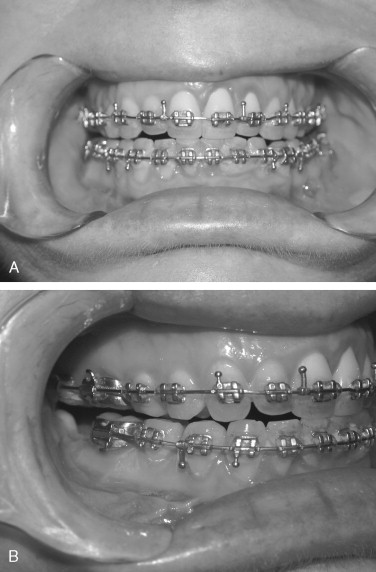
4.
Ensure Proper Leveling and Root Divergence in Segmental Cases
Preoperative orthodontics in cases of segmental mandibular surgery may include leveling of the individual segments. Proper leveling of the teeth adjacent to the osteotomy should been achieved, especially on the segment to be mobilized. For example, if a deep bite deformity exists and surgical intrusion of the anterior mandibular segment is planned, a rainbow curve of Spee must be leveled such that when the segment is moved inferiorly the cuspids are not buried below the level of the occlusal plane. This situation will lead to both orthodontic and periodontal problems. With segmental surgery, adequate space between the proposed tooth roots must exist. Inadequate interdental space increases the likelihood of damage to adjacent tooth roots.
5.
Prepare the Patient Psychologically for Surgery
Patients can be dissatisfied with the outcome of treatment despite a surgical success when a discrepancy exists between the expected and actual impact of treatment on the patient’s life. Flanary et al found that effective, continuous communication among the patient, surgeon, and orthodontist was among the most important factors in patient satisfaction with the surgical results. Nagamine et al found 22% of their 65 patients who had surgical correction of mandibular prognathism were dissatisfied with their results. Among the primary reasons for dissatisfaction were forward relapse of the mandible and paresthesia of the lower lip.
With the advent of video imaging, patients have been able to visualize treatment results more clearly. Some studies have indicated that video image predictors were clinically acceptable in cases of isolated mandibular surgery. However, with bimaxillary surgery video imaging may not be as accurate as initially hoped.
INTRAOPERATIVE PHASE
Intraoperative complications are often attributable to improper surgical technique and/or failure to appreciate the patient’s anatomy; however, unanticipated intraoperative complications also can occur. Intraoperative complications are discussed below for the following mandibular procedures and, when applicable, are divided into the following categories: (1) unfavorable osteotomy split, (2) nerve injury, (3) bleeding, (4) proximal segment malpositioning, and (5) miscellaneous technical difficulties.
1.
Sagittal Ramus Osteotomy
The sagittal ramus osteotomy is among the most frequently performed surgical procedures in the mandibular ramus. It is used both for mandibular advancement and mandibular setback. The intraoral sagittal osteotomy was first described by Schuchart and was modified and popularized by Trauner and Obwegeser. Obwegeser carried the medial osteotomy to the posterior border of the mandible and the vertical limb to the region of the antegonial notch. DalPont modified the osteotomy to extend further forward into the body of the mandible, and Hunsuck limited the extent of the medial cut to the retrolingular fovea. Epker further modified the technique by limiting the soft tissue dissection. Despite its frequent use, the sagittal ramus osteotomy is a technically difficult procedure. A number of authors have presented their experience with intraoperative complications with this procedure.
Unfavorable Osteotomy Split.
One of the most common problems associated with the sagittal split ramus osteotomy (SSRO) is unfavorable fracture of either the proximal or distal segment: incidence rates as high as 18% have been reported for these types of fractures. Once this so-called “bad split” occurs, a decision must be made regarding its treatment. One can either correct the bad split and complete the operation or abort the procedure and allow the patient to heal. It is the better part of valor to stop the operation, with a plan to reoperate after the bone has healed, if good bone contact most likely cannot be achieved ( Figure 20-5 ). This decision must be made on a case-by-case basis. Reoperating on a well-healed mandible is far easier than trying to valiantly complete the procedure and end with a nonunion from poor bone contact.
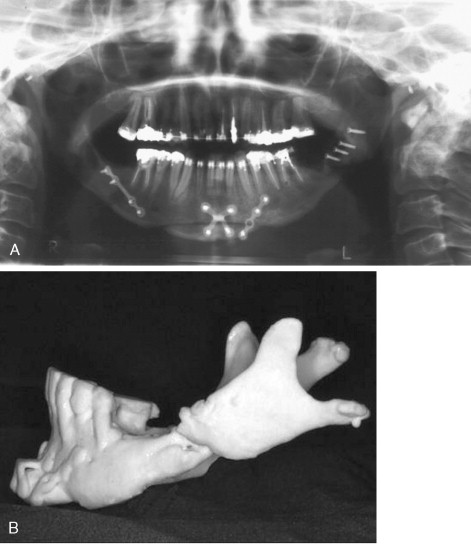
Proximal segment fracture, also known as a buccal plate fracture, is the most frequent type of unfavorable split. Several contributing factors have been cited: presence of an impacted third molar, recent removal of a third molar, age of the patient, and extent of the surgeon’s experience. In an analysis of 1256 patients who underwent sagittal osteotomy, Precious et al found that fracture of the proximal segment was more common than fracture of the distal segment (70% versus 30%). The authors did not observe any relation between proximal segment fractures and the presence of third molars, but they did note such a relation with distal segment fractures when the third molars were present.
Behrman and later Turvey reported a 3% incidence of proximal segment fracture during SSRO, and MacIntosh found a 6.6% incidence of such fractures.
Mehra et al found that fracture of the distal segment occurred more often in younger patients with impacted third molars, whereas fracture of the proximal segment was seen more often in older patients without third molars. In a group of 70 patients, Reyneke et al found three fractures of the distal segment and one fracture of the proximal segment. They observed that the presence of the third molars in young patients (younger than 20 years) was correlated with a higher rate of unfavorable fractures. The role of impacted third molars in unfavorable splits is controversial. Some believe feel that removal of third molars at least 6 months before SSRO is important in reducing the risk for adverse fractures, whereas others believe that third molars do not predispose the patient to such problems. The direction of mandibular movement, degree of impaction of the third molar, and experience of the surgeon are factors to be considered in the decision to remove third molars preoperatively. Removal of the third molars at the time of orthognathic surgery helps reduce costs and avoids an additional surgical procedure.
Fracture of the buccal plate most often occurs when the inferior border of the mandible is incompletely transected ( Figure 20-6, A ). In this situation, the thin buccal plate is the area of least resistance and can be fractured by the force used to split the mandible (see Figure 20-6, B ). Once a buccal plate fracture occurs, the task of completing the split is made technically difficult because the fracture leaves the buccal plate shortened and with less bone to pry against (see Figure 20-6, C ). Mehra et al did not describe their technique for completing the osteotomy after proximal segment fracture, but these authors stabilized the free proximal segment with a bone plate and monocortical screws.
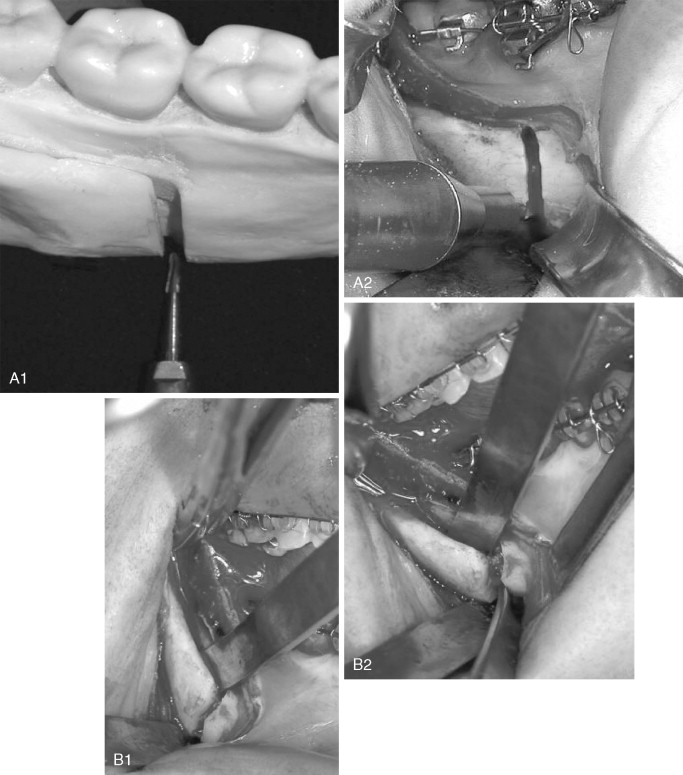
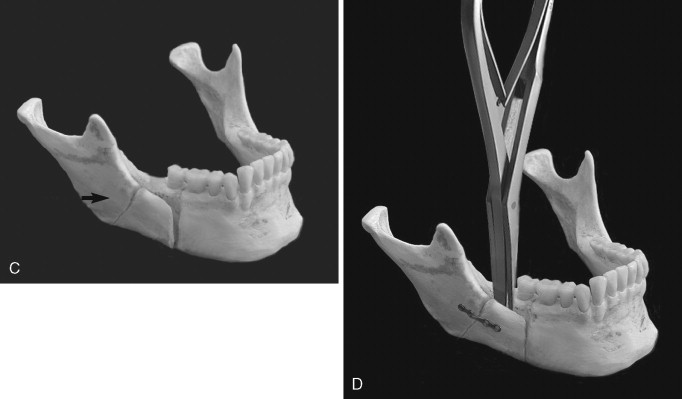
In response to a “low” fracture of the buccal plate during SSRO, the authors recommend that the buccal plate be secured with a monocortical plate immediately after it becomes fractured; the split should then be completed in the usual way (see Figure 20-6, D ). This technique is simple and quick, facilitates completion of the split, and may reduce damage to the inferior alveolar nerve that can occur when osteotomes are blindly used to finish the split.
When a high buccal plate fracture occurs near the mandibular condyle, plating the segment as described above may be difficult. Patterson and Bagby discussed fracture of the proximal segment and noted that completion of the split can be extremely difficult. To complete the split, the authors recommended lateral retraction of the remaining proximal segment and vertical osteotomy of the distal segment. Although this procedure may limit the amount of advancement and may place the lingual nerve at risk from stretching or retraction of the medial tissues, the authors have found it useful in salvaging high buccal plate fractures ( Figure 20-7 ).
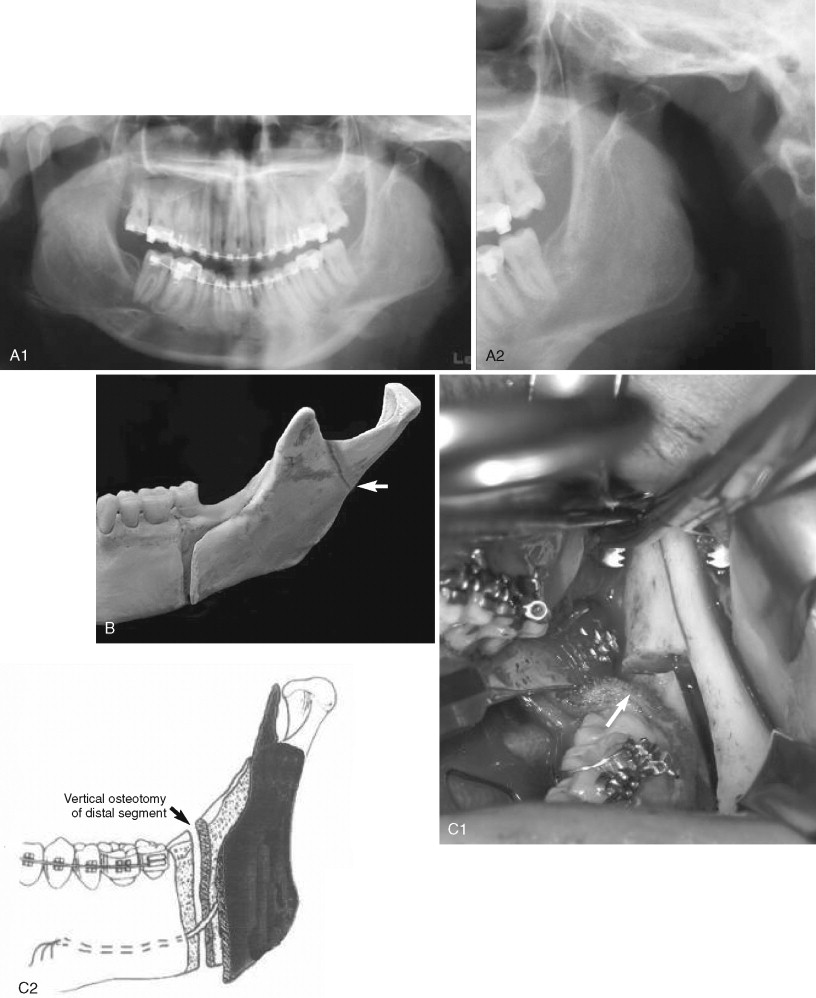
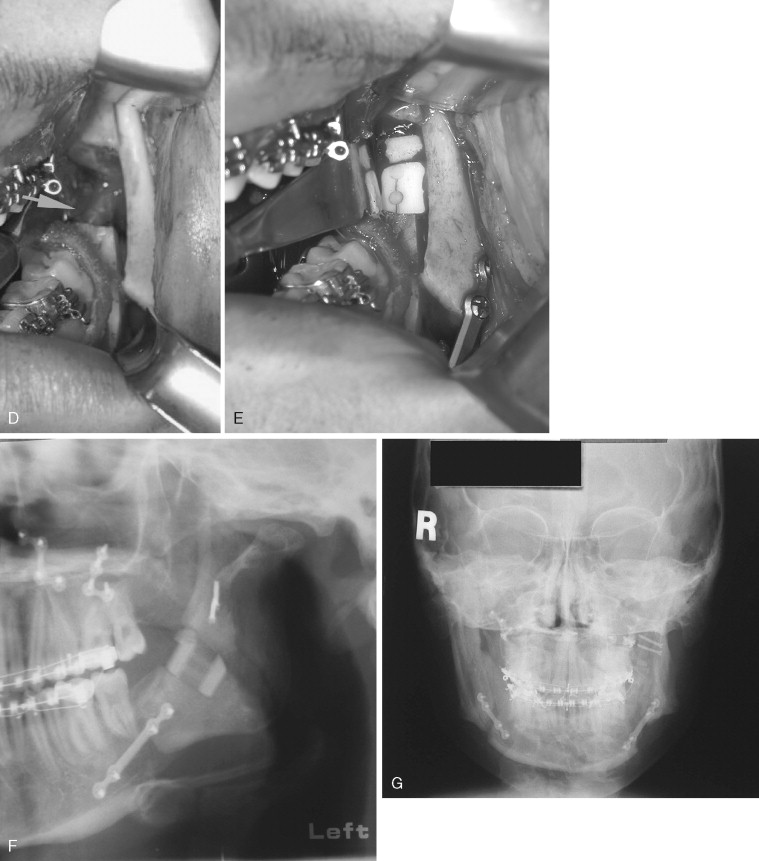
Fracture of the coronoid process of the mandible during SSRO has been reported and is likely caused by placement of the horizontal osteotomy too high where the ramus is thin. If an osteotome is used, it can penetrate the lateral ramus. Coronoid process fractures can be avoided by ensuring that the horizontal cut is not carried too far laterally and is made just above the lingula where the mandible is relatively thick. If the horizontal osteotomy is made in the thin part of the ramus, made too deeply, and carried to the posterior border of the mandible, a through-and-through osteotomy can occur, resulting in a free condyle–ramus segment ( Figure 20-8 ). This is among the most difficult types of unfavorable fractures to salvage. If possible, it must be corrected with an osteosynthesis plate, and the SSRO can be either be completed properly or aborted.
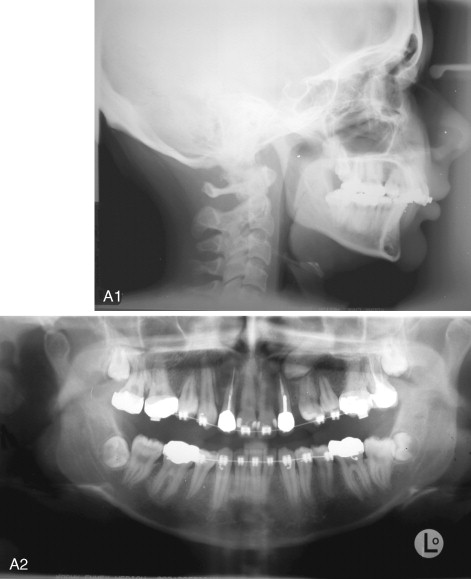
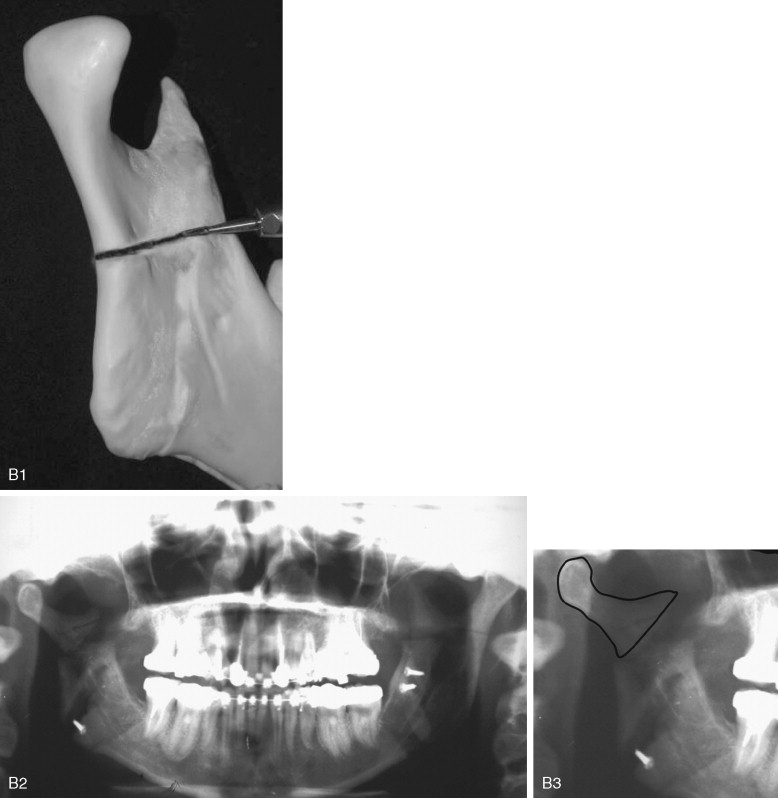
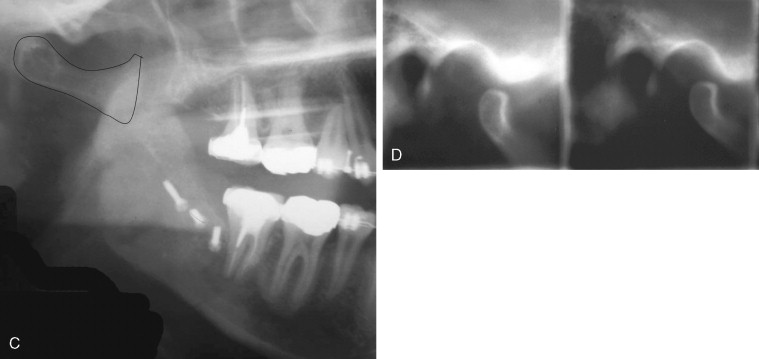
Although fracture of the buccal plate is the most common type of unfavorable fracture with the sagittal ramus osteotomy, several other types of “bad splits” also can be seen. Fracture of the distal segment during the sagittal osteotomy has been reported as an intraoperative complication. This can be encountered when the distal segment is weakened, such as when an impacted third molar is present or the patient is edentulous in the molar area, causing thinning of the mandible in this region ( Figure 20-9 ). Care must be taken if using the Smith spreader (Walter Lorenz Surgical, Jacksonville, Fla.) in applying force to the distal segment in such cases.
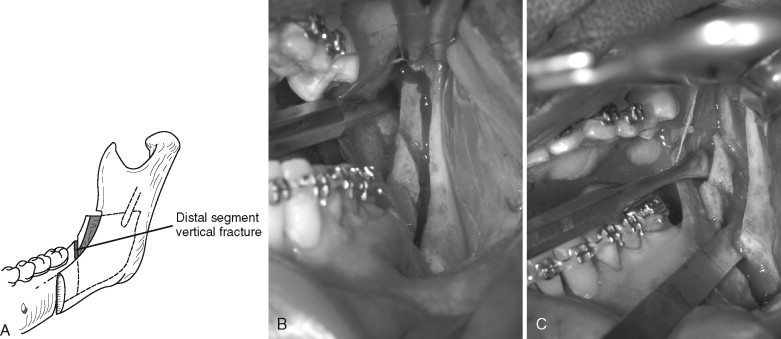
Occasionally, if the inferior border of the mandible is not transected completely and the osteotomy is split, the inferior border, which should be on the proximal segment, remains on the distal segment ( Figure 20-10 ).
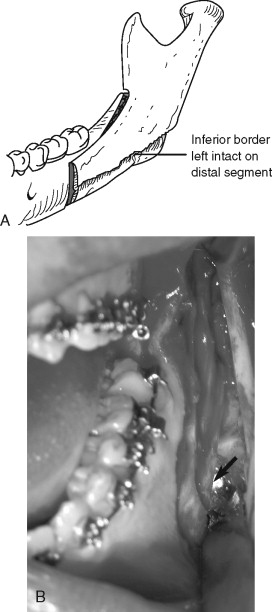
Nerve Injury.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


