Fig. 8.1
Biomaterial leakage in the maxillary sinus lumen due to an undetected membrane perforation
Direct visual inspection is the best way to detect a perforation. The movement of the elevated membrane movement while the patient is breathing from his nose gives an idea if the membrane is perforated. Postoperative radiologic examination with a periapical X-ray, a panoramic radiography, or a CBCT can be helpful after the surgery to check if there is a leakage of the biomaterial.
8.2.1.3 Timing of the Perforation
During the surgery a perforation could appear at any of these stages. During bone window trepanation if the bur passes through the bone and reaches the membrane, it can either perforate it or injure it. The use of a diamond bur when approaching to the membrane lessens this risk. The piezoelectric device has been proven to be safer (Wallace et al. 2007), considering that the diamond-coated tips do not harm the soft tissue. Following osteotomy if the bony window is to be removed, care should be taken not to tear the membrane when detaching it. Moreover, perforations can be associated with the use of air-driven high-speed rotary instruments. Anyway, dental turbines, which are always air-driven, should not be used in surgery also because of their risk of subcutaneous air emphysema. According to some authors, perforations occur more frequently during osteotomy than during the reflection of the membrane (Vlassis and Fugazzotto 1999). Reflecting the sinus membrane remains a delicate step of sinus floor elevation. The tension applied by the instrument on the sinus membrane, the buccopalatal depth of the sinus cavity, the ease of access, the thickness of the membrane, and especially the presence of septa are all factors that can complicate membrane reflection. A very delicate pressure is applied on the membrane, and without resistance the movement is repeated with small amplitude and slowly progressed. In sinuses with important buccopalatal width, the access to the medial or palatonasal wall is difficult, long neck curettes must be used, and it is crucial to keep the instrument in tight contact with the bone to prevent membrane tearing. Incomplete elevation of the sinus membrane from the medial wall is considered unfavorable for bone revascularization and remodeling.
The size of the window is a factor to be considered. If it is too small (Fig. 8.2) in order to be tissue conservative, the visual and mechanical access to the sinus is restricted, the movements of the curette are more limited, and the identification of a perforation is difficult. Sinus septa are the major cause for membrane perforation and will be discussed later. Under general anesthesia, the airways are under positive pressure, the sinus membrane is inflated, more care must be taken, and the risk of piercing seems more probable than under local anesthesia.
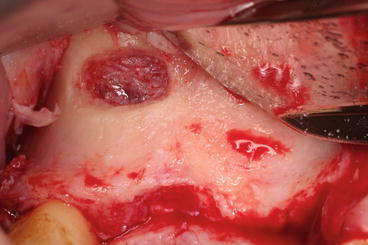
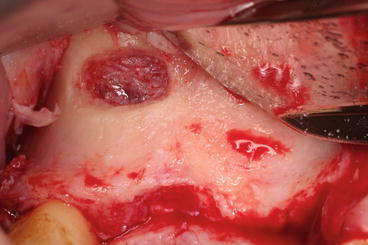
Fig. 8.2
A small lateral window has the advantage to be more conservative for the surrounding bone but allows restricted visual access to the elevated membrane
If simultaneous implant placement is planned, drilling the residual alveolar crest must be done with care in order not to perforate the membrane when the drill passes the sinus floor. A curette can be helpful to maintain the membrane high and far from the drill.
When the bone substitutes are introduced inside the sinus, there is a risk of microlacerating the membrane especially if the edges of the biomaterial are sharp. If the quantity of biomaterial filled in the cavity is very important while the surface of the elevated membrane is small, the pressure applied on the membrane can fragilize it or tear it.
If simultaneous implantation is planned, the sinus is first partially grafted by bone substitutes at the palatal side followed by implant placement before completing the grafting procedure (Fig. 8.3). Otherwise the implant insertion after complete bone substitute filling will augment the risk of tension on the membrane and perforate it intra- or postoperatively.
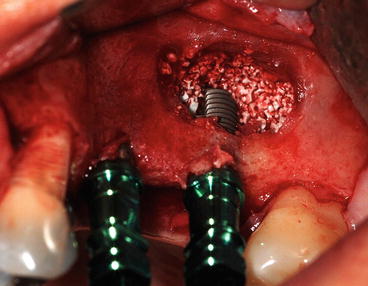
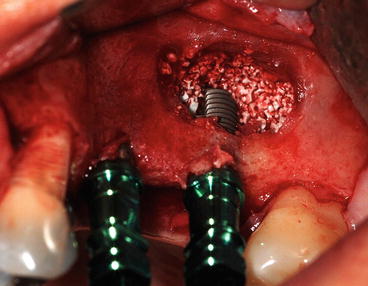
Fig. 8.3
Bone grafting the palatal side before implant placement
Membrane perforations occur during osteotomy and the reflection of the membrane. Keep the instrument in tight contact with the bone to prevent membrane tearing.
Factors that can increase the risk of membrane perforation are (Becker et al. 2008):
-
Septa
-
Thin membrane
-
Soft tissue adhesion
-
Previous entrance into the sinus
-
Cyst/sinus pathology
-
Operator error
-
Overfilling with the graft material
8.2.1.4 Septa
The anatomy of the maxillary sinus cavity is variable. On the internal walls, we often observe a bone crest in relation to dental roots, acute angles, or especially septa. These irregularities are considered to be a real challenge during sinus grafting. The thorough preoperative examination of anatomical structures is always vital to prevent intraoperative or postoperative sinus complications. Antral septa were first analyzed and studied by the anatomist Arthur S. Underwood in 1910. Considered insignificant by clinicians for decades, they have gained importance since the beginnings of sinus floor grafting. Krennmair et al. (1999) classified septa into primary and secondary. The primary septa arise from the development of the maxilla and tooth eruption and are congenital, whereas the secondary septa are said to arise from the irregular pneumatization of the sinus floor following tooth loss and are acquired. Secondary bony septa can be considered residues between two zones of different resorption rate. Therefore, it can be said that the septa above the teeth are primary and the septa above an edentulous ridge are primary or secondary.
Septa prevalence is significantly higher in edentulous ridges compared with dentate ridges (Pommer et al. 2012). 28.4 % of sinuses contain at least one septum. No gender difference could be observed. The most frequent location (54.6 %) of septa is apical to first or second maxillary molar regions. It is very rare (0.3 %) to have a complete septum that divide completely the sinus into two separate cavities. Most of septa are incomplete and their mean height is 7.5 mm.
For a clinical purpose, it is extremely important to explore the orientation of the septum in order to decide how it will be managed during sinus floor grafting. Septa could be transverse (buccopalatal) in 87.6 %, sagittal (mesiodistal) in 11.1 %, or horizontal (parallel to the sinus floor) in 1.3 % (Fig. 8.4).


Fig. 8.4
3D reconstruction of a CT scan. Upper view of the two maxillary sinuses. Presence of two transverse (buccopalatal) septa in the left sinus and a sagittal septum in the right sinus
The use of 2D radiography for sinus examination and septa diagnosis prior to sinus floor augmentation is insufficient and give incorrect interpretations. Sagittal septa are not diagnosable on panoramic radiographs. The position, inclination, and height of the transverse septa are inaccurate on panoramic radiographs (Fig. 8.5). In order to have a complete knowledge of the anatomy of the sinus and to reduce complications related to septa, 3D radiography must be done (Fig. 8.4). The precise study of the coronal and Panorex reconstructed images allows the operator to conduct correctly the grafting procedure.


Fig. 8.5
Same patient of Fig. 8.4. On the panoramic radiograph, the sagittal septum in the right sinus cannot be seen and the buccopalatal septa in the left sinus are visible
Once the septa presence and configuration are well underlined, the surgical access strategy can be adopted. In presence of a transverse septum, the buccal window design is modified: two windows can be made (Fig. 8.6), one anterior and one posterior to the septum, and the membrane elevated till the tip of the septum but not lifted among its cranial part. If the septum is low, one W-shaped window can be made, and the membrane must be elevated from the cranial part of the septum. When septa are present, it is advised not to invert the buccal bone plate. Luxation of the window into the sinus and lifting of the membrane can tear the membrane stuck between the different bone borders. Cutting the septa with a chisel or a piezoelectric device and removing it with forceps can be done in order to eliminate this obstacle, but during this manipulation, a membrane perforation is very likely.


Fig. 8.6
In the presence of a septum, two lateral windows could be necessary
If the septum is high and sagittal, grafting only the lateral portion of the sinus cavity (laterally to the septum), as if the sinus anatomy is internally narrow, will be the safer therapeutic approach, and the implants will have to be placed more buccally. In case of short sagittal septum, a large window will allow access and membrane elevation to both parts, lateral and medial part of the sinus. It is very delicate to overpass the cranial part of the septa.
Some septa might be too difficult to manage during sinus floor augmentation, so we must take into consideration to change implant positions, avoiding some sites and therefore avoiding the sinus grafting on these sites (Figs. 8.7 and 8.8). In other cases grafting is aborted due to septa positions, so alternatives for sinus floor augmentation are chosen.
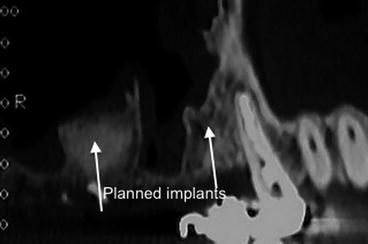
Fig. 8.7
Presence of a high septum
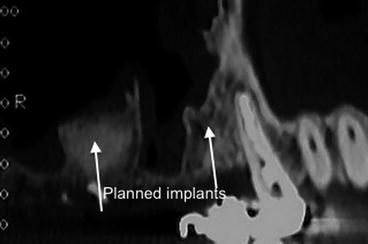
Fig. 8.8
The sinus was grafted distally to the septum and the implants will be placed in this grafted site (first molar) and the first premolar site. The two implants support a three-unit fixed prosthesis.
The membrane perforation risk is higher when antral septa exist because of the technical difficulty to overpass the cranial border of the septa and especially because the Schneiderian membrane is always thinner over the septa. In fact Binali et al. (2013) found a negative relationship between the membrane thickness and the presence of septa.
Explore the orientation and morphology of the septum on 3D radiography in order to know how to manage it. Two windows or W-shaped window allows access to sinus when the septum is high and transverse. Graft only the lateral portion of the sinus cavity when the septum is high and sagittal. Schneiderian membrane is always thinner over the septa.
8.2.1.5 Membrane Thickness
Lacerations are most likely to occur if the sinus membrane is thin (Van der Bergh et al. 2000). The incidence of perforation is greater when the thickness is less than 1.5 mm. Preoperative membrane thickness evaluation through clinical and radiological evaluation is possible (Figs. 8.9 and 8.10). Authors have found positive correlation between periodontal phenotype and sinus mucosal thickness. Subjects with thick gingival architecture are likely to have a thick (>1.26 mm) sinus mucosa. Gingival thickness seems to be a reliable parameter to predict sinus membrane thickness.
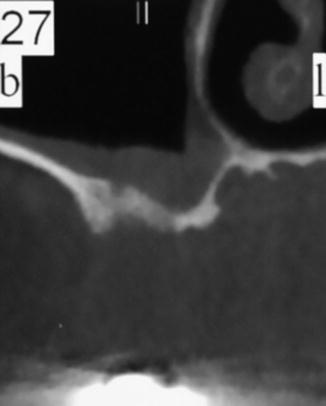
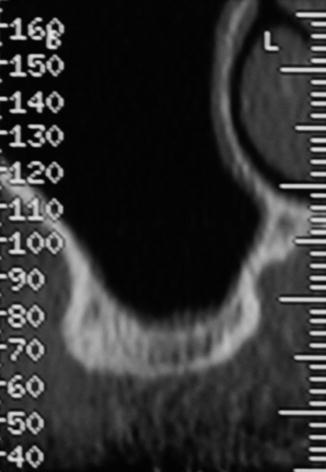
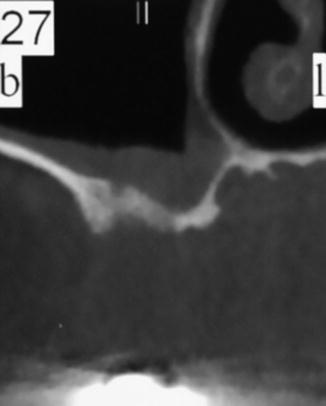
Fig. 8.9
Radiographic view of a thick Schneiderian mucosa lining the sinus floor
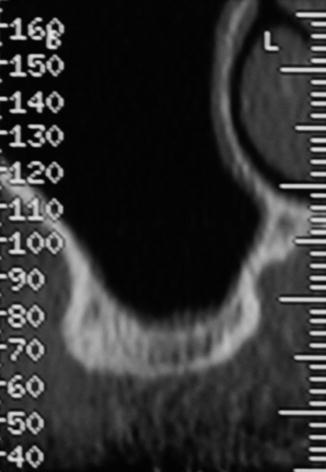
Fig. 8.10
Radiographic view of a thin sinus mucosa
Variations in the thickness of the Schneiderian membrane are due to the connective tissue layer. The epithelial lining contains two cell layers and is uniformly thick. Studies have found that thickness was higher in male than in female patients and that only slight differences were assessed intraindividually (Havas et al. 1988).
Sinuses that already received a surgical entrance might have a membrane that is fused with the inner portion of the buccal flap (Figs. 8.10, 8.11, 8.12, 8.13, 8.14, and 8.15). The membrane can also clinically be hardened and thickened, with some portions containing residual graft particles (Fig. 8.16). Removal of the incorporated graft is almost impossible because the membrane and the residual graft had fused together. The sinus membrane must be separated from the inner portion of the flap by sharp dissection with the blade to the detriment of the buccal mucosa. The stiffened sinus membrane is then carefully elevated. Manipulation of the mucosa in these cases seems easier.
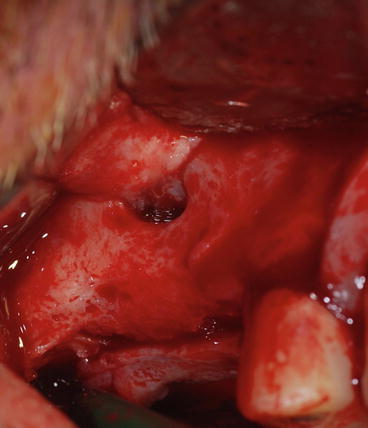
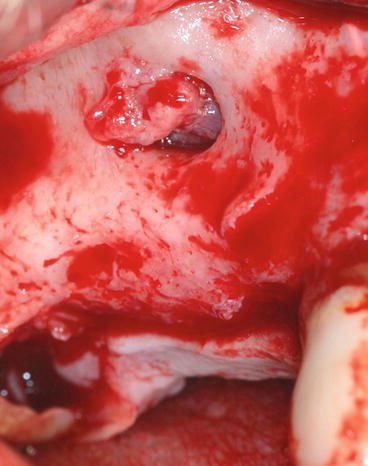

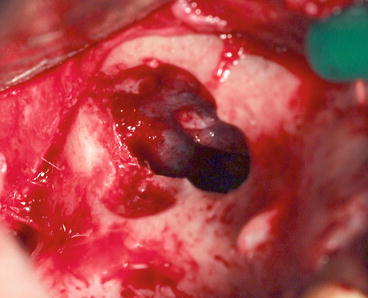
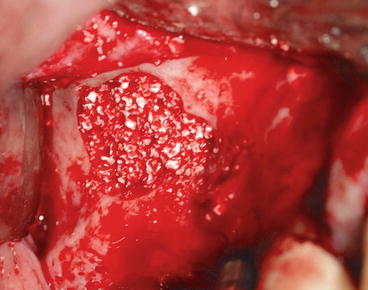
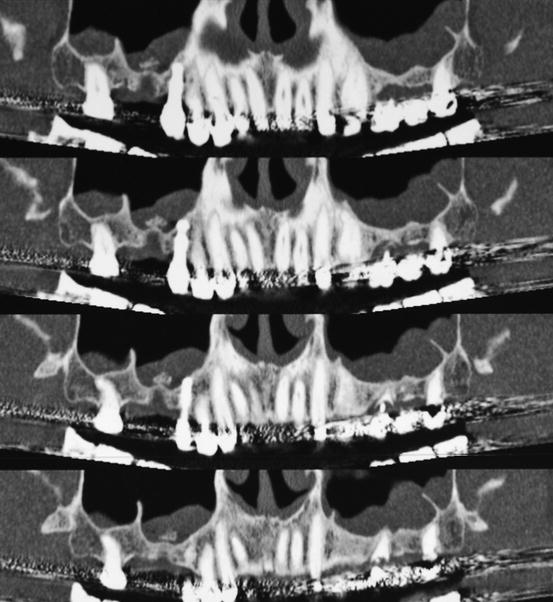
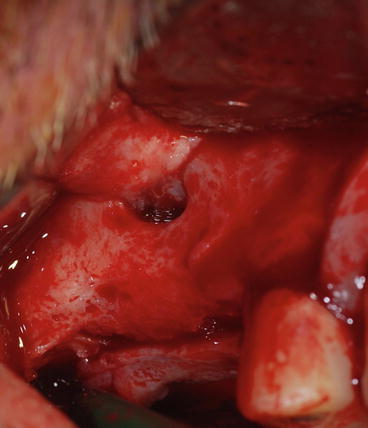
Fig. 8.11
The sinus and buccal mucosas are fused secondary to a gap in the maxillary bone. The origin of this gap is a previous periapical infection
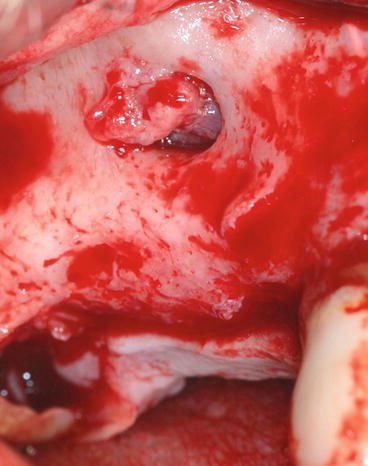
Fig. 8.12
Separation of the fusion with a blade to the detriment of the buccal mucosa. Care is taken not to cut the sinus membrane

Fig. 8.13
Osteotomy of the lateral wall starts from the maxillary bone gap
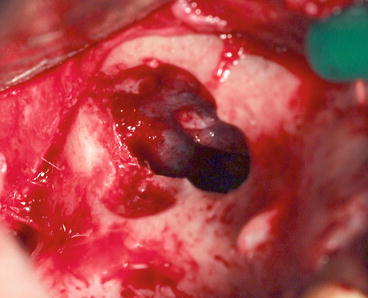
Fig. 8.14
After removal of the lateral window, the elevation of the stiffened sinus mucosa is completed
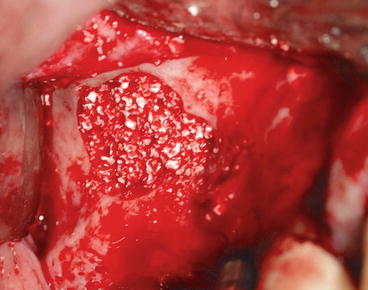
Fig. 8.15
Filling of the sinus floor with synthetic hydroxyapatite (Ingenios Zimmer Dental Inc., Carlsbad, USA)
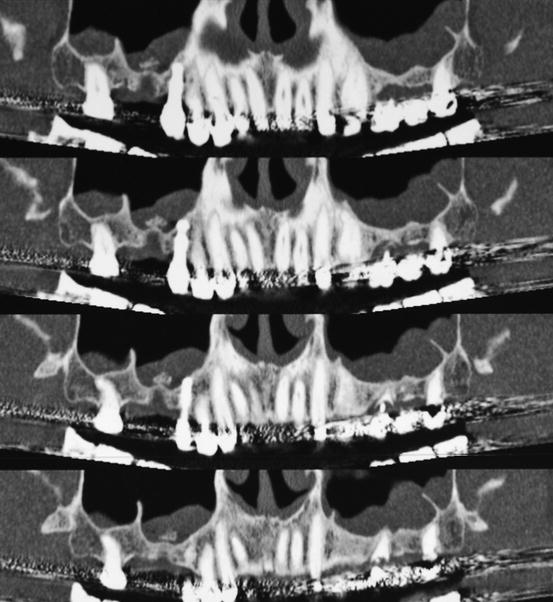
Fig. 8.16
Biomaterial particles incorporated in the sinus membrane secondary to a failed grafting attempt
8.2.1.6 Perforations Management
Vlassis and Fugazzotto (1999) have classified perforations based on their size or on their location, and in 2003 they published a new classification based on the difficulty to repair. We will describe the most adapted ways to manage such complications.
When a perforation is detected, it is essential to evaluate the width of the bone window, and when necessary the outline of this window will be extended in order to reach intact membrane from where elevation can be initiated. The membrane surrounding the perforation is delicately dissected with a blunt instrument. This elevation must be started far from the perforation in an attempt to relieve the tension on the tissue of the perforated area.
In small perforations (<5 mm), the membrane will fold on itself during the elevation. After complete elevation, an absorbable collagen wound dressing (photo CollaTape, Zimmer Dental Inc., Carlsbad, USA) is applied on the antral mucosa as reinforcement. Its adhesive properties make it easy to handle and to apply on the perforated membrane (Figs. 8.17 and 8.20). A platelet-rich fibrin membrane can also be used in this same indication. Bone filling can then be continued. The use of a fibrin adhesive to seal a small perforation has been suggested by authors to be efficient (Choi et al. (2006)).


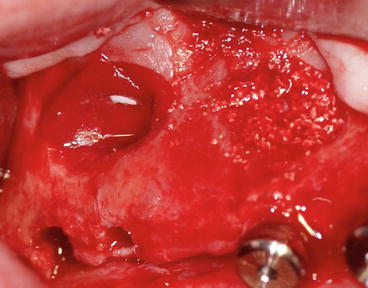


Fig. 8.17
A small perforation occurred during the osteotomy procedure

Fig. 8.18
CollaTape wound dressing (Zimmer Dental Inc., Carlsbad, USA)
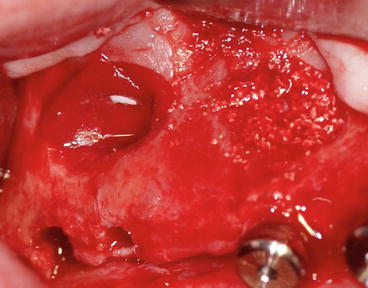
Fig. 8.19
The wound dressing covering the perforation after membrane elevation

Fig. 8.20
Filling of the sinus floor and simultaneous implant placement
In larger perforations (5–10 mm), if after elevation of the membrane the perforation is still apparent, we can place an absorbable collagen membrane underneath the elevated sinus membrane to create a superior barrier to confine the grafts.
Suturing the perforation with a 6/0 Vicryl (Ethicon, Norderstedt, Germany) is a very difficult manipulation because of the inaccessibility and the mechanical proprieties of the mucosa lining that has tendency to dilaceration and subsequently to enlarge or create new perforations (Fig. 8.21).
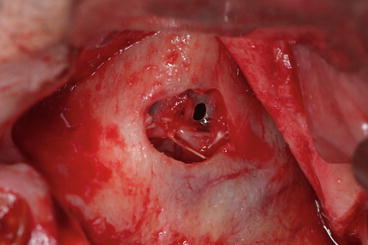
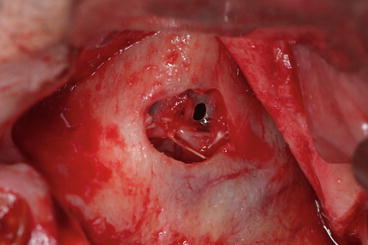
Fig. 8.21
Attempt to suture the perforated membrane
Complete Tear. In the event of a large dilaceration, again the use of a large resorbable collagen membrane allows proper reparation.
This membrane will be placed on the medial wall of the sinus and then folded on the borders of the bone window from the upper and lower part as a new roof and floor. This pouch surrounds and isolates the bone graft (Proussaefs and Lozada 2003).
It is sometimes necessary to stabilize this membrane on the surrounding bone using fixing pins or resorbable sutures. However, this isolation using the pouch might have an adverse effect on the neovascularization and the remodeling of the graft (Figs. 8.22, 8.23, 8.24, and 8.25).
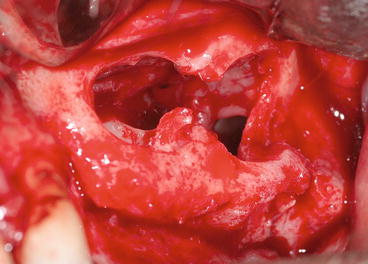
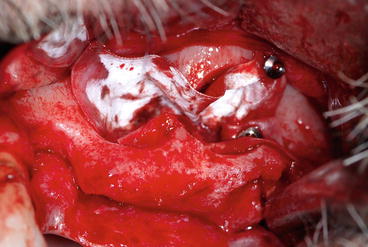


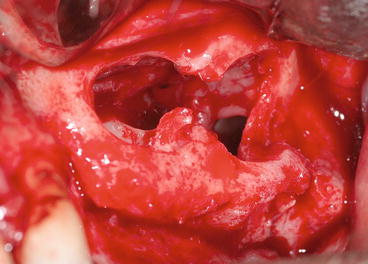
Fig. 8.22
The same patient in Fig. 8.4. During membrane elevation between the two sagittal septa, a large dilaceration of the membrane occurred
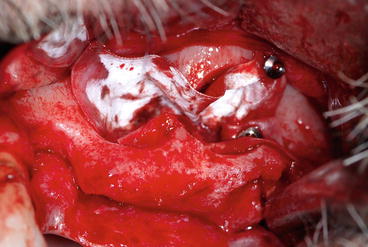
Fig. 8.23
A large resorbable collagen membrane (Copios Pericardium 30 × 40 mm, Zimmer Dental Inc., Carlsbad, USA) is placed on the medial wall of the sinus and then folded on the borders and stabilized with fixing pins

Fig. 8.24
Biomaterial filling in the pouch

Fig. 8.25
Postoperative panoramic radiography showing the graft left maxillary sinus
Otherwise a bone block harvested from the symphysis or the retromolar area can be placed and fixated as a roof for the graft. The major inconvenience is the additional time and surgical site that were not planned and unexpected by the patient. A pedicled buccal fat pad can also be used to restore the defect. It can be harvested quickly but meticulously from the infratemporal fossa through an incision of the periosteum. After blunt dissection of the buccinator muscle with a Metzenbaum scissors, the buccal fat pad is drawn out with Kelly forceps and placed against the membrane. It will isolate the sinus cavity from the graft material packed underneath it.
For all sinus grafting candidates and especially for those who had a perforation repaired, it is extremely important to emphasize on the postoperative care: not to blow their noses and to sneeze opening the mouth for 2 weeks after surgery (no scuba diving, no flying).
At last the interruption of the procedure is recommended when the repair of a perforation seems difficult. Some authors (Schwartz-Arad et al. 2004; Pikos 2008; Lee et al. 2013) have postulated that there is no need to abort a sinus augmentation procedure in the event of a complete tear and that properly repaired sinus membrane perforation did not cause subsequent implant failure. In some cases, it is much easier and safer to abort grafting and program reentry at least six weeks later, in order to obtain a healed membrane.
8.2.1.7 Outcome
Considering its prevalence (20 %), perforation is a frequent complication; it is all the more important to evaluate the outcome of sinus grafting after a perforation.
Membrane perforation can be associated with the appearance of:
-
Graft dislodgement into the sinus
-
Obstruction of the osteomeatal apparatus
-
Disruption of the normal sinus physiology
-
Bacterial invasion
-
Secondary acute or chronic infection
-
Graft loss and/or failure
-
Disturbance of the vascularization of the membrane and consequently of the neovascularization of the graft mass
Disrupted mucociliary apparatus function and loss of the biologic barrier owing to perforation of the membrane can increase sinus bacteria invasion and infection. The first step in managing infection is drainage and switching antibiotic regimens (to clindamycin or pristinamycin). If the infection persists, surgical debridement of infected bone and granulation tissue has to be performed.
The clinical significance of sinus membrane perforation is controversial. Multiple studies have shown an association between membrane perforation and acute sinusitis or graft infection or failure (Proussaefs et al. 2004; Schwartz-Arad et al. 2004; Jensen et al. 1998, Khoury et al. 1999), whereas others have shown no association between membrane integrity and infection or graft failure (Bornstein et al. 2008; Raghoebar et al. 2001; Becker et al. 2008; Jensen 1997). Repaired perforations have often an uneventful healing. Complete graft removal and drainage are seldom necessary because of acute postoperative infection. Due to infection a partial graft loss can be observed, but the remaining bone can be sufficient for implant placement. Patients can also report graft particle evacuation from the nasal fossae.
Data (Proussaefs and Lozada 2003; Khoury 1999) in the literature showed that in perforated membrane cases, the implant failure was significantly higher and vital bone formation lower. In contrast in other studies, there was no association between membrane perforations and implant survival rate (Schwartz-Arad et al. 2004; Fugazzotto and Vlassis 2003; Nkenke et al. 2002; Shlomi et al. 2004). However, extreme care should be taken when managing perforations, and close follow-up should be established in order to make an early diagnosis. When reparation seems difficult or impossible, the procedure should be abandoned in order to avoid serious postoperative complications.
Repaired perforations have often an uneventful healing. Extreme care is taken when managing perforations and close follow-up is primordial. When reparation is impossible, the procedure is aborted. Reentry is planned after 3 months.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


