Subapical osteotomy of the entire mandible is an operation with specific and limited indications, but when these indications are present, the operation is invaluable. With attention to details, the operation can be conducted safely with excellent healing, few complications, and favorable outcomes. The keys to the safe conduct of the operation are (1) preserving the lingual tissues, including all musculature, as the vascular pedicle, and (2) providing complete exposure and protection of the neurovascular bundle as it courses through the mandible from the third molar region to the mental foramen.
The mandibular subapical osteotomy was originally described by Hullihan and is the oldest documented mandibular osteotomy; it was first performed more than a century and a half ago. Hofer’s and Köle’s publications contributed to the popularity of this procedure. Procedures such as Hullihan’s were confined to the anterior mandible. Osteotomy of the entire mandibular dentoalveolus was first described in 1974 by MacIntosh. Subsequently, Booth and Buckly contributed to this topic. Relative to other facial osteotomies, a paucity of literature is available on this procedure, most likely because its indications are limited.
When the procedure was originally described, the major indication was open bite recalcitrant to orthodontic treatment. Class II malocclusion with excessive chin projection and exaggerated labiomental fold is another indication. The goals of the operation are to correct the malocclusion, maintain the chin projection, and improve support for the lower lip and labiomental fold. The primary esthetic benefit of the operation is seen as altered position of the lip and improved harmony of the lip with the chin.
Today, it is recognized that the vertical dimension of the face is an important determinant of chin projection. Long-faced patients tend to demonstrate retrogenia. Short-faced patients tend to exhibit progenia (macrogenia). Therefore, when the indications for this operation are evaluated, the ideal facial vertical height must be determined, and planning commences from that position. When face height increases as a result of this operation, the pterygomasseteric musculature is stretched as the mandibular angles rotate inferiorly and posteriorly. Accurate determination of the free way space prior to surgery assists in determining the amount of vertical opening that is tolerable. This operation may be used to reduce face height; accommodation and stability are more favorable than when face height is increased. A critical step in this procedure is to control the face height so that the desired face height is established.
INDICATIONS
The primary esthetic indication for this operation is imbalance between the chin and lower lip accompanied by class II or class II malocclusion. Under normal circumstances, the lower lip should be on the same parallel as the chin when viewed in profile.
The position of the lower lip is dependent on support from the mandibular incisors and the dental alveolus, as well as on the composition and distribution of the skin, mucosa, fat, muscle, and salivary glands of the lip. When the profile is considered, the lower lip and chin should be balanced, and the labiomental fold should separate the two with a gentle concavity. Cephalometric analysis aids in establishing the exact measurement necessary to achieve harmony between these facial units. The holdaway ratio in most Caucasians is 1 : 1, or at most 2 : 1 (in smaller females). This line is constructed by extending the N-B line to the inferior border of the mandible and by measuring the distance from this line to the tip of the mandibular incisor and comparing it with the measurement from the same line to the pogonium. In African and Asian populations, this measurement increases ( Figure 6-1 ).
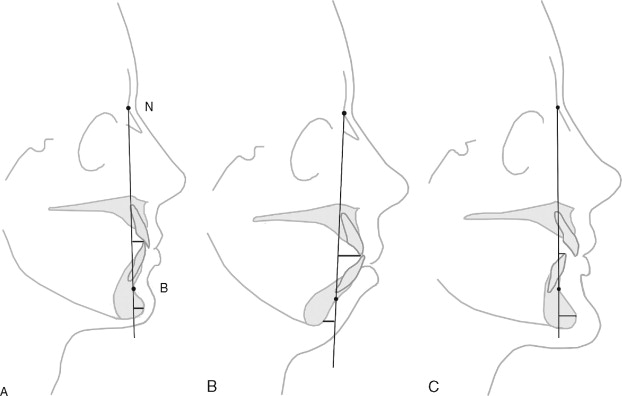
When class II malocclusion is corrected and the dentoalveolus is advanced, the retruded lower lip and labiomental fold respond favorably. When class III malocclusion is corrected with this operation, the dentoalveolus is positioned posteriorly, and the lower lip and the labiomental fold follow. In both situations, improving lip-to-chin harmony is the goal.
Other indications for this procedure include vertical and transverse dental arch discrepancies. When transverse arch discrepancies or vertical discrepancies exist, segmenting the mandibular arch simultaneously is also possible. The success of this depends on maintaining healthy vascular pedicles to the segments and safely conducting the interdental osteotomy. Orthodontic preparation of the interdental osteotomy site is important. Creating adequate space between the roots (2 to 3 mm) helps to minimize the risks of developing endodontic or periodontal defects at the site.
TECHNIQUE
All mandibular third molars should be removed at least 3 months in advance of this operation. A panorex is taken to identify the roots of the mandibular teeth and their relationship to the neurovascular canal. Almost always, several millimeters can be measured between the roots and the superior border of the neurovascular canal. The panorex is also helpful in identifying the height of the mandible that remains at the inferior border after the proposed osteotomy has been conducted. Ideally, 1 cm of inferior border should remain intact at the completion of surgery. This ensures the integrity of the mandible and reduces the risk of fracture.
The buccal tissues of the entire mandibular alveolus and the lower lip are injected with a diluted vasoconstrictor (1 : 100,000 epinephrine). An incision is made in the loose mucosa to the depth of the periosteum over the external oblique ridge of the mandibular ramus in the retromolar region (similar to sagittal osteotomy). The incision continues anteriorly toward the mental foramen approximately 5 mm inferior to the junction of the fixed gingiva and the mucosa.
At the region of the first premolar, the incision is directed into the lip so that the midline is well beyond the mucobuccal fold (similar to a genioplasty incision). With this incision, the mentalis is transected rather than being dissected from its attachment to the mandible, as when a sulcular incision is made. Suturing the muscle during closure is critical; this reduces the risks of chin ptosis and wound dehiscence. Wide buccal soft tissue coverage remains over the entire anterior region, and the fixed gingival tissues remain in place around the teeth. A similar incision on the opposite side connects at the midline. A full-thickness mucoperiosteal flap then is elevated to the inferior border of the mandible. At the mental foramen, the nerve is identified, dissected around the entire circumference of the foramen, and protected. Anteriorly, the dissection is stepped through the mentalis muscle to expose the entire symphysis. Care must be taken to avoid violating the skin during this part of the dissection. When the entire buccal dissection has been completed, the inferior border of the mandible, the mental foramina, the symphysis, and the bodies of the mandible are exposed to the angle.
Recording the vertical dimension from a landmark below the proposed subapical osteotomy site at the symphysis to a reliable maxillary or mandibular landmark is critical and should be done initially ( Figure 6-2 ). This assists in determining that the preplanned height of the face is achieved, and that the chin will not be rotated out of position.
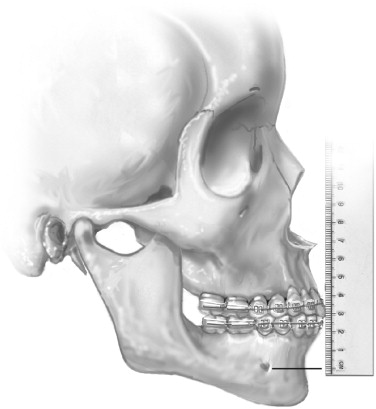
Channel retractors are placed under the inferior border of the mandible to expose the buccal cortex from the mental region to the retromolar region. Panoramic radiography helps the clinician to identify the superior-inferior location of the neurovascular bundle as it courses through the mandible.
The inferior alveolar nerve enters the mandibular foramen on the medial surface below the sigmoid notch. It courses laterally as it descends the ramus to the third molar region, where it lies just below the buccal cortex. At this point, it proceeds anteriorly and medially in the cancellous bone. When it reaches the mental foramen, it exits the foramen in a superior and posterior direction. Before exiting the foramen, the incisal nerve branches off and continues anteriorly to the symphysis. The buccal-lingual anatomy of the nerve is relatively constant, and its most buccal position is in the third molar region. Its anterior course is more lingual and has been described in detail by Sicher. Cone beam computed tomography (CT) scans can be used to identify the exact location of the nerve, but the necessity of using CT when this operation is performed is questionable. The major portion of the nerve exits the mental foramen as the mental nerve, which supplies innervation to the lower lip and chin area. From the retromolar region to the mental foramen, the nerve is dissected; it is protected throughout this operation.
Blood is supplies to the mobilized segment primarily from the lingual musculature and soft tissues that remain pedicled to the segment. The inferior alveolar neurovascular bundle contributes to the vascularity of the mobilized segment, but its integrity is not critical for wound healing. If it is violated during the procedure, the operation should not be aborted. Hemostasis should be attained, and this violation should have little or no consequences on healing as long as the lingual pedicle remains attached.
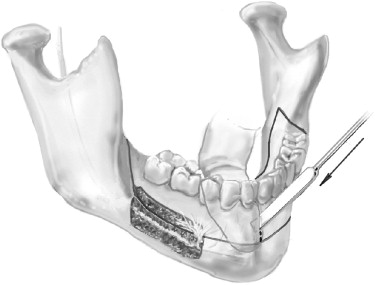
A small fissure bur is used to perform a buccal cortex osteotomy approximately 1 cm inferior to the alveolar crest from the retromolar region anteriorly to the mental foramen. This should occur above the neurovascular canal. A second buccal cortex osteotomy is made below the level of the neurovascular bundle parallel to the first. The two osteotomies then are joined anteriorly and posteriorly by two perpendicular osteotomies—one in the retromolar region and the second just anterior to the mental foramen. It is important for these osteotomies to extend through the full cortex and enter the cancellous bone.
The superior osteotomy is beveled to allow insertion of a curved osteotome ( Figure 6-3 ). Through malleting of the osteotome in multiple areas, the buccal cortex is fractured and removed, exposing the cancellous bone. The cancellous bone is scraped away to expose the neurovascular bundle. The neurovascular bundle is identified and is left in the canal. Care must be taken around the mental foramen to free it and to preserve the nerve. The neurovascular bundle remains undisturbed in its position, as does the incisal branch. A reciprocal saw then is used to make a cut above the neurovascular bundle and below the roots through the entire thickness of the lingual cortex ( Figure 6-4 ). Anterior to the foramen, the cut should be made 5 mm below the cuspid root and through both the buccal and lingual cortices. This is done bilaterally, and the osteotomies are joined in the midline below the genial tubercle. The incisal branch of the inferior alveolar nerve occasionally is observed and even transected without significant consequences.
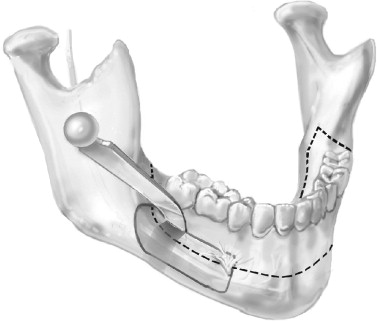

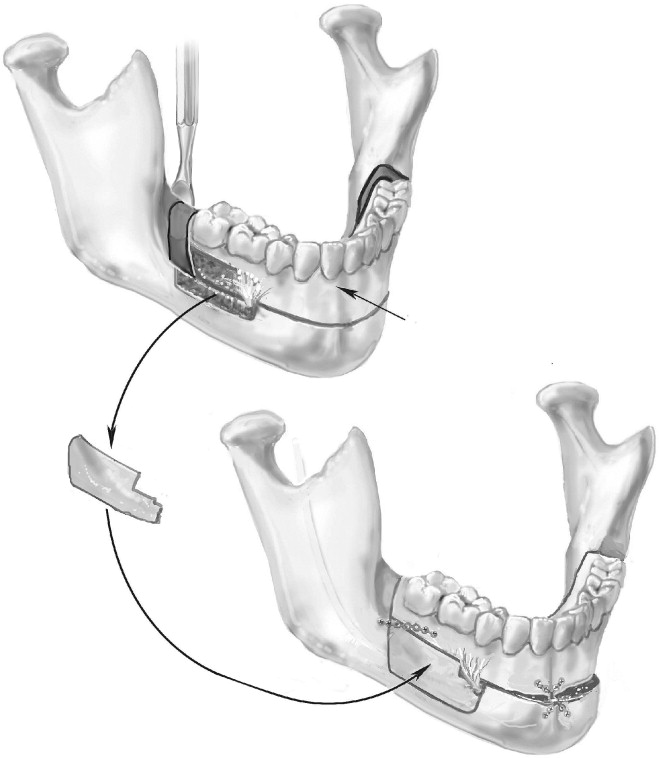
The retromolar vertical osteotomy is performed next. After the gingival tissues are dissected superiorly over the external oblique ridge to the lingual cortex, a reciprocal saw is used to section the bone from the superior alveolus inferiorly to join the subapical osteotomy. The retromolar osteotomy should be performed obliquely and just posterior to the terminal molar. This facilitates setback and provides good bone contact when an advancement is performed. If the segment is to be moved posteriorly, a retromolar ostectomy is required. When an ostectomy is performed in the retromolar region, subperiosteal dissection of tissues on the lingual side should be performed to prevent lingual nerve injury. Care must be taken to protect the neurovascular bundle, especially when the two osteotomies are joined ( Figure 6-5 ). A small osteotome can be used judiciously to complete the bone cut. A large wedging osteotome or bone spreaders then are used to mobilize the entire dentoalveolar segment anteriorly. Force should not be required and should not be applied to prevent untoward fracture, especially of the inferior border of the mandible.
Once mobilized, the segments should be advanced or retropositioned as desired. The occlusal splint and intermaxillary fixation should be applied. Reference points from the maxilla or mandible to the mandibular inferior border are checked to determine the correct vertical dimension. Bone should be relieved at areas of premature contact until the correct height has been achieved. It is critically important that the desired vertical height be achieved if the desired result is to be achieved.
When the mobilized dentoalveolus is to be segmented, the correct interdental site is dissected subperiosteally on the buccal side to the crest of the alveolus. Periapical or panorex radiographs are used to facilitate the process of locating the roots. A small fissure bur is used to score the buccal cortex between the roots. Then, a thin osteotome is malleted through to the lingual. A finger placed intraorally on the lingual surface aids in protecting the lingual soft tissues, which should remain intact ( Figure 6-6 ). An occlusal splint is used to establish the desired positions of the segment. When multiple segments are mobilized, they are wired into the occlusal splint so their correct position can be established. Bone plates and screws then should be used to secure the segments. Usually, one plate positioned anteriorly and one placed on either side posteriorly are all that is required ( Figure 6-7 ). If multiple segments have been mobilized, appropriate stabilization may require additional plates and screws.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses