Fig. 2.1
(a) Scheme of IBBC at immediately after surgery and 2–3 weeks after surgery. (b) Animal experiment of IBBC cross section of femoral condyle of the rabbit performed with IBBC. (c) Animal experiment of IBBC 1 week after surgery. (d) Animal experiment of IBBC 2 weeks after surgery. (e) Animal experiment of IBBC 8 months after surgery. (f) Animal experiment of IBBC 3 years after surgery. (g) Higher magnification of Figure (f)
2.2.2 Experimental Studies
2.2.2.1 Histological Studies
Holes with a diameter of 6 and 10 mm in depth were made in both femoral condyles of mature rabbits, and HA granules of 300–500 μm in diameter were smeared in less than two layers over the bone surface of the hole, and the hole was filled with bone cement (Fig. 2.1b). In groups of three, rabbits were sacrificed at 2, 3, 4, 6, 12, and 24 weeks and at 3 years after implantation. Non-decalcified hard tissue specimens were prepared and examined by optical microscopy, scanning electron microscopy (SEM), and backscattered electron imaging.
One week after surgery, new bone began entering the first to second layer and adhering to the HA granules (Fig. 2.1c). At 2–3 weeks after surgery, new bone had entered a majority of the spaces in the second layer (Fig. 2.1d). After 6 weeks or more, all spaces were filled with new bone, thus forming a unified body, as illustrated in Fig. 2.1e at 8 months postsurgery. Three years after surgery (Fig. 2.1f), bone ingrowth into the spaces of HA granules was the same as that seen at 6 weeks and 8 months (Fig. 2.1e). The bone was retained only in the place where HA granules were smeared. There was no bony tissue in other place due to aging (Fig. 2.1f, g).
2.2.2.2 Bonding Strength of the HA Granule Layer to Bone
IBBC was tested on mature rabbits. Holes with a 6 mm diameter and a depth of 10 mm were made in both femoral condyles. The rabbits were sacrificed in groups of three at 2, 4, 6, 12, and 24 weeks after implantation, and a push-out test was performed. HA coating applied to a smooth titanium surface was used as a control.
A relatively strong initial fixation was obtained immediately after implantation using the IBBC technique. Two weeks after implantation, the bonding strength of IBBC was higher than that of the HA coating, but at 6 weeks after implantation, the bonding strength of IBBC became similar to that of HA coating. The fractures resulting from the push-out test occurred in the HA granule layer from 2 to 6 weeks after implantation and occurred in both the HA granule layer and the surrounding bone layer after 12 weeks. These results indicated that the strength of the HA granule layer gradually increased after surgery and reached almost the same level as the bone around the HA granule layer after 12 weeks. In these experiments, the bonding strength of bone cement to bone by interposing HA granules was found to be adequate (Fig. 2.2).
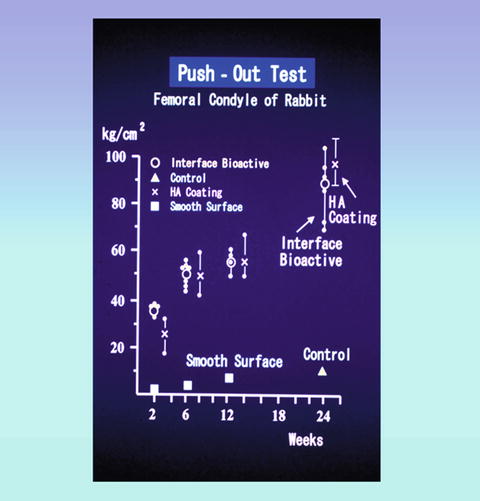
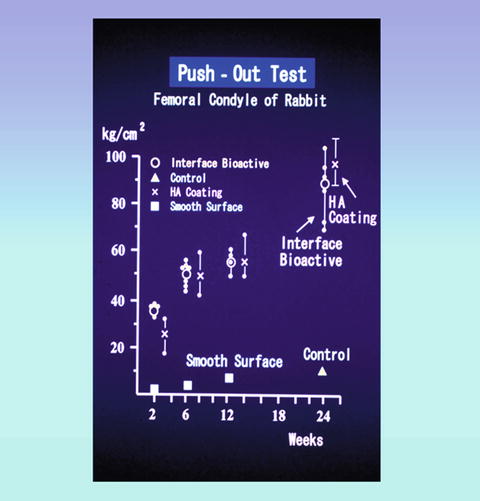
Fig. 2.2
Push-out test: Comparison of adhesive strength to the bone of IBBC and HA coating
Stress shielding was not found in subsequent clinical trials. When cement fixation using PMMA bone cement was performed, excellent initial fixation can be obtained. However, after a period of time, a connective tissue membrane may form between the bone and bone cement, particularly in the acetabulum. This may lead to component loosening.
When cementless fixation with a HA-coated component was performed, micromotion of the component may occur if the initial fixation is insufficient. Therefore, we are confident that IBBC combines the fixation advantages of both conventional PMMA bone cement and HA coating in early stage.
2.2.3 Clinical Studies
2.2.3.1 Surgical Technique
A cobalt-chromium alloy femoral component (KC, Kyocera Co. Ltd. Kyoto, Japan) with a 28 mm alumina head was used in combination with an all-polyethylene acetabular component. All operations were performed by the senior author (H.O.) through an anterolateral approach in supine position.
HA granules were manufactured by sintering at 1,200 °C in Sumitomo Osaka Cement Co. Ltd., Chiba, Japan. Porous HA granules with 300–500 μm in diameter were used. For acetabular side, several small anchor holes for initial fixation were made and intensive care was taken for sufficient hemostasis by means of hypotensive anesthesia (approximately 90 mmHg), temporal compress at the bleeding points with bone paste obtained by acetabular reaming, and a rinse with hydrogen peroxide followed by compressive gauze packing. HA granules (2–3 g) were smeared on the bone surface just before cementing of the acetabular component. CMW-I bone cement (C.M.W. Laboratories Ltd., Blackpool, UK) was used in all cases. Porous HA granules could easily adhere on the wet bone surface (Fig. 2.3a, b). For the femoral side, hemostasis was achieved in the same manner and HA granules (2–3 g) were smeared on the inner surface of the prepared femoral canal using a half-tube silicone rubber (3–5 cm in length) clamped by a long-straight Kocher’s hemostatic clamp (Fig. 2.3c, d). The femoral component was fixed with second-generation cementing technique using an intramedullary bone plug and cement gun. These procedures resulted in the presence of less than 2–3 layers of HA granules in most of the bone-bone cement interface, while bone cement directly contacted with bone without interposition in some part. The same cementing technique was applied for the conventional THA procedures except for using HA granules.
Fig. 2.3
(a) Smearing procedures of HA granules on the acetabulum. (b) After smearing of HA granules on the acetabulum. (c) Smearing procedures of HA granules on the inner surface of the femur. (d) Experimental studies of smearing of HA granules on the inner surface of the femur. (d–[a]) Homemade instrument to smear HA granules. (d–[b]) Smearing HA granules by using the instrument. (d–[c]) Inner surface of the femur before smearing HA granules. (d–[d]) Inner surface of the femur after smearing HA granules
The key points of surgical procedures were as follows:
1.
Hemostasis immediately before cementing is very important.
2.
Several small anchoring holes for initial fixation are necessary.
3.
HA impregnated by antibiotics as a drug delivery system is very effective for prevention of infection.
2.2.3.2 Changes of IBBC Technique
In the first generation, from 1982 to 1988, HA granule size of 0.3–0.5 mm in diameter was used, and several small anchoring holes of 3 mm in diameter were made. In the second generation, from 1989 to 1997, HA granules of 0.1–0.3 mm were used because a smaller size of HA granules adhered more easily to the interface. However, as a smaller size of HA was covered easily by blood in the bleeding area, the connection of the bone cement with HA was prevented. As the result, a space appeared between bone cement and HA.
Consequently, in the third generation, from 1998 to 2001, HA granules of 0.3–0.5 mm were used again and several numbers of anchoring holes of 6 mm in diameter were made for stronger initial fixation. In the fourth generation, since 2001, HA granules of 0.3–0.5 mm with 1.0–1.5 mm were used and several layers of anchoring holes more than 6 mm in diameter were made, thereby enhancing safety even if IBBC was performed in the bleeding area.
2.2.3.3 Long-Term Clinical Results for 24–31 Years
Long-term clinical cases were classified into three groups. In group (1), 1982–1985, IBBC was performed in 12 joints as trials and conventional bone cement (non-IBBC) in 79 joints. In group (2), 1985–1986, IBBC was performed on one hip joint and non-IBBC was performed on the other hip joint in the same patient. These were performed in 25 patients. In group (3), 1986–1989, IBBC was performed in all cases in 285 joints (212 patients) (Fig. 2.4).
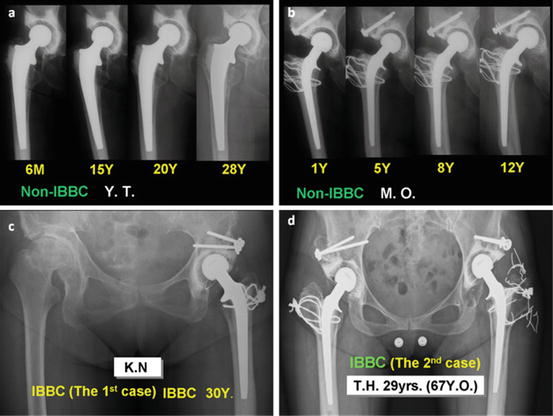
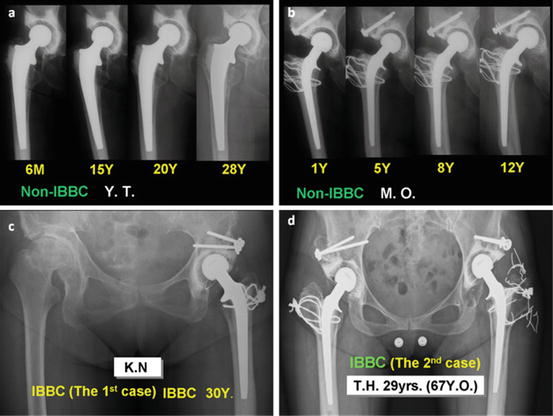
Fig. 2.4
(a) Clinical course of X-ray figure after THA with conventional bone cement (non-IBBC). Osteolysis was seen in the femur 15 years after THA. Osteolysis and radiolucent line were seen in the acetabulum and the femur 20 years after THA, and they progressed 28 years after THA. (b) Clinical course of X-ray figure after THA with non-IBBC radiolucent line was seen in the acetabulum 5 years after THA. Stem loosening was seen 8 years after THA and it progressed and radiolucent line progressed in the acetabulum and stem loosening progressed 12 years after THA. (c) This is the first case of THA with IBBC. Thirty years after THA, polyethylene socket wear increased in high degree. However, neither radiolucent line nor osteolysis was seen. (d) This is the second case of THA with IBBC in bilateral hips 29 years after THA. She has worked as a dancer for 28 years. Radiolucent line and osteolysis were seen in only small limited area
2.2.3.4 Group (2): (1985–1986, 25–26 Years After Surgery)
Group 2 has 16 patients with survival in both hips. In non-IBBC hips, the prostheses were loosened in five hips in the acetabulum and in two hips in the femur within 20 years. The radiolucent line and the osteolysis increased gradually and their appearance time was indefinite. Seven hips were revised within 15–20 years.
In IBBC hips, the radiolucent line and the osteolysis appeared in only small limited areas and did no progress. The rich new bone formation was maintained at the interface of bone and bone cement by interposing HA granules (Fig. 2.5a–c). In the survival cases of hips with both IBBC and non-IBBC, wide radiolucent lines and osteolysis and loosening were seen in non-IBBC cases; however, only few radiolucent lines and osteolysis were seen in the small limited areas in IBBC hip replacements (Fig. 2.5d, e).
Fig. 2.5
(a) One year after THA with non-IBBC in the left hip and 3 months after THA with IBBC in the right hip. (b) In the right hip with IBBC, neither radiolucent line nor osteolysis was seen 23 years after THA in spite of progress of polyethylene wear. In the left hip with non-IBBC, both radiolucent line and osteolysis progressed in both acetabulum and femur 24 years after THA. (c) In the right hip with IBBC, neither radiolucent line nor osteolysis was seen 23 years after THA. In the left hip with non-IBBC, 24 years after THA, both radiolucent line and osteolysis were seen in the acetabulum, and osteolysis and stem loosening were seen in the femur. (d) Comparative appearance rate of radiolucent line 25–26 years after THA with IBBC and non-IBBC performed in the same patient. (e) Comparative appearance rate of osteolysis 25–26 years after THA with IBBC and non-IBBC performed in the same patient
2.2.3.5 Group (3): (1986–1989, 22–25 Years After Surgery)
In this group, IBBC technique was used in all cases in 285 joints (212 patients). The radiolucent line and osteolysis appeared in only small limited areas and did no progress (Fig. 2.6a). Extensive new bone formation was seen at the interface of bone and bone cement by interposing HA granules (Fig. 2.6b, c). In groups 1–3, when IBBC was performed in the bleeding area, the spaces appeared between bone cement and HA several months after surgery on the X-ray figure (Fig. 2.6d). However, the spaces did no progress (Fig. 2.6e). When the space appeared in the large area, the partial separation of bone cement from HA at the interface of HA and bone cement occurred in two cases (Fig. 2.6f). HA incorporated with the bone at the interface (Fig. 2.6g). In non-IBBC cases with only conventional bone cement, when wear particles of polyethylene increased, phagocytosis occurred and osteolysis appeared on the radiograph.
From the long-term clinical results of IBBC, the rate of formation of space or voids between HA and bone cement was less than 2 %. They appeared at the limited areas in both the acetabulum and the femur for the first- and second-generation IBBC procedures. The spaces were not radiolucent lines. They appeared at a rather higher rate in the second generation than in the first generation because the HA granule size in the first generation was bigger than that in the second generation.
The appearance rate of osteolysis was extremely low, less than 1.5 %, appearing in few restricted areas. The separation between bone cement and HA occurred in the acetabulum in the second generation in two joints that is 0.8 %. There was no loosening between bone and bone cement. Since 2001, in order to prevent the occurrence of the spaces and the separation between bone cement and HA, several anchoring holes over 6 mm in diameter were made in the acetabulum and HA granules of 0.3–0.6 mm and 1.0–1.5 mm were smeared on the bone surface.
In the IBBC procedure, there was no loosening between bone and bone cement in groups 1, 2, and 3 for 27 years. However, in non-IBBC hip replacements, loosening occurred in over 80 % of cases, a high rate, for 31 years (Table 2.1).
2.2.4 Histological Studies on Retrieval Cases
2.2.4.1 Materials and Methods
In 14 patients, specimens containing a well-fixed bone-cement interface were retrieved during revision surgery. The diagnosis was degenerative osteoarthritis in ten hips and in one knee, rheumatoid arthritis (RA) in two, and osteonecrosis after radiation therapy for portio cancer in one. The causes of revision were dissociation of the metal-back socket from the bone cement in nine hips, aseptic loosening of the socket in one, and late infection in four.
Fig. 2.6
(a) Clinical results of THA with IBBC 22 to 25 years after THA. Appearance rate of radiolucent line and osteolysis was extremely low. Radiolucent line appeared between bone cement and HA, because the cementation was performed in the bleeding area. This line was not a radiolucent line but a space in correct. (b) THA with IBBC was performed in dysplastic acetabulum 24 years after THA. Neither radiolucent line nor osteolysis was seen in both acetabulum and femur. Rich new bone formation was seen on the hole around the bone cement. (c) THA with IBBC was performed in dysplastic acetabulum 24 years after THA. Wear of polyethylene socket highly increased; nevertheless, neither radiolucent line nor osteolysis was seen. (d) Scheme of the condition performed IBBC in the bleeding area. Spaces appeared between bone cement and HA several weeks after THA on the radiograph. It did no progress. (e) IBBC was performed in the bleeding area. A space appeared several weeks after THA. It did no progress. (f) Separation between bone cement and HA after THA with IBBC in the bleeding area and without sufficient anchor holes. (g) IBBC was performed in the bleeding area without sufficient anchor holes. Separation occurred between bone cement and HA 3 weeks after THA. However, fixation of bone to the bone cement was continued by interposing HA granules (IBBC) at the laterosuperior area
At the revision surgery, the specimens were carefully cut out using a surgical osteotome or oscillating bone saw to retrieve the bone-cement composites without breaking the bone-cement interface. In the acetabulum, six specimens were retrieved from the superior wall, which was considered to be the principal weight-bearing site, and ten specimens were retrieved from the inferomedial wall, which was considered to be the auxiliary weight-bearing site. Three specimens were retrieved from sites where the HA granules failed to be smeared. In the femur, two specimens were retrieved from the greater trochanter and femoral neck. In the femoral condyle, two specimens were retrieved.
The retrieved tissues were immediately fixed with neutral buffered formalin (10 %) and dehydrated in increasing concentration of ethanol up to 100 % at room temperature. A polyester resin solution (Rigolac; Mixture of resin no. 2004 and resin no. 70 °F, 80/20 (wt.%/wt.%); Showa Highpolymer Co., Ltd., Tokyo, Japan) was used for embedding. To prevent complete loss of the bone cement, the treatment in the first resin solution was minimized. Finally, the resin solution was kept in a chamber at 60 °C for 8 h and polymerized. The cured blocks were cut into slices 300–500 μm thick using a metal cutting saw and then ground down to sections 50–80 μm thick. Sections were examined by backscattered electron microscopy (SEM) and conventional light microscopy after staining with methylene blue or toluidine blue.
Table 2.1
Summary of results of loosening rate between bone and bone cement in groups 1, 2, and 3
|
Non-IBBC
|
IBBC
|
|||
|---|---|---|---|---|
|
79 Joints
|
12 Joints
|
|||
|
G. 1
|
R.L.L.
|
7 Joints not loosened
|
R.L.L.
|
Extremely low rate no progress
|
|
O.L.
|
O.L.
|
|||
|
L.
|
6 Joints not revised
|
L.
|
0
|
|
|
Revision, death, and lost
|
65
|
Death
|
3 Joints
|
|
|
Lost
|
3 Joints
|
|||
|
G. 2
|
Total: 25
|
|||
|
Survival in both hips for 25–26 years: 16 patients
|
||||
|
Loosening within 20 years
|
Acetabulum: 5 hips
|
L.
|
0 (except for separation between HA and cement)
|
|
|
Femur: 2 hips
|
||||
|
G. 3
|
285 Joints
|
|||
|
R.L.L.
|
Extremely low rate no progress
|
|||
|
O.L.
|
||||
|
L.
|
0
|
|||
2.2.4.2 Results
Bone ingrowth was observed in all interfaces where the HA granules were interposed on the living bone. Dense bone ingrowth was present in all specimens retrieved from the superior wall of the acetabulum. Among specimens from the inferomedial wall of the acetabulum, cancellous bone ingrowth was recognized in nine specimens and dense bone ingrowth was recognized in one (Fig. 2.7
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


