Chapter 19
Basic surgery for implant placement
This chapter discusses the surgical techniques for implant placement. Three different cases demonstrate individual techniques that can be considered when replacing teeth in different areas of the mouth.
Surgical placement of an implant to replace an upper first molar
Summary
A 55-year-old female presents with pain from UR6, which had been endodontically treated and crowned more than 10 years ago.
History
 History of complaint
History of complaint
The tooth was endodontically treated and a porcelain-fused-to-metal crown provided, which had remained functional for approximately 10 years. The patient first started to experience pain when biting on this tooth approximately 1 week ago; since then, the pain has become progressively worse.
Examination
 Intraoral examination
Intraoral examination
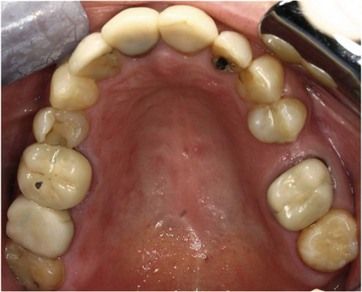
The dentition is heavily restored. Most of the posterior teeth are crowned or have intracoronal restorations (< ?xml:namespace prefix = "mbp" />
UR6 has a porcelain-fused-to-metal crown. The tooth is tender to percussion.
 Radiographic examination
Radiographic examination
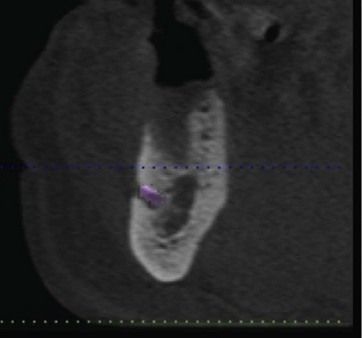
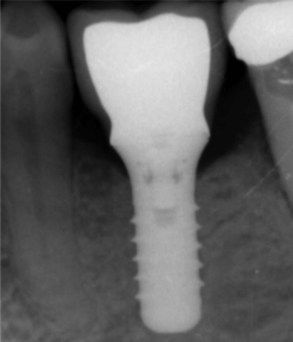
UR6: Single-cone root fillings are noted in the two buccal canals, and obturation voids are noted in the palatal canal. A slight widening of the lamina dura is noted in the mesiobuccal canal (
UR7: Single-cone root fillings are present in the buccal canals. The tooth has been restored with cast post and core crown.
UR5: Has a distal–occlusal restoration, with no periapical pathology.
What is the diagnosis and what factors will determine the prognosis of this tooth?
Diagnosis: Chronic periapical periodontitis in UR6.
The prognosis depends on two main factors:
Endodontic retreatment is possible and has a predictable outcome. The removal of existing obturation seems straightforward. However, one should be suspicious of a possible fourth canal (second mesiobuccal). A conscious effort to identify it and, if present, instrument appropriately is imperative in achieving success.
Moreover, the restorability of the tooth has to be determined. Although the tooth may be successfully treated after endodontic retreatment, the long-term prognosis will also depend on the underlying restorability of the tooth. It is advisable to dismantle the extracoronal restoration to investigate the amount of remaining tooth structure.
Once the crown was removed, underneath was primarily a core of composite resin. The mesial margin was subgingival (
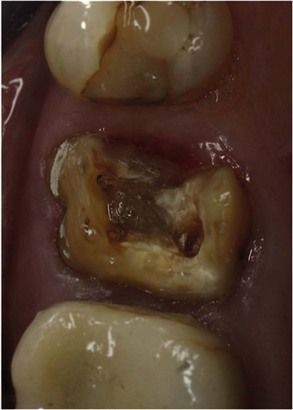
Fig 19.3 Removal of the existing restoration and underlying core, demonstrating lack of adequate coronal dentine.
After discussing the risks and benefits, it was decided to extract the tooth.
What replacement restorations would you consider and why?
1. Conventional three-unit bridge (UR5 to UR7)
Overall, a conventional bridge has a 10-year survival rate of 89.2% and would be cost-effective. However, UR7 is already restored with a post–core crown and would therefore be prone to a higher failure rate. In addition, UR5 has a small intracoronal restoration, and preparing it for a bridge would result in significant loss of healthy tooth tissue.
A single-tooth implant restoration is independent and does not require support from adjacent teeth. It would provide a long-term successful restoration, with a reported survival rate of 89.4% after 10 years. However, an implant requires a surgical procedure with its related postoperative complications, protracted treatment time, and it is expensive in comparison to conventional options.
After a detailed discussion about the options, the patient chose to have the tooth replaced by an implant-retained crown.
Preimplant assessment
 What factors would you consider when planning an implant to replace a maxillary and a mandibular molar?
What factors would you consider when planning an implant to replace a maxillary and a mandibular molar?
See
Table 19.1 Factors to assess when considering implant replacement of molar teeth
| Factor | Comments |
|---|---|
| Anatomical structures | Maxillary molar: maxillary sinus ( Mandibular molar: inferior dental canal and mandibular foramen ( |
| Bone height | Adequate bone height for the selected implant length using plain radiograph paralleling technique or a cone beam CT scan. In the mandible, watch for lingual concavity |
| Bone width | Clinical assessment and cone beam CT scan |
| Functional and aesthetic outcome | Although it is a molar, the final restoration should blend with the adjacent teeth |
| Implant selection | Implant with a wider body diameter is selected. It is desirable to choose an implant with a wider restorative head (platform), which will facilitate a good crown emergence for a molar tooth ( |
 Describe the surgical technique pertinent to molar region
Describe the surgical technique pertinent to molar region
As outlined in
The patient should sign an informed consent prior to surgery. The surgery can usually be performed under local anaesthesia. A crestal incision is extended to include a tooth on either side. A vertical releasing incision can also be made to gain better access. A surgical template is advisable and fabricated using an appropriate technique. A series of drills of widening diameters (
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses