Introduction
There is an increasing research interest in quality of life issues in orthodontics. In this study, we aimed to investigate changes in oral health related quality of life (OHRQoL) among adults during fixed orthodontic appliance therapy (FOAT).
Methods
Two hundred thirty-two adult patients were enrolled from a consecutive sample at a university dental hospital. OHRQoL was assessed by 2 standardized instruments (OHIP-14 and OHQoL-UK) at 4 times: before treatment (T0), 6 months after bonding and banding (T1), 12 months after bonding and banding (T2), and 18 months after bonding and banding (T3). Friedman 2-way analysis of variance (ANOVA) and Wilcoxon signed rank tests were used to compare the relative changes of OHRQoL among the different time points.
Results
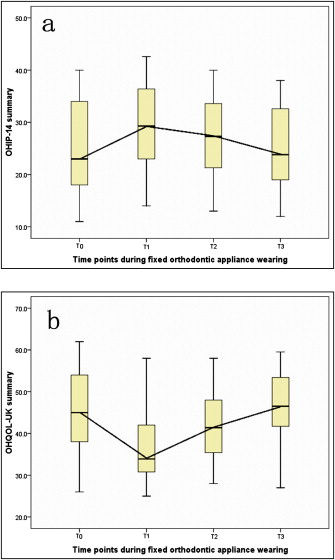
Significant changes in the summary scores of both the OHIP-14 and OHQoL-UK were observed during fixed orthodontic treatment ( P <0.001). There were significant OHRQoL deteriorations at T1 and T2 compared with T0; these were reflected by summary scores of both the OHIP-14 and OHQoL-UK as well as some of their domain scores ( P <0.05). However, at T3, the OHIP-14 suggested deterioration in OHRQoL, but the OHQoL-UK suggested improvement in OHRQoL.
Conclusions
Changes in OHRQoL occur during fixed orthodontic appliance therapy. In the early phase of treatment, the greatest deterioration in OHRQoL occurs. With ongoing treatment, the detrimental effects to OHRQoL are reduced.
Improved quality of life (QoL) is the ultimate goal of health care systems, particularly when services are provided for a health condition that is not life threatening. This has led to an extensive interest in QoL issues in medicine to assess the impact of various chronic health states on QoL and to assess outcomes from health care interventions in terms of QoL. In dentistry, there has been considerable interest in QoL issues, and a number of indexes have been developed to assess oral health-related QoL (OHRQoL). It has also long been recognized that the impacts of malocclusion, the motivating factors behind seeking care, and the outcomes from orthodontic care are related to QoL issues; thus there is a growing interest in QoL research in orthodontics.
Although improvement of QoL is often seen as the major goal of orthodontic care, it is accepted that, to obtain improvement in QoL, patients must experience some treatment-related side effects of wearing orthodontics appliances. Previous research has reported on the symptoms associated with wearing orthodontic appliances such as pain and discomfort. More recently, there have been calls for the need to assess the consequences of orthodontic treatment in the broader terms of QoL by using standardized OHRQoL measures to enable comparisons to be made of experiences encountered by different populations and changes over time. A cross-sectional study of adolescents undergoing orthodontic treatment reported that treatment-related experiences frequently impact on QoL and particularly among those undergoing fixed orthodontic appliance therapy (FOAT). Zhang et al reported on the effects of FOAT on childhood OHRQoL during the initial 6-month phase of treatment. There is a dearth of information on the experiences of adults in response to wearing orthodontic appliances in terms of QoL and of the ongoing experiences of FOAT beyond 6 months. Greater understanding of the dynamics of OHRQoL during orthodontic treatment is important on many fronts and, in particular, for informed consent so that patients can weigh the potential benefits of treatment in light of what they are likely to experience during treatment. In addition, understanding the sequelae associated with orthodontic treatment has implications with respect to treatment compliance and medicolegal situations. Ultimately, taking into account what patients will experience during orthodontic treatment can provide insight into the true benefits and health gains associated with orthodontic therapy.
In this study, we aimed to assess the impact from FOAT on QoL by investigating the changes in OHRQoL among adults during treatment.
Material and methods
This was a prospective longitudinal study involving a cohort of adults undergoing FOAT at Hong Kong University’s orthodontic teaching center. A consecutive sample of 347 adults seeking orthodontic treatment at the center was screened for suitability to undergo FOAT. Inclusion criteria were adults (aged 16 and older) rated as having a need for comprehensive fixed orthodontic treatment by the consulting orthodontists. Exclusion criteria were patients with untreated dental caries (cavitated lesions), periodontal diseases (periodontal pockets ≥4 mm), missing teeth in need of prosthetic rehabilitation; previous orthodontic treatment; and patients who were proposed to receive other types of orthodontic appliances aside from conventional labial FOAT (ie, lingual orthodontic appliance or Invisalign [Align Technology, Santa Clara, Calif]) or to be treated by combined FOAT and orthognathic surgery.
Assessment of OHRQoL was conducted by using 2 standardized measures: the short form of the oral health impact profile (OHIP-14) and the United Kingdom oral health-related quality of life (OHQoL-UK), whose psychometric properties have been evaluated in the local setting.
OHIP-14 is a short form of the oral health impact profile whose theoretic framework was based on the World Health Organization’s International Classification of Impairments, Disabilities and Handicaps relating health and its sequence in a hierarchy of different outcome levels. OHIP-14 has 7 conceptualized domains (2 items per domain): functional limitation, physical pain, psychological discomfort, physical disability, psychological disability, social disability, and handicap. Respondents are asked to rate how frequently they experienced an oral health impact (as described by each item). The response to each item was scored on a 5-point Likert scale: 0, never; 1, hardly ever; 2, occasionally; 3, fairly often; and 4, very often or every day. Summary OHIP-14 scores can range from 0 to 56, and domain scores can range from 0 to 8. A higher OHIP-14 score indicates poorer OHRQoL. The OHQoL-UK was developed based on the revised conceptual model of health as outlined in the World Health Organization’s International Classification of Impairments, Disabilities and Handicaps-2. This instrument assesses both the negative and positive impacts of oral health on QoL across 3 health domains: physical (6 items), psychological (5 items), and social (5 items). Each item is scored on a 5-point Likert scale: 1, very bad; 2, bad; 3, none; 4, good; and 5, very good. Summary scores of the OHQoL-UK can range from 16 to 80; the physical domain scores can range from 6 to 30, the social domain scores from 5 to 25, and the psychological domain scores from 5 to 25. A higher OHQoL-UK score indicates better OHRQoL.
Assessments of OHRQoL were conducted at baseline before banding and bonding of orthodontic treatment (T0), 6 months after banding and bonding (T1), 12 months after banding and bonding (T2), and 18 months after banding and bonding (T3). Since many participants had completed FOAT by 24 months, the study period was limited to 18 months.
Statistical analysis
Summary and domain scores of the 2 OHRQoL instruments were derived by summating responses of corresponding items. Nonparametric analysis methods were used in exploring the changes of OHRQoL during FOAT, since the data for both OHRQoL measures followed a Poisson distribution. First, Friedman 2-way analysis of variance (ANOVA) was used to compare the relative changes in OHRQoL scores at T1, T2, and T3 with a grouping method pairing OHRQoL scores of each subject at different treatment time points with that of his or her own baseline (T0) OHRQoL scores. Then, to identify time points at which OHRQoL significantly changed, the OHRQoL scores at T1, T2, and T3 were respectively compared with OHRQoL scores at T0 (T1-T0, T2-T0, and T3-T0) with the Wilcoxon signed rank test. In addition, changes in OHRQoL scores between adjacent time points (T2-T1 and T3-T2) were assessed by the Wilcoxon signed rank test to explore the direction and amount of changes during specific treatment phases.
Results
Of the 347 adults screened, 232 met with inclusion and exclusion criteria. Of the 232 subjects who were enrolled in the study, 201 (86.6%) completed the OHRQoL assessments at the 4 times during the study. The median age of the participants was 20 years (interquartile range, 5 years), and 63% (146) were female. There was no significant difference in the baseline OHRQoL assessments of those who completed all assessments (included in the analyses) and those who failed to complete all assessments (exluded for the analyses) ( P >0.05).
Significant changes in OHRQoL were observed during FOAT ( Fig ). There were significant changes in the OHIP-14 summary scores during FOAT ( P <0.001) and among 5 of its 7 domain scores (except for the handicap and physical disability domains): functional limitation ( P <0.001), physical pain ( P <0.001), psychological discomfort ( P <0.001), psychological disability ( P = 0.03), and social disability ( P <0.01) ( Table I ). There were also significant changes in summary OHQoL-UK scores ( P <0.001) and all of its 3 domain scores: physical ( P <0.001), psychological ( P <0.001), and social ( P = 0.02) during FOAT ( Table I ).
| T0 | T1 | T2 | T3 | P value | |||||
|---|---|---|---|---|---|---|---|---|---|
| Median | IQR | Median | IQR | Median | IQR | Median | IQR | ||
| OHIP-14 summary | 23.0 | 16.0 | 29.3 | 13.4 | 27.3 | 12.3 | 23.8 | 13.6 | <0.001 |
| Functional limitation | 3.0 | 2.0 | 4.9 | 1.6 | 4.0 | 1.4 | 3.8 | 1.3 | <0.001 |
| Physical pain | 3.0 | 3.0 | 5.1 | 1.6 | 3.5 | 2.3 | 3.1 | 1.3 | <0.001 |
| Psychological discomfort | 5.0 | 3.0 | 6.3 | 1.5 | 6.6 | 2.4 | 5.8 | 3.6 | <0.001 |
| Physical disability | 3.0 | 3.0 | 3.2 | 3.8 | 3.1 | 2.3 | 2.9 | 3.0 | 0.105 |
| Psychological disability | 4.0 | 3.0 | 4.7 | 2.6 | 4.8 | 2.9 | 4.6 | 3.6 | 0.032 |
| Social disability | 2.0 | 3.0 | 2.7 | 0.7 | 2.8 | 0.4 | 2.6 | 1.4 | 0.007 |
| Handicap | 3.0 | 4.0 | 3.1 | 2.5 | 2.9 | 3.3 | 3.2 | 3.4 | 0.081 |
| OHQoL-UK summary | 45.0 | 16.0 | 33.9 | 11.2 | 41.4 | 12.6 | 47.3 | 11.7 | <0.001 |
| Physical | 16.0 | 4.0 | 10.8 | 7.8 | 13.4 | 8.9 | 15.8 | 8.0 | <0.001 |
| Psychological | 15.0 | 3.0 | 13.8 | 7.5 | 13.9 | 9.1 | 13.7 | 6.5 | <0.001 |
| Social | 14.0 | 3.0 | 10.2 | 5.9 | 14.3 | 7.0 | 16.7 | 6.7 | 0.016 |
Compared with T0, at T1 and T2, there were significant increases in the OHIP-14 summary scores ( P <0.01) and in 5 of its 7 domain scores ( Table II ). At T3 compared with T0, there were significant increases in the OHIP-14 summary scores ( P = 0.04) and in 2 of its 7 domain scores. With respect to the OHQoL-UK scores, at T1 compared with T0, there were significant decreases in summary OHQol-UK scores ( P <0.001) and all of its domain scores ( Table II ). Compared with T0, at T2, there were also a significant decrease in summary OHQoL-UK scores ( P <0.01) and a significant increase in the physical and psychological domains scores. At T3 compared with T0, there were a significant increase in the summary OHQoL-UK scores ( P = 0.04), a significant increase in the social domain score, and a significant decrease in the psychological domain score.
| T1-T0 | T2-T0 | T3-T0 | ||||
|---|---|---|---|---|---|---|
| Median | IQR | Median | IQR | Median | IQR | |
| OHIP-14 summary | 6.4 ‡ | 4.0 | 3.7 † | 4.4 | 1.2 ∗ | 6.3 |
| Functional limitation | 1.9 † | 2.0 | 1.2 † | 1.6 | 0.5 | 2.4 |
| Physical pain | 2.0 † | 1.0 | 1.3 † | 1.6 | 0.5 | 2.3 |
| Psychological discomfort | 1.5 ∗ | 2.0 | 1.7 ∗ | 1.5 | 1.1 ∗ | 2.4 |
| Physical disability | 0.3 | 0.5 | 0.5 | 1.8 | −0.1 | 1.3 |
| Psychological disability | 0.7 ∗ | 2.0 | 0.7 ∗ | 2.6 | 0.8 ∗ | 3.9 |
| Social disability | 1.1 † | 2.4 | 1.0 ∗ | 2.5 | 0.8 ∗ | 2.3 |
| Handicap | 0.2 | 1.0 | −0.1 | 2.5 | 0.1 | 3.3 |
| OHQoL-UK summary | −10.2 ‡ | 6.4 | −5.2 ‡ | 7.2 | 2.1 ∗ | 4.3 |
| Physical | −4.6 ‡ | 4.0 | −2.8 † | 5.7 | −0.5 | 3.9 |
| Psychological | −1.1 † | 3.8 | −1.5 † | 4.5 | −1.3 ∗ | 5.0 |
| Social | −2.5 † | 4.9 | 0.2 | 1.9 | 2.3 † | 5.7 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


