Chapter 23 Bipolar radiofrequency cold ablation turbinate reduction for obstructive inferior turbinate hypertrophy
1 INTRODUCTION
Nasal obstruction secondary to inferior turbinate hypertrophy is a common compounding problem for many patients with obstructive sleep apnea and/or snoring (OSA/S).
2 PATIENT SELECTION
With respect to inferior turbinate hypertrophy, the relative size of the inferior turbinate along its full length must be assessed. It is not uncommon to find patients with relatively normal-appearing anterior inferior turbinates, but with very pronounced posterior (tail) cobblestoned turbinate hypertrophy. The relationship of the inferior turbinate hypertrophy to nasal septal deviation in particular should be assessed. Some patients with septal deviation may yet still be candidates for inferior turbinate reduction alone if the turbinate component is felt to contribute substantially more to the nasal obstruction. Unfortunately, no clear-cut testing modality will define the individual contributions to nasal obstruction for these anatomic factors. However, we and others have found that a topical nasal decongestant test with neosynephrine or oxymetazoline may help identify patients more likely to benefit from inferior turbinate reduction. Patients must be cautioned that this pharmacologic turbinate reduction is supraphysiological and may exaggerate what is achievable with mechanical inferior turbinate reduction. Those patients who demonstrate an improvement in their subjective sense of nasal breathing and/or objectively demonstrate improvement in their nasal patency (as measured by acoustic rhinometry or nasal endoscopy) are more likely to achieve benefit with inferior turbinate reduction alone. We avoid mixing topical lidocaine in conjunction with topical decongestants because it may confound the patient’s subjective assessment of their nasal breathing. A small fraction of patients will have limited improvement with topical decongestion, still demonstrating large inferior turbinates. These patients often have a large bony (concha) inferior turbinate and may be better candidates for submucous resection techniques. Patients with significant nasal septal deviation (especially in the anterior or mid-nasal cavity), sinonasal polyposis or adenoid hypertrophy are often not good candidates for inferior turbinate reduction alone.
3 OUTLINE OF PROCEDURE
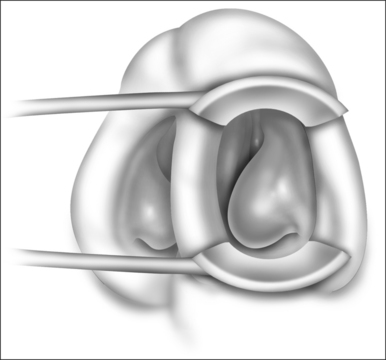
Patients are positioned upright in the procedure chair in the clinical examination room. Visualization of the anterior aspect of the nasal cavity is readily provided by a nasal speculum and headlight illumination as seen in Figure 23.1. The inferior turbinate dimensions both in terms of cross-sectional area occupied and anterior–posterior length of hypertrophy are determined. Infrequently, preoperative sedation or preoperative pre-emptive pain medication may be provided for anxious individuals. The procedure for anesthesia of the nasal cavity is a very important component of outpatient coblation inferior turbinate reduction and actually takes up much of the operative time. The nasal cavity is sequentially anesthetized, first with spray application of a lidocaine/phenylephrine mixture. After a few minutes, this is then followed by a direct contact anesthesia applied in the form of a cottonoid pledget soaked in cetaccainephenylephrine which is placed in the anterior one half of the nasal cavity, maximizing contact with the inferior turbinate. After an additional few minutes have elapsed, these pledgets are removed, an additional 2–3 ml up 2% lidocaine has infiltrated in each anterior inferior turbinate head, extending from the mucosal surface to the periosteum of the inferior concha. Additionally, we have found that further anesthetic injections just lateral to the piriform aperture, slightly anterior to the anterior head of the inferior turbinate, provide additional anesthesia to the infraorbital nerve branches to the inferior turbinate, increasing patient comfort and tolerance for the procedure. Occasionally, even after these steps with anesthesia, patients still may have some pain with the coblation procedure, especially as the middle to posterior aspects of the inferior turbinate are treated. In these patients, it is helpful to provide a sphenopalatine nerve block with a slightly bent spinal needle as indicated in Figure 23.2. For a sphenopalatine nerve block, 1–2 ml of 1% lidocaine with epinephrine are instilled just posterior and slightly inferior to the posterior attachment of the middle turbinate. This is best done with a 3 ml injection syringe coupled to a slightly bent 22-gauge spinal needle (Fig. 23.3). On occasion, endoscopic guidance may facilitate this posterior nerve block. Alternatively, a transoral, greater palatine foramen approach to the sphenopalatine ganglion for this additional nerve block may be employed.
< div class='tao-gold-member'>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses