This chapter discusses the assessment of pathology and abnormal function of the temporomandibular joint. If one is to comprehend the pathologic processes resulting in pain and dysfunction of the temporomandibular joints, a clear understanding of normal anatomy and biomechanics is essential. Assessment of the temporomandibular joint, typically performed on a symptomatic patient, requires an understanding of the various clinical conditions that encompass temporomandibular disorders.
TEMPOROMANDIBULAR DISORDERS
Temporomandibular disorders (TMDs) are defined as clinical problems involving the masticatory musculature, the temporomandibular joints (TMJs) and associated structures, or both. Articular disorders of the TMJ often coexist with masticatory muscle pain, and a clear differential diagnosis is necessary, especially when a surgical consideration is possible. Articular disorders include disc displacement disorders, arthritic or degenerative changes, and neoplasm. Other conditions that may affect the temporomandibular joints include congenital disorders, inflammatory conditions, and systemic disease.
TMD is considered the most common musculoskeletal disorder that causes orofacial pain. Three cardinal signs of a temporomandibular disorder may be evident: (1) pain with mandibular function, (2) limitation of mandibular movement, and (3) joint sounds. One, two, or all three conditions, when present, may represent signs of chronic adaptation of the anatomy of the joint that require no treatment interventions, or they may reveal symptoms of dysfunction that may limit the activities of daily life because of pain or a limited ability to masticate.
Although pain in the masticatory system can arise from the muscles of mastication or can be referred to the orofacial region from remote musculoskeletal structures, a discussion of muscle pain is not within the scope of this chapter. However, it is important to keep in mind that myogenous pain occurs more frequently than pain due to articular disorders.
A differential diagnosis of myogenous pain and dysfunction as opposed to a true internal derangement or temporomandibular joint dysfunction is essential if successful treatment is to be effected. For the purpose of classification, temporomandibular disorders will be considered as pain or dysfunction of the musculoskeletal system involving the temporomandibular joints and the masticatory muscles.
With myogenous pain, the patient typically provides a history of regional pain, a sense of muscle weakness, easy fatigability of the masticatory muscles, and limited passive mandibular range of motion. Palpatory examination of the masticatory muscles often reveals myofascial trigger points and muscle tenderness, which also can produce referral patterns to the region of the temporomandibular joints.
Included in the myogenous pain group are conditions such as myositis or muscle inflammation, which often result from local trauma or infection. Upon palpation, muscles with myositis also may be tender and may feel swollen and warm.
Myospasm is an often overused diagnostic term. It describes an involuntary muscle contraction. The patient with myospasm may present with a restricted mandibular range of motion that must be differentiated from an internal derangement of the joint, because this condition also can restrict mandibular movement. Spastic muscles may be tender to palpation. True myospasm can be diagnosed by needle electrode electromyography.
With time, masticatory muscles that exhibit chronic contraction or other local myopathies may develop myofibrotic contracture. This may not be a painful condition, but it also will limit the mandibular range of motion. For this reason, a differential diagnosis requires a detailed history and thorough evaluation. Myofibrotic contracture may be characterized by local tenderness and may be differentiated from other forms of muscle disorders via needle electrode electromyography.
ANATOMY
The temporomandibular articulation is among the most complex in the body. It is a synovial joint that has two joint compartments, four articular surfaces, contains vascularized tissue within the joint capsule, and has articular surfaces of fibrocartilage, rather than chondrocartilage.
The temporomandibular joint functions within the glenoid or temporomandibular fossa of the skull. The fossa is located in the temporal bone bilaterally, just anterior to the external auditory meatus. The TMJ fossa is not so much of a precise socket, but more of a depression in the base of the skull, within which the mandibular condyle functions.
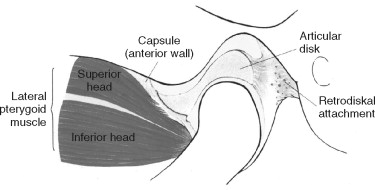
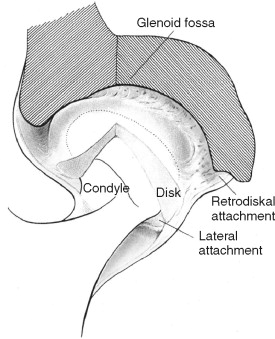
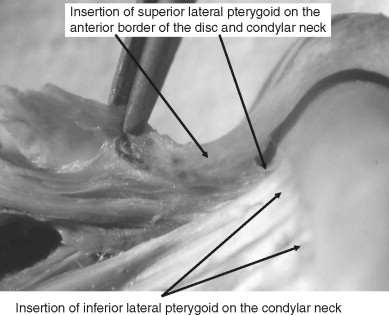
The mandibular condyle is a spheroidal structure that is capable of a wide range of anterior, posterior, and lateral movements. The fibrocartilagenous articular surfaces of the condyle and fossa function against the fibrous interarticular disc that is interposed between these two structures ( Figure 43-1 ). The disc is attached to the mandibular condyle by lateral and medial collateral ligaments and blends into the capsule anteriorly. Posteriorly, the disc attaches to the complex retrodiscal tissues. Although the disc is avascular and is not innervated, retrodiscal tissue is highly vascularized and richly innervated ( Figure 43-2 ). Therefore, intracapsular pain may be due to injury or inflammation of the retrodiscal tissue (retrodiscitis).
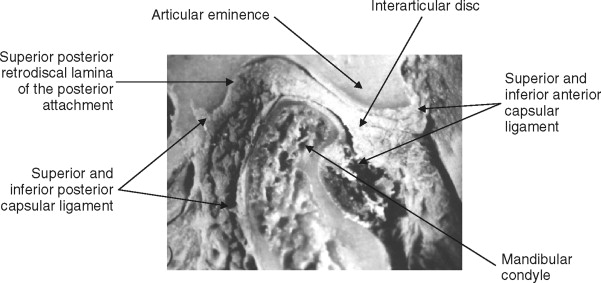
The temporomandibular joint is a synovial joint; by definition, it is encapsulated and stress bearing. The disc and its circumferential attachments separate the joint into upper and lower joint spaces. The disc–condyle complex and the mandibular fossa are enclosed within the capsular ligament, which is lined by synovial tissue with collateral ligaments that blend into the capsule. The TMJ lateral ligament complex arises from the articular eminence and attaches to the posterior aspect of the neck of the condyle ( Figure 43-3 ). The lateral ligament complex functions to limit lateral movement.
NORMAL BIOMECHANICS
The TMJ is a ginglymoarthrodial joint that is capable of both rotational and translational movements ( Figure 43-5 ). During function, the lateral and medial discal collateral ligaments allow for rotational movement of the condyle on the inferior surface of the disc, and the superior surface of the disc translates or slides along the posterior aspect of the articular eminence. Biomechanically, the TMJ exhibits significant mobility. The mandibular condyle freely rotates on the inferior surface of the interarticular disc, and the disc–condyle complex moves within the fossa and translates unimpeded along the posterior slope of the articular eminence. In addition, limited lateral movements are possible. During all of these movements of a normal temporomandibular joint, the interarticular disc is always positioned between the fossa/eminence and the condyle by the action of the superior lateral pterygoid muscle and the uppermost elastic properties of the posterior attachment known as the posterior, superior retrodiscal lamina of the retrodiscal tissue. Translation of the condyle occurs as a result of the action of the inferior lateral pterygoid muscle, which protrudes the mandible, acting in concert with other mandibular depressors of the infrahyoid and suprahyoid musculature. Movement of the disc is also controlled by a second structure. The superior, posterior retrodiscal lamina acts passively to pull the disc posteriorly during opening as the condyle translates anteriorly. The superior lateral pterygoid muscle contracts eccentrically during closure to stabilize the disc against the distal slope of the articular eminence ( Figure 43-4 ). Normal disc/condyle/fossa relationships are demonstrated in the illustration below ( Figure 43-6 ).
ABNORMAL BIOMECHANICS
Smooth and coordinated opening and closing, in the absence of pain or joint sounds, characterize normal function of all synovial joints, including the TMJ. Signs of a TMD therefore include limited or irregular jaw movements, discomfort, and/or sounds emanating from the joint during function.
Impediments to normal joint movement can be extracapsular or intracapsular. A temporomandibular joint assessment must differentiate between the two.
As was previously discussed, extracapsular conditions that affect joint movement typically are caused by muscle dysfunction, although osseous anomalies also may interfere with mandibular movement. These include coronoid hypertrophy, calcified styloid processes, osteochondromatosis, or other bony abnormalities ( Figures 43-7 through 43-9 ).


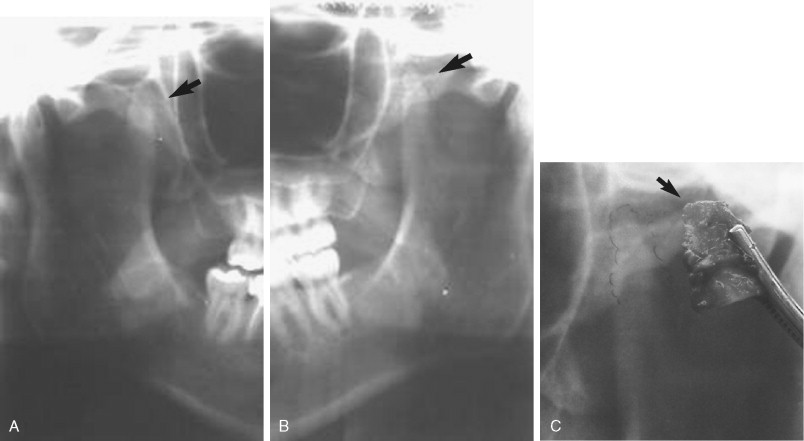
Synovial chondromatosis is an uncommon arthropathy, but it is one that should be considered in the differential diagnosis of TMJ–pain dysfunction syndrome ( Figure 43-10 ). Limitation of mandibular function caused by calcified bodies found within the TMJ capsule may displace the mandibular condyle, impede mandibular function, and mimic disc displacement or disc interference disorders.

Myofascial pain, myositis, myalgia, and muscle contracture not only can limit mandibular depression but also can result in pain during movement. Myofascial trigger points of the masticatory musculature can refer pain to the TMJ. Care must be taken during the history and physical examination to clearly define the source of the problem. If it is assumed that mandibular dysfunction is not due to extracapsular myogenous causes, attention next will be directed at possible intracapsular disorders.
INTRACAPSULAR PATHOFUNCTIONAL DISORDERS
Intracapsular pathofunctional disorders include anterior disc displacement with and without reduction.
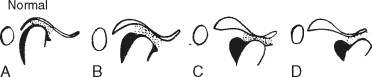
Anterior disc displacement is characterized by a partial anterior or anteromedially displaced disc. Chronic anterior disc displacement may occur for a variety of reasons and may be an adaptive change that occurs within the joint as a result of functional demands ( Figure 43-11 ).
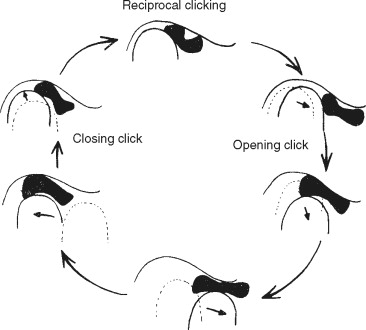
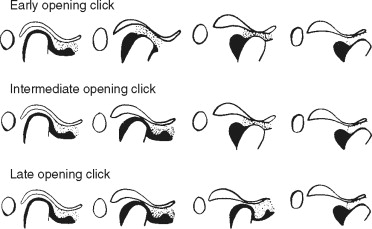
Anterior disc displacement with reduction is characterized by joint sounds during function that occur at variable points during mandibular movement ( Figure 43-12 ).
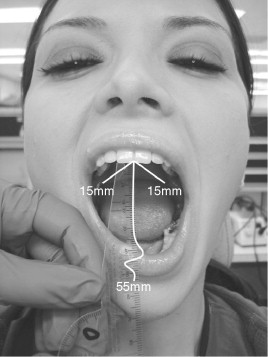
Differential diagnosis involves a physical examination in which the mandibular range of motion is measured, the gait of movement is observed, and the joint is auscultated.
The mandibular range of motion has been reported in the literature as within normal limits at approximately 40 to 55 mm. Normal range of motion is less in women and decreases with increasing age. However, this is only a guide in that the range of motion often depends upon the stature of the patient. A patient of small stature might have a mandibular range of motion of less than 40 mm, and that of a larger individual might approach 60 mm. A more accurate measure of normal opening might involve assessment of condylar translation to the crest of the articular eminence. This may be seen radiographically, but the use of x-ray or magnetic resonance imaging (MRI) for this purpose is not suggested; use of these methods would be considered overutilization of diagnostic imaging.
Soft tissue imaging such as MRI can reveal a displaced disc that improves its position during jaw opening. Hard tissue imaging may show an absence of degenerative changes, even though adaptive remodeling of the articular surfaces may occur. Disc displacement with reduction also may be accompanied by pain with joint movement and deviation of the mandible during opening, possibly coinciding with a click as the displaced disc returns to normal. No restriction is placed on mandibular movement despite the possibility of an episodic and momentary catch during jaw movement. An abnormal disc/condyle relationship is characteristic of disc displacement with reduction.
Disc displacement without reduction is typically chronic but initially presents as an acute problem. Some patients with anterior disc displacement with reduction evolve to non-reducing disc displacement. However, it is impossible to speculate which patient with an anterior disc displacement with reduction will evolve to more advanced dysfunction.
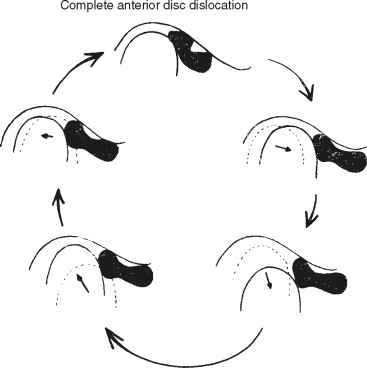
Anterior disc displacement without reduction is the state in which the anteriorly displaced disc is maintained in this position throughout translation. This is often referred to as a closed lock . Essentially, the disc no longer allows the condyle to translate along the articular eminence. Thickening of the disc or damage to the posterior attachment may contribute to the disc’s getting caught or may interfere with condylar movement.
A patient with disc displacement without reduction frequently has a history of clicking during mandibular movement. A non-reducing disc displacement typically occurs in the absence of joint sounds. Soft tissue imaging reveals a displaced disc that does not improve its position during jaw opening. Hard tissue imaging may show degenerative changes. An acute closed lock or non-reducing anterior disc displacement has a sudden onset with nearly immediate limited mouth opening of less than 25 mm. The mandible deflects to the affected side, and lateral movement to the opposite side is limited. Soft tissue imaging reveals the displaced disc, although hard tissue imaging may be normal.
Chronic anterior disc displacement without reduction or chronic closed lock typically includes a history of sudden onset of limited mouth opening with continued limitation of opening for longer than 4 months. Soft tissue imaging shows the displaced disc without reduction. Typically, arthritic or degenerative changes are not extensive ( Figure 43-13 ).
Another post-traumatic condition that may affect mandibular and TMJ function involves intracapsular adhesions. As was previously described, the TMJ functions within a capsular ligament. This ligament exhibits varying degrees of toughness, with the strongest portion at the medial aspect of the superior joint space. The superior/anterior TMJ capsular ligament is comparatively fragile. A sudden hypertranslation or condylar subluxation could allow the condyle to traumatically encroach on this structure. If injured, bleeding may occur into the superior joint space, resulting in the organization of fibrous bands known as adhesions. These intracapsular adhesions can prevent normal translation of the disc and, while giving the appearance and history of chronic disc displacement without reduction, can actually fixate the disc to the roof of the fossa. MRI or computed tomography (CT) may show the disc in a normal, closed position.
Another explanation for what appears to be a clinical closed lock in the presence of a normal discal position has been described. A sudden and persistent severely limited mouth opening associated with a total lack of disc translation along the articular eminence may be due to adhesion of the disc to the articular eminence. In view of the fact that it is promptly released by lavage (arthrocentesis) of the upper joint space, inefficient lubrication of the joint secondary to joint overloading is hypothesized. It has been postulated that this overloading may reduce lubrication and may be responsible for adhesion of the disc to the fossa and/or eminence. This also may explain the immediate release of the disc following arthrocentesis.
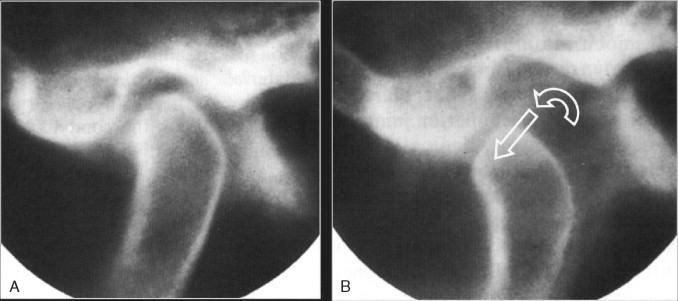
In contrast to hypomobility caused by disc interference or muscle contraction is the chronic subluxation or hypermobility that is seen when, because of laxity of the supporting ligaments, the mandibular condyle translates beyond the articular eminence. Subluxation of the condyle will result in a soft or hard click as the condyle passes beyond the articular eminence at maximum opening. This is accompanied by unilateral or bilateral deflective movements at the end of the opening range. The joint sound associated with a subluxation should not be confused with that of a disc interference disorder ( Figure 43-14 ).
Aside from mechanical dysfunction of the TMJ, inflammation that may accompany abnormal joint mechanics may contribute to the patient’s discomfort. Intracapsular swelling from inflammation also may impede joint movement. Inflammation of the joint capsule (capsulitis) or inflammation of the joint lining (synovitis) can result in pain with jaw movement.
Trauma to the highly innervated and richly vascularized retrodiscal tissue, as might occur with a blow to the jaw that drives the condyle upward and backward, can impart a direct trauma to this tissue, resulting in swelling and pain. Pain within the joint may result in secondary muscle splinting or protective guarding of the joints that may cause a more limited mandibular range of motion and pain. Inflammatory mediators within the injured joint may perpetuate pain and dysfunction. Synovial fluid may be diminished in quality and/or quantity; this compromises nutrition of the articular surfaces and diminishes protection and lubrication of the joints. Although the quality of synovial fluid within an inflamed joint may be poor, a tendency for excessive synovial fluid formation may result in increased intracapsular pressure, which may lead to further dysfunction and pain.
EVALUATION
The goals of any treatment regimen regarding injury to, or dysfunction of, a joint are the restoration of function and the elimination or reduction of pain. The approach to management of a TMJ injury or dysfunction is similar to that of treatment for other joints.
Regardless of the cause, pain and dysfunctional movements and sounds during function characterize a TMD. Although trauma may have been the precipitating event leading to the onset of the patient’s complaints, contributing factors may result in lengthier and less productive treatment, if they are not recognized and eliminated. Therefore, the first goal in implementing a well-defined management program is to identify contributing factors. This involves addressing physical, emotional, and psychological factors.
A comprehensive evaluation must include a detailed history that reviews the following:
- •
Chief complaint
- •
History of the present illness
- •
Chronology of onset
- •
Description of any trauma
- •
- •
Patient’s medical and dental histories
- •
Prior history of joint dysfunction
- •
Has this individual ever been treated for a similar problem?
- •
What were the results of that treatment?
- •
Are any comorbid systemic disorders present?
- •
- •
Findings of the clinical examination include the following:
- •
Evaluation of the muscles of mastication and the supporting muscles of the neck and shoulders
- •
Conditions found within the oral cavity that might be contributing to the patient’s pain complaints (i.e., an evaluation of the soft tissues, periodontium, and teeth)
- •
Myofunctional and/or parafunctional habits
- •
Mandibular range of motion measurements
- •
Auscultation of the temporomandibular joints during movement
- •
- •
Radiologic findings
DIAGNOSTIC IMAGING
Temporomandibular disorders often involve displacement or dislocation of the interarticular disc and arthritic changes in the bony components of the joint. These alterations from normal anatomy and function may result from various causes, including trauma, degenerative joint processes, developmental anomalies, and neoplasm. It is acceptable to include some form of diagnostic imaging in a temporomandibular joint evaluation to facilitate diagnosis. Various methods of radiologic imaging are available.
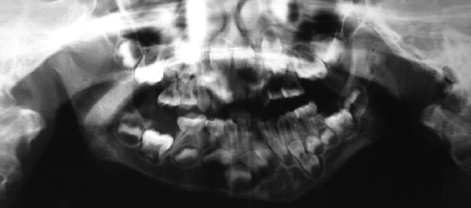
The most readily available diagnostic radiograph used in the dental office is the panoramic radiograph. This type of study often is all that is necessary to identify fractures, gross arthritic changes, or hard tissue abnormalities, such as tumors, bone cysts, or malformations ( Figures 43-15 and 43-16 ).

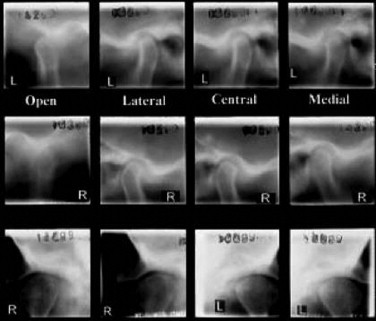
The next most common radiographic study, which also is easily performed in a dental office, is the transcranial view. This study, which uses standard dental x-ray equipment, normally includes views of each condyle in the open, closed, and rest positions. Transcranial radiographs provide information concerning the contours of bony elements. Transcranial radiographs often are inappropriately used to determine condylar position in the fossa—a determination that is not possible with this type of study. As with the panoramic radiograph, transcranial radiographs may be useful in ruling out gross arthritic changes, as well as fractures. Although greater detail is offered on transcranial radiographs, the information provided is similar to that seen on the panoramic radiograph ( Figure 43-17 ).
Tomography also offers an evaluation of the osseous structures ( Figure 43-18 ). It is a more accurate study in that it can focus on planes (“cuts”) that are only several millimeters thick. This ability enables a tomographic study to evaluate a temporomandibular joint similarly to a loaf of bread, that is, to evaluate one slice at a time. Greater detail of the articular surfaces is rendered. More accurate information regarding condylar displacement and arthritic changes also may be attained.
Cone-beam computed tomography (CBCT) is increasingly being used as an imaging modality in the assessment of the temporomandibular joint and has been reported to provide superior reliability and greater accuracy than standard tomography and TMJ panoramic projections in the detection of condylar cortical erosion. However, other studies report that CBCT has not yet been shown to offer significant differences in diagnostic accuracy from that available with conventional tomograms.
Although transcranial, tomographic, and cone beam studies are acceptable for evaluating hard tissues of the temporomandibular joints, these do not show the interarticular disc. One of the objectives of conservative temporomandibular joint therapy is to attempt to reduce, or return, a displaced disc to a more normal relationship to the mandibular condyle. Often, conservative therapy fails to achieve this goal. In such a case, it may be necessary to determine the location of the disc.
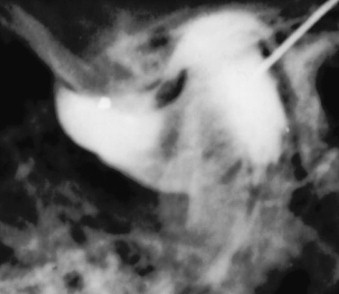
Various imaging techniques may be used to determine the position of the interarticular disc. Arthrography is an excellent method of imaging disc position. It is performed by injecting a small amount of radiopaque material into the inferior and/or superior joint compartment. The radiopaque solution outlines the disc ( Figure 43-19 ). This procedure, which may be combined with video fluoroscopy, provides a great deal of information. Difficulties associated with this type of radiographic study include the following: (1) it is often painful for the patient, (2) it requires a great degree of expertise on the part of the radiologist, and (3) it exposes the patient to a significant amount of radiation. This test is now performed very infrequently but is of historic value and has been replaced by MRI.
Non-invasive imaging studies include the CT scan and the MRI. Computerized axial tomography has the capacity to image not only the hard, bony tissues but soft tissues as well. Through computerized analysis of the x-ray signal, soft tissues such as the temporomandibular joint disc may be visualized ( Figure 43-20 ). This procedure has proved fairly accurate in its depiction of discal position, although the image often lacks detail. On the negative side is the fact that with this test, as with arthrography, the patient receives substantial radiation.

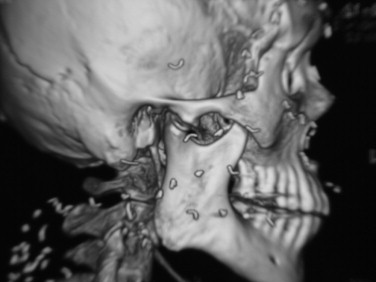
Enhanced osseous detail is obtained with the use of three-dimensional (3D) CT ( Figure 43-21 ).
MRI represents the current gold standard of diagnostic imaging technology. It does not use radiation at all. The image is produced through computer analysis of signals emitted by the oscillation of molecules of water that contain soft tissues in a magnetic field. These signals are produced by placing the patient into a strong magnetic field. MRI is quite effective. The detail of soft tissues that an MRI study can reveal is often quite remarkable. Not only can MRI allow visualization of the TMJ interarticular disc, often in more detail than former studies, it also can reveal scar tissue and inflammation of soft tissues when called upon to do so ( Figure 43-22
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


