Introduction
The aim of this study was to assess the bone morphology of teeth mesialized into the grafted region in patients with unilateral alveolar cleft.
Methods
The sample comprised 30 patients with unilateral cleft lip and palate with a mean age of 20.5 years. High-resolution cone-beam computed tomography images of the maxilla were obtained 6 months to 2 years after comprehensive orthodontic treatment. The contralateral canines and lateral incisors were used as controls. Axial section was used to measure the bone thickness, and cross section was used to measure the alveolar crest height using the cementoenamel junction as a reference. Paired t tests and Wilcoxon tests were used to compare the cleft and noncleft sides ( P <0.05).
Results
High individual variability was found. In general, the canines in the cleft side had statistically thinner buccal bone plates than the contralateral teeth. No differences between the cleft and noncleft sides were found for the lingual bone plate thickness. The canine on the cleft side showed a slightly greater distance between the lingual alveolar crest and the cementoenamel junction than the lateral incisor in the noncleft side.
Conclusions
In patients with unilateral cleft lip and palate, mesial orthodontic movement of the maxillary canines into the grafted alveolar cleft results in acceptable buccal and lingual periodontal morphology.
Highlights
- •
Canines moved into the grafted alveolar cleft show adequate periodontal insertion.
- •
Buccal bone dehiscence is found in a minority of canines moved to the grafted cleft.
- •
Ortho-perio integration may prevent gingival recession in mesialized canines.
Cleft lip and palate (CLP) is the most common congenital craniofacial malformation in humans. The rehabilitation protocol of CLP includes lip and palate repair during the first months and year of life, respectively. During the late mixed dentition, an alveolar bone graft is indicated to rehabilitate the alveolar cleft. After the secondary alveolar graft surgery, the maxillary canines spontaneously erupt through the grafted region in most patients.
Patients with CLP often have agenesis of the maxillary lateral incisors. The gold standard treatment plan after alveolar bone graft surgery is to mesially move the maxillary canines to replace the missing lateral incisors. This procedure stimulates maintenance of the alveolar bone graft at the cleft region and avoids the need for tooth prosthesis. After canine substitution for missing maxillary lateral incisors, esthetic dentistry is performed to complete treatment similarly to that for noncleft patients with maxillary lateral incisor agenesis.
Orthodontic tooth movement into an edentulous alveolus is critical in terms of alveolar bone response. Bone remodeling around the tooth root depends on the magnitude of force, the amount of tooth movement, and the presence of bacterial plaque. Despite our knowledge of periodontal responses to orthodontic treatment, there is lack of information regarding the response of grafted bone to orthodontic therapy in cleft patients. Since the grafted alveolar cleft has buccolingual constriction of the alveolar ridge, during comprehensive orthodontic treatment for canine substitution, does movement of the maxillary canine toward the grafted area occur within the bone or through the bone?
Previous studies have demonstrated that maxillary canines that erupt through the graft have similar periodontal conditions to canines erupted in normal bone. These studies, however, analyzed only the mesial and distal alveolar bone by means of periapical radiographs. No previous study has evaluated the buccal and lingual bone plates of maxillary canines moved into the grafted area. Therefore, the purposes of this study were to evaluate the buccal and lingual alveolar bone thicknesses and levels of canines moved into the grafted alveolar cleft, and to compare these characteristics with the contralateral teeth in patients with unilateral CLP. The null hypothesis is that the teeth on the cleft and noncleft sides have similar buccal and lingual alveolar bone morphology.
Material and methods
Institutional research ethics committee and written patient and parent consents were obtained. The confidentiality and rights were protected. The sample size calculation was based on preliminary statistics including the first 5 patients of the sample. For a standard deviation of 0.13 mm for bone thickness and a minimal intergroup difference of 0.10 mm to be detected, a sample of 28 patients was required to provide statistical power of 80% with an α of 0.05.
From August 2011 to January 2012, a sample of 30 patients with unilateral alveolar cleft from 1 rehabilitation center was consecutively selected. Twenty-two patients had complete unilateral CLP, and 8 had unilateral cleft lip and alveolus. The patients were examined at the orthodontic department of the Hospital of Rehabilitation of Craniofacial Anomalies, University of São Paulo, in Brazil during their appointments for retainer adjustment. The inclusion criteria were (1) minimum retention period of 6 months after debonding, (2) age between 15 and 25 years, (3) history of secondary alveolar bone graft surgery with iliac crest autogenous bone, (4) presence of canines and lateral incisors in the noncleft side, (5) agenesis of the lateral incisor at the cleft side, and (6) comprehensive orthodontic treatment including mesial movement of the maxillary canines toward the grafted alveolar cleft. The exclusion criteria were patients with syndromes. The final sample comprised 14 female and 16 male subjects with a mean age of 20.5 years and a mean retention period of 1.8 years. The ratio between the right and left sides of the cleft was approximately 1:2.5. The mean age when the secondary alveolar bone graft was performed was 11.8 years. Three surgeons performed the bone graft procedure using the same technique. At the time of secondary alveolar bone graft, 36% of the patients had their permanent canine partially erupted on the cleft side. In 58% of the patients, the permanent canine at the cleft side spontaneously erupted after the bone graft, whereas 7% of the patients needed canine traction.
Orthodontic movement of the canine after the secondary alveolar bone graft began 2 months after surgery for patients who had the canine erupted at the time of surgery. For patients who had the secondary alveolar bone graft before canine eruption, comprehensive orthodontic treatment was initiated only after the cleft-side canine had erupted. Comprehensive orthodontic treatment started a mean of 18.6 months after the secondary alveolar bone graft surgery (SD, 17.1 months). No regrafting surgery was needed. Only 2 of the 30 patients underwent orthognathic surgery.
This study had a split-mouth design. The experimental group consisted of the maxillary canines at the cleft side (C3). The control group consisted of the maxillary canines (NC3) and the lateral incisors (NC2) on the noncleft side.
Cone-beam computed tomography (CBCT) was performed with an i-CAT cone-beam 3-dimensional system (Imaging Sciences International, Hatfield, Pa). The technical parameters for image acquisition were 120 kV, 23.87 mA, field of view of 16 × 6 cm, and voxel size of 0.25 mm.
Initially, the CBCT image was standardized in the sagittal view, positioning the palatal plane parallel to the horizontal plane. In the frontal view, the occlusal plane was coincident to the horizontal plane. Finally, in the axial sections, the vertical guideline was positioned at the midline of the central incisors ( Fig 1 ).
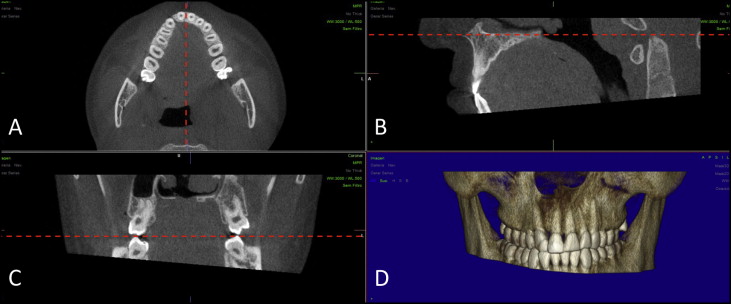
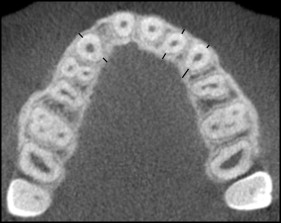
In the frontal and sagittal images, an axial section passing through the trifurcation of the right first permanent molar was selected. On this image, the buccal and lingual alveolar bone thicknesses were measured on the C3 and on the NC3 and NC2 ( Fig 2 ).
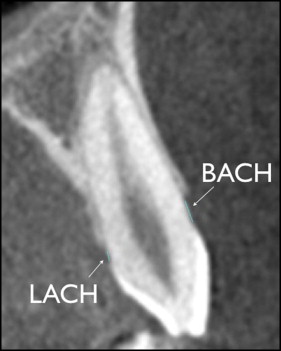
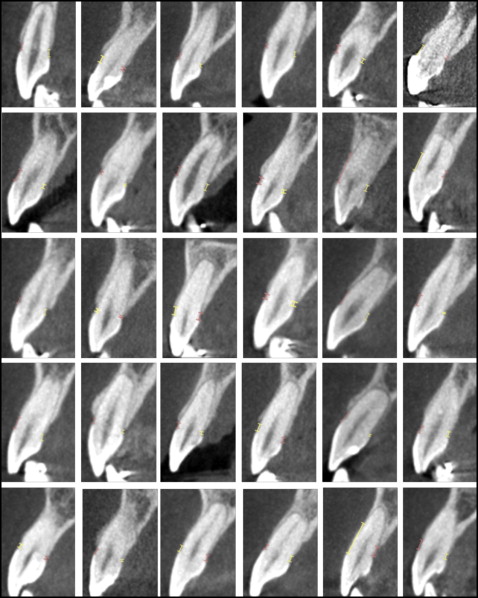
The buccal and lingual alveolar crest heights were measured on cross sections passing through the center of the crowns of the C3, NC3, and NC2, with the cementoenamel junction (CEJ) as a reference ( Fig 3 ).
Statistical analysis
Teeth were measured twice with an interval of at least 1 month by 2 examiners (M.S.Y., D.G.G.). Intrarater and interrater reliabilities were assessed with intraclass correlation coefficients.
Normal distribution was evaluated with the Kolmogorov-Smirnov test ( P <0.05). Intergroup comparisons were performed using the paired t test when there was normal distribution or the Wilcoxon test when there was nonnormal distribution ( P <0.05).
Results
Alveolar bone thickness measurements showed excellent intrarater correlations of 0.91 to 1.00. The alveolar crest level assessments demonstrated good intrarater correlations of 0.7 to 0.89.
Intergroup comparisons are shown in the Table . The canines’ buccal bone in the cleft area was thinner than that of the controls, and the lingual bone thickness was similar ( Table and Fig 4 ).
| C3 mean (SD) | NC3 mean (SD) | P | C3 mean (SD) | NC2 mean (SD) | P | |
|---|---|---|---|---|---|---|
| BABT | 0.20 (0.34) | 0.45 (0.47) | 0.002 ∗ | 0.20 (0.34) | 0.53 (0.54) | 0.001 ∗ |
| LABT | 1.39 (1.11) | 1.44 (0.93) | 0.738 | 1.39 (1.11) | 1.48 (0.82) | 0.556 |
| BACH | 2.58 (1.67) | 1.95 (0.78) | 0.050 | 2.58 (1.67) | 2.06 (1.23) | 0.378 |
| LACH | 1.87 (1.63) | 1.38 (0.67) | 0.094 | 1.87 (1.63) | 1.02 (0.51) | 0.000 ∗ |
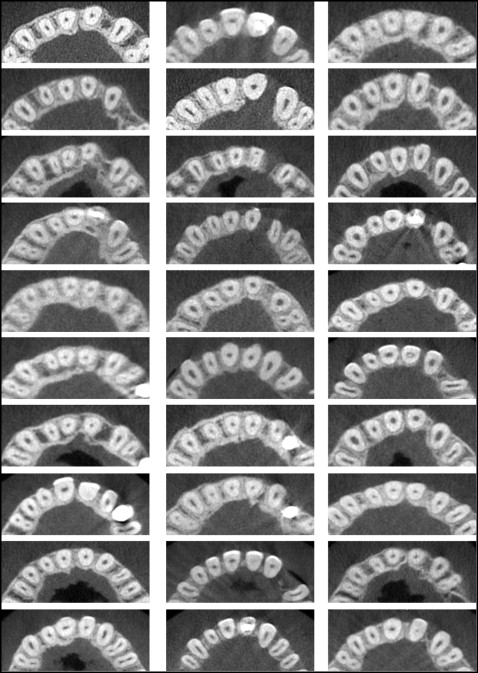
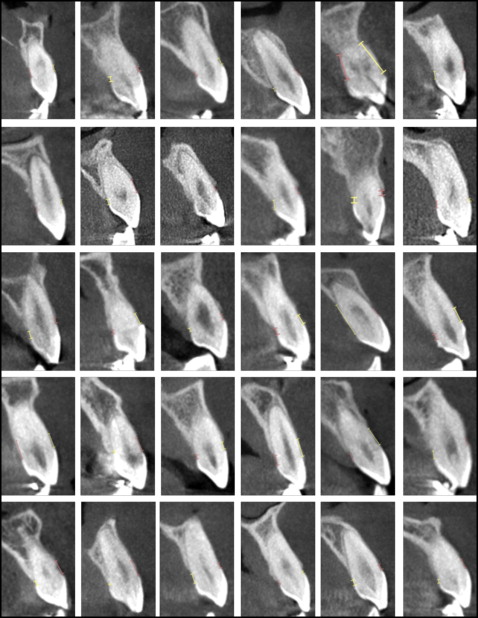
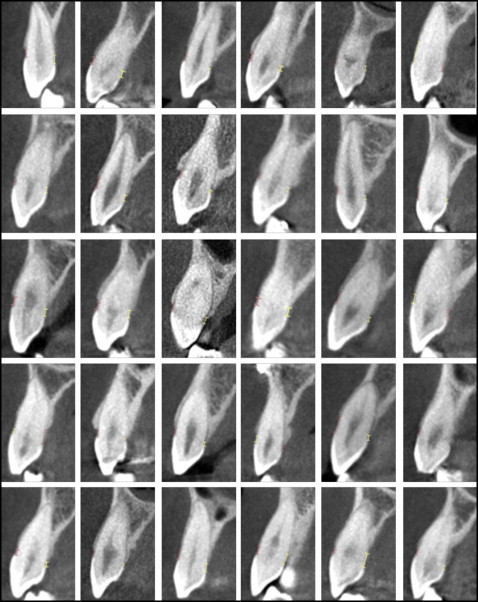
Cross-sectional images of the experimental and control teeth from the complete sample are shown in Figures 5, 6 , and 7 . Despite the large individual variations ( Fig 5 ), the buccal alveolar crest level of the maxillary canines moved into the grafted alveolar cleft was similar to that of the contralateral teeth ( Table ). In the whole sample, only 1 patient showed severe buccal bone dehiscence, and 6 patients had moderate buccal bone dehiscences. The lingual alveolar crest height of the C3 was similar to the control canines but more apically located than were the NC2 ( Table ). Two of the 30 patients showed severe lingual bone dehiscences, and 1 patient had moderate lingual bone dehiscence.
Results
Alveolar bone thickness measurements showed excellent intrarater correlations of 0.91 to 1.00. The alveolar crest level assessments demonstrated good intrarater correlations of 0.7 to 0.89.
Intergroup comparisons are shown in the Table . The canines’ buccal bone in the cleft area was thinner than that of the controls, and the lingual bone thickness was similar ( Table and Fig 4 ).



